Translate this page into:
Evolution of verrucous hemangioma
Correspondence Address:
Mirjana Popadic
Dermatovenereologist, MD, MSc Work address: Pasterova 2, Belgrade, Serbia
| How to cite this article: Popadic M. Evolution of verrucous hemangioma. Indian J Dermatol Venereol Leprol 2012;78:520 |
Sir,
This is a case report of verrucous hemangioma (VH)in a female child, and it is an exclusive report of its evolution seen during the follow-up period.
A 14-year-old, Caucasian girl was referred to Dermatology Clinic for the evaluation of congenital, pigmented lesion on her right leg. Trauma of the lesion caused the patient to seek medical advice for the first time at this stage of lesion.
The initial clinical examination in June 2009 revealed solitary, purplish-brown, plaque with moderately rough surface [Figure - 1]. The main dermoscopic feature of the entire lesion, was the alveolar appearance, numerous small, oval and polygonal elements surrounded by slightly darker pigmentation and mildly presented sulci [Figure - 2]. Purplish-brown color was the predominant pigmentation. Typical lacunae of varying dimensions were found on the lower half of the lesion margin.
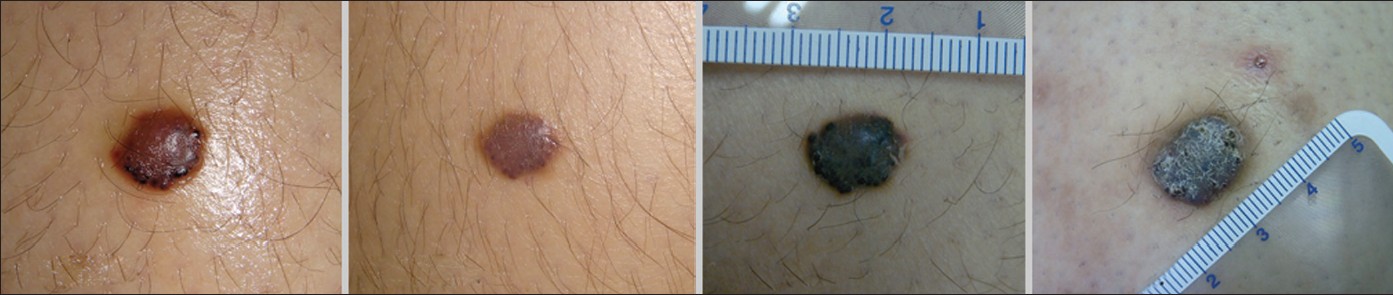 |
| Figure 1: Side-by-side comparison of the baseline and follow-up digital clinical images. Significant changes include increase in size, darkening and development of hyperkeratotic surface (Sony DSC T 700 digital photo-camera) |
 |
| Figure 2: Side-by-side comparison of the baseline and follow-up digital dermoscopic images. Significant changes include pronounced alveolar appearance with more prominent sulci, dominance of dark-bluish pigmentation and increasing number and size of the surrounding lacunae (Dermlite photo 37, 3GEN mounted on the Nikon coolpix 4500 digital photo camera) |
The initial follow-up examination in September 2009 revealed a significant regression of the lesion. Clinically, well-circumscribed purple plaque, with flat and smooth upper surface, was present [Figure - 1] with dermoscopically alveolar appearance, purple-bluish pigmentation and disappearance of the lacunae [Figure - 1].
Nevertheless, after 3 months at the second follow-up control in December 2009, morphologic appearance and dermoscopic features of the lesion were significantly changed.
Clinically, the lesion enlarged and become dark bluish-black, raised nodule, with irregular borders and hyperkeratotic surface [Figure - 1]. Dermoscopic examination revealed more marked alveolar appearance, with more pronounced sulci [Figure - 2]. The dominance of blue color was the following striking feature with different shadows of the light blue, indigo blue and dark bluish-black color. Darker, bluish-black and black lacunae were present mainly at the periphery, partially surrounding the lesion.
Histologically, the lesion was characterized by hyperplastic epidermis, showing hyperkeratosis and irregular acanthosis [Figure - 3]. The underlying dermis was occupied by numerous dilated vessels, some located between lengthened dermal papillae. Numerous smaller vessels, mainly capillary-type, were extending below them in the reticular dermis.
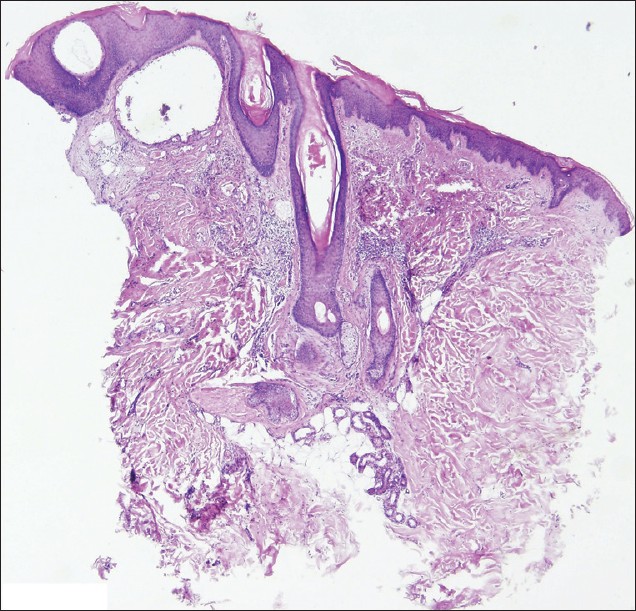 |
| Figure 3: Histopathology (4 mm punch biopsy specimen) showing the hyperkeratosis, irregular acanthosis and numerous, heavily dilated papillary vessels in underlying dermis as well as numerous dilated capillary-type vessels in reticular dermis (H and E ×100) |
Verrucous hemangioma (VH) is a rare, congenital vascular tumor, initially appearing as reddish macular area of vascular staining, resembling the "port-wine" stain. Although almost invariably present at birth, VH may appear later, even in adult age. [1] After a variable number of years and recurrent episodes of bleeding and infection, it begins to take on its characteristic bluish-black color and an increasingly verrucous surface and become bluish-black, verrucous and hyperkeratotic plaques, nodules or bands. Lesions are single or grouped, and may have a linear or serpiginous arrangement or may occur in a more disseminated distribution, without evidence of the systemic lesions. [1] Small satellite lesions are commonly present. The size of VH may vary from 4 mm to 8 cm in diameter. In a large majority of cases (95%), the VH occurs unilaterally on the lower extremities of children. [2]
The term "verrucous hemangioma" was first used by Halter in 1937, but as a distinct entity, it was first described by Imperial and Helwig in 1967, defined it as congenital vascular malformation, comprising the capillary or cavernous hemangioma in the dermis and subcutaneous tissue, associated with the reactive epidermal acanthosis, papillomatosis, and hyperkeratosis, distinguishing it from angiokeratoma. [3]
The subtle distinction, deeper extension of VH than angiokeratoma into the reticular dermis and subcutaneous adipose tissue, has serious implications for treatment, as VH requires a deeper excision to prevent persistence of the lesion.
In this report, the clinical, dermoscopic and histopathological features of VH in 14-year-old girl were described. To the best of my knowledge, it is the first review of evolution of VH documented by images.
| 1. |
Atherton DJ, Moss C. Naevi and other developmental defects. In: Textbook of Dermatology, In: Burns DA, Breathnach S, Cox N, Griffiths C, editors. 7th ed. Oxford: Blackwell Science; 2004.p.15-60.
[Google Scholar]
|
| 2. |
Clairwood QM, Bruckner LA, Dadras SS. Verrucous hemangioma: a report of two cases and review of the literature. J Cutan Pathol 2011;38:740-6.
[Google Scholar]
|
| 3. |
Imperial R, Helwig EB. Verrucous hemangioma. A clinicopathologic study of 21 cases. Arch Dermatol 1967;96:247-53.
[Google Scholar]
|
Fulltext Views
2,793
PDF downloads
2,314





