Translate this page into:
Excision of basal cell carcinomas smaller than 1 cm with 2 mm safety margins: Lateral margin adequacy evaluated by double-bladed scalpel method
2 Department of Pathology, Botucatu Medical School, São Paulo State University (Unesp), SP, Brazil
Correspondence Address:
Juliano Vilaverde Schmitt
Department of Dermatology and Radiotherapy, Botucatu Medical School, Universidade Estadual Paulista, Av. Prof. Mario Rubens Guimaraes Montenegro, S/N, Distr. Rubiao Jr, Botucatu, 18618.687, SP
Brazil
| How to cite this article: Haddad GR, Miot HA, Alencar Marques ME, Schmitt JV. Excision of basal cell carcinomas smaller than 1 cm with 2 mm safety margins: Lateral margin adequacy evaluated by double-bladed scalpel method. Indian J Dermatol Venereol Leprol 2018;84:603-606 |
Sir,
The most frequent safety margins recommended in the literature for excision of basal cell carcinomas range from 3 to 4 mm. On the contrary, for small, well-defined, pigmented lesions and for lesions located in more cosmetic and sensitive areas (such as periorbital), the feasibility of more conservative treatments and narrower safety margins aided by dermoscopy is advocated.[1],[2]
As an option for the evaluation of lateral surgical margins, the use of a double-bladed scalpel has been described, with the removal of skin strips which are then assessed lengthwise in histological sections.[3]
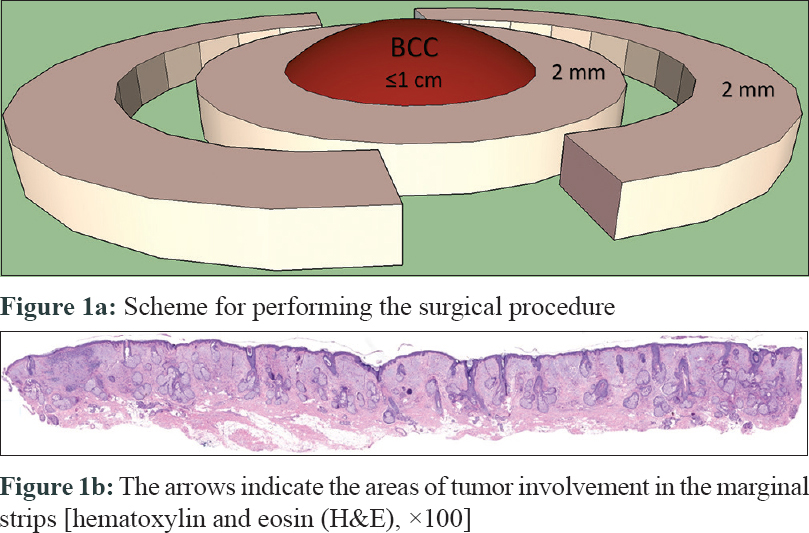
The double-bladed scalpel consisted of a lightweight holder with two parallel blade sockets at the tip with a 2 mm interblade gap, allowing the execution of two simultaneous parallel uniform lines of incision, facilitating the attainment of marginal tissue strips, by producing two concentric regular incisions at the same depth. The resulting ring of tissue can be delineated and easily excised using a scalpel or a scissor [Figure - 1] and [Figure - 2].
 |
| Figure 1: |
 |
| Figure 2: |
A cross-sectional study was carried out, consisting of patients with excised, well-defined, nonrelapsed, <1 cm in diameter basal cell carcinomas, using a 2 mm safety margin, with removal of marginal skin strips in addition [Figure - 1] and [Figure - 2].
Margins of 2 mm were demarcated using a surgical ruler aided by dermoscopy and the excision was performed with a 2 mm-wide double-bladed scalpel, with the inner blade aligned with the margin mark of 2 mm. All tumors were removed at the subcutaneous level, and surgical defects were subjected to primary closure.
Tumors and strips margins were dyed, embedded in paraffin and stained in hematoxylin and eosin. The marginal strips were assembled so that the microtome sections were processed from the inner to the outer face of the margins in order to ensure greater similarity to the margins analyzed in the central part by the cross-cut technique [Figure - 1]. All initial sections of the paraffin block containing marginal strip tissue were analyzed.
The study was approved by the Ethics Committee of the institution and the participants signed a consent form.
[Table - 1] and [Table - 2] summarize the information about the participants and the lesions. All central parts of the excised strips presented free surgical margins in the cross-cut evaluation. Three marginal strips (5.8%) proved to be compromised, with clinical relapse in one lesion (33.3%) after a 12-month follow-up [Table - 3] and [Figure - 3].



 |
| Figure 3: (a) Histological sections of tumors (H&E, ×100) (lesion n1 of Table 3) (b) Compromised marginal strips. The arrow indicates the areas of tumor involvement in the marginal strips (H&E, ×100). (lesion n1 of Table 3) (c) Histological sections of tumors (H&E, ×100) (lesion n2 of Table 3) (d) Compromised marginal strips. The arrow indicates the areas of tumor involvement in the marginal strips (H&E, ×100) (lesion n2 of Table 3) (e) Histological sections of tumors (H&E, ×100) (lesion n3 of Table 3) (f) Compromised marginal strips. The arrows indicate the areas of tumor involvement in the marginal strips (H&E, ×100) (lesion n3 of Table 3) |
After a median follow-up of 15 [12–22] months, there was no local relapse in any of the tumors with free marginal strips. There was no difference regarding the diameter (6 [6-6] × 6 (4-7); P = 0.46) of the lesions with and without compromised strips, but none of the 24 lesions up to 5 mm in diameter had their strips compromised, as compared to 3/28 (10.7%) of the lesions with 6–10 mm in diameter (P = 0.24).
As for the location, 2/3 (66.7%) of the compromised strips occurred on the head or neck, against 35/49 (71.4%) of noncompromised strips (P = 0.99).
The study of narrower margins of excision for basal cell carcinomas is interesting, mainly for low-risk lesions as more conservative treatments have better acceptability in patients. Illustratively, the change from a 2-mm to a 4-mm surgical margin for a basal cell carcinoma of 6-mm in diameter increases the area of excised tissue by almost 100%. This difference may be significant in cosmetic areas such as the face and in patients with several previous skin cancer surgeries.
The use of lateral skin stripping technique added sensitivity to the identification of compromised margins. With a 2-mm margin, according to the assessment of the lateral margins of the strips, there is an involvement of margins of 5.8% (confidence interval of 95%: 0–11.5% – “bootstrap method”), but in conventional cuts, there was no compromise of the margins.
In a review of literature including 16,066 basal cell carcinomas, Gulleth et al. observed a 15–18% variation in the compromise of margins in conventional histological examination and local relapse rates between 4 and 1.6%, with 2- to 4-mm safety margins. Unlike the present study, the mean diameter of the lesions was 11.7 mm, varying from 3 to 30 mm, with no restrictions regarding clinical pattern or histological subtype. In this study, they concluded that safety margins of 3 mm would be reasonable for basal cell carcinomas up to 2 cm in diameter.[4]
Griffiths et al. (2007) verified lesions incompletely excised peripherally in 6.1% of 1539 basal cell carcinomas excised by conventional surgery. Again, they did not report restrictions regarding lesion size or histological subtype; however, 70% of tumors had peripheral histological margins narrower than 5 mm.[5]
On the contrary, Caresana and Giardini identified only three compromised margins in 200 basal cell carcinomas (1.5%) removed with a 2-mm safety margin aided by dermoscopy. Similarly, Ito et al. found only 4.3% tumor-positive margins in 46 pigmented basal cell carcinomas excised with 2-mm or less surgical margins.[1],[2]
Our data present results similar to the studies of Caresana and Giardini and Ito et al., indicating lateral tumor-positive margins of around 5% or less for well-demarcated basal cell carcinomas. On the contrary, Kimyai-Asadi et al. found higher rate (24%) of tumor-positive margins for small (<1 cm), well-demarcated lesions. These differences could be explained by the surgical techniques used, the aid of dermoscopy and the lesion profile, because we had 35% of pigmented tumors and 38% of lesions located on nonfacial regions.[1],[2],[6]
Our study had limitations including low number of specimens studied and a possible reduction of external validity because the identification of well-defined and solid tumors, as well as the demarcation of their borders, depended on the evaluator. Other limitation could be irregular correlation between marginal strip and central part margins analysis; however, all initial sections with marginal strip tissue were analyzed.
To conclude, in this study, the excision of well-delineated basal cell carcinoma lesions of up to 1 cm in diameter with a 2-mm safety margin aided by dermoscopy presents a lateral compromise rate of 5.8% when evaluated by marginal strip technique, reinforcing the results of some previous studies and suggesting the feasibility of narrower lateral surgical margins for small (<1 cm), well-demarcated basal cell carcinomas.
Acknowledgement
The authors would like to thank the Support Fund for Dermatology of São Paulo State – Sebastião Sampaio (FUNADERSP) for supporting the study.
Financial support and sponsorship
Support Fund for Dermatology of São Paulo State – Sebastião Sampaio (FUNADERSP).
Conflicts of interest
There are no conflicts of interest.
| 1. |
Ito T, Inatomi Y, Nagae K, Nakano-Nakamura M, Nakahara T, Furue M, et al. Narrow-margin excision is a safe, reliable treatment for well-defined, primary pigmented basal cell carcinoma: An analysis of 288 lesions in Japan. J Eur Acad Dermatol Venereol 2015;29:1828-31.
[Google Scholar]
|
| 2. |
Caresana G, Giardini R. Dermoscopy-guided surgery in basal cell carcinoma. J Eur Acad Dermatol Venereol 2010;24:1395-9.
[Google Scholar]
|
| 3. |
Aoyagi S, Hata H, Homma E, Shimizu H. Controlling the histological margin for non-melanoma skin cancer conveniently using a double-bladed scalpel. J Surg Oncol 2010;101:175-9.
[Google Scholar]
|
| 4. |
Gulleth Y, Goldberg N, Silverman RP, Gastman BR. What is the best surgical margin for a basal cell carcinoma: A meta-analysis of the literature. Plast Reconstr Surg 2010;126:1222-31.
[Google Scholar]
|
| 5. |
Griffiths RW, Suvarna SK, Stone J. Basal cell carcinoma histological clearance margins: An analysis of 1539 conventionally excised tumours. Wider still and deeper? J Plast Reconstr Aesthet Surg 2007;60:41-7.
[Google Scholar]
|
| 6. |
Kimyai-Asadi A, Alam M, Goldberg LH, Peterson SR, Silapunt S, Jih MH, et al. Efficacy of narrow-margin excision of well-demarcated primary facial basal cell carcinomas. J Am Acad Dermatol 2005;53:464-8.
[Google Scholar]
|
Fulltext Views
4,170
PDF downloads
5,625





