Translate this page into:
Exogenous ochronosis
Correspondence Address:
Sathish B Pai
Department of Dermatology, Kasturba Medical College and Hospital, Manipal University, Manipal - 576 104, Karnataka
India
| How to cite this article: Jain A, Pai SB, Shenoi SD. Exogenous ochronosis. Indian J Dermatol Venereol Leprol 2013;79:522-523 |
A 45-year-old male, presented with hyperpigmentation on face with history of photo aggravation, since 10 years. History of treatment with triple combination de-pigmenting agents for melasma was present, with no improvement in hyperpigmentation over the last 7 years. On examination, black colored macules were present over the nose, malar area, forehead; earlobes sparing the eyelids, and naso-labial fold [Figure - 1]. Confetti-like de-pigmentation and hyperchromic, pin-point, caviar-like papules and telengectasias were seen on the lateral aspect of nose [Figure - 2]. Neither follicular plugging nor discoid rash was seen. ANA (Antinuclear antibody) global result was moderately positive with granular pattern. Skin biopsy from malar area showed moderately strong basement membrane zone (BMZ) band of IgG on direct immunofluorescence (DIF). Histopathology showed yellow-brown ochronotic pigment, deposited within collagen bundles causing homogenization and swelling of the bundles [Figure - 3]. Focal periadnexal and perivascular lymphoplasmacytic infiltrates were seen. There were no features of discoid lupus erythematosus (DLE). Based on clinical features and histopathology a diagnosis of exogenous ochronosis was made.
 |
| Figure 1: Hyperpigmented macules on face |
 |
| Figure 2: Close-up view of nose showing caviar-like papules |
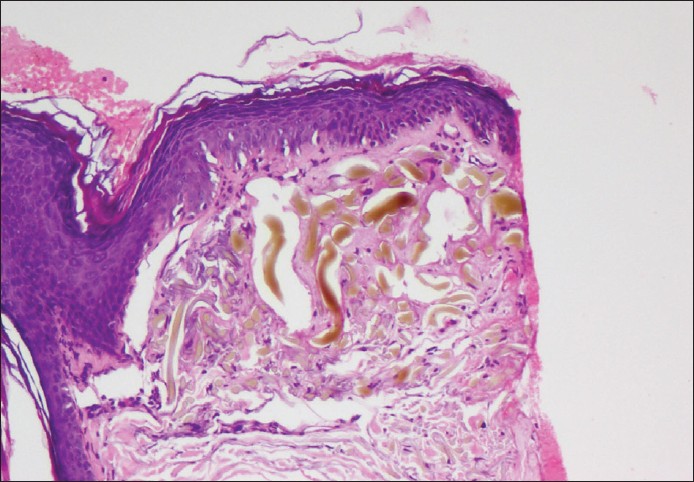 |
| Figure 3: Yellow-brown ochronotic pigment in collagen bundles in the dermis (H and E, × 100) |
Exogenous ochronosis was first described by Beddard and Plumtrein (1912) in a patient following the use of phenol for leg ulcer. Topical application of hydroquinone (1975 by Findlay), phenol, resorcinol, oral anti-malarials have been implicated too. Inhibition of homogentisic oxidase and accumulation of homogentisic acid which polymerizes to form ochre (brownish-yellow) pigment in the papillary dermis is the proposed mechanism. This condition is exclusively seen in high photo type. Three clinical stages are - erythema and mild hyperpigmentation; Hyperpigmentation and pigmented colloid milium (caviar-like lesions) with scanty atrophy and last stage with papulo-nodular lesions. Histopathology in exogenous ochronosis shows pigment incontinence, solar elastosis, ochre pigment, ′banana-shaped′ fibers in papillary dermis, and eventually degeneration of the collagen; colloid milium and/or granulomas. In Indian population, DLE can present as macular hyperpigmentation. In DLE, immune deposits are characteristically seen along the BMZ with IgG being more specific and three immunoreactants being significant; patterns of fluorescence can be linear, granular, and shaggy. 60-94% of biopsy from lesional skin is positive for DIF in DLE. Facial hyperpigmentation not responding to long term treatment with bleaching agents should be dealt with high index of suspicion for exogenous ochronosis. An early diagnosis necessitates immediate discontinuation of hydroquinone, rather than increasing the concentration in attempt to clear the dermatosis. Exogenous ochronosis is often missed clinically and also under reported. In view of under diagnosis, the condition is being reported. Satisfactory results have been described with retinoic acid, dermabrasion, cryotherapy, CO2, laser, Q-switched Ruby laser, and Q-switched Alexandrite 755 laser. In the present case, histopathological findings were not suggestive of DLE. IgG deposits and ANA global positivity may not be significant in this patient, but a close follow-up is necessary to see if he develops features of connective tissue disease. DLE was ruled out by histopathology and immunofluorescence showed only IgG deposits. There should be more than two positive immunoreactants in DIF to confirm the diagnosis of DLE. Patient is being treated with broad-spectrum sunscreen and topical 6% glycolic acid and counseled for Erbium: YAG (Yttrium aluminium garnet) pixel laser.
Fulltext Views
16,503
PDF downloads
2,994





