Translate this page into:
Expression of Ber-EP4 and CD34 can distinguish clear-cell basal cell carcinoma from trichilemmoma: A case series
Corresponding author: Dr. Schulman, VA Mather, 10535 Hospital Way, Building #650, Pathology, Mather, CA 95655. Joshua.Schulman@va.gov
-
Received: ,
Accepted: ,
How to cite this article: Mitra A, Schulman JM. Expression of Ber-EP4 and CD34 can distinguish clear-cell basal cell carcinoma from trichilemmoma: A case series. Indian J Dermatol Venereol Leprol. 2024;90:118-20. doi: 10.25259/IJDVL_468_2022
Dear Editor,
Basal cell carcinoma is one of the most common diagnoses encountered in the daily practice of dermatopathology across the globe. Though they are usually diagnosed readily based on conventional histopathologic features, some may present a diagnostic challenge, especially when tumour cells exhibit uncommon cytomorphologic characteristics. One such example is the clear-cell variant of basal cell carcinoma, in which the cytoplasm of tumour cells appears vacuolated or empty, occasionally with displacement of the nucleus to the periphery leading to a signet-ring morphology. The differential diagnosis of clear-cell basal cell carcinoma includes neoplasms with trichilemmal, sebaceous and eccrine or apocrine differentiation, as well as clear-cell variants of squamous cell carcinoma, melanoma and metastatic renal cell carcinoma. In particular, differentiating clear-cell basal cell carcinoma from trichilemmoma may be difficult, as both entities share clinical features and, histopathologically, can demonstrate a lobular growth pattern, peripheral palisading, epidermal connection and surface ulceration. These entities can also demonstrate varying proportions of basaloid to clear or pale-staining tumour cells. Despite these similarities, distinction between these diagnoses is usually straightforward on routinely stained sections when areas of conventional basal cell carcinoma or prototypical trichilemmoma are also present. However, for biopsy specimens which are small, superficial, fragmented, or affected by technical artifact, accurate diagnosis may require additional studies such as immunohistochemistry.
The use of immunohistochemical staining to distinguish clear-cell basal cell carcinoma from trichilemmoma has not previously been explored in a systematic manner considering the rarity of these cases. Herein, we are presenting a case series consisting of five cases of clear-cell basal cell carcinoma and investigate the utility of immunohistochemical staining with CD34 and Ber-EP4 to differentiate these tumours from trichilemmomas. Ber-EP4 and CD34 are well-established immunohistochemical stains for basal cell carcinoma and trichilemmoma, respectively, but the staining pattern in the former has not been established previously.
All study material was from routine diagnostic cases. We selected basal cell carcinoma cases that included at least focal areas of conventional basal cell carcinoma for the reviewing dermatopathologist to establish an unequivocal diagnosis for each case. Formalin-fixed paraffin-embedded sections from all the cases (five cases of clear-cell basal cell carcinoma and seven cases of trichilemmomas) were stained with haematoxylin and eosin (H&E) and stained for CD34 (Roche Diagnostics, Clone: QBEnd/10) and Ep-CAM (Sigma Aldrich, Clone: Ber-Ep4). The H&E and immunohistochemical findings were analysed by both authors, one of whom is a board-certified dermatopathologist .
Haematoxylin and eosin: Histopathologically, our cases of basal cell carcinoma demonstrate a range of clear-cell changes, with some examples mostly resembling conventional basal cell carcinoma with only focal areas of clear-cell change, and others demonstrating almost exclusively clear-cell cytomorphology with only rare areas of conventional basaloid tumour. The transition between conventional and clear-cell areas within a given tumour may be gradual or abrupt. Usually, basal cell carcinoma shows at least focally peritumoural clefting, and the tumour-associated stroma is greyish and loose. In contrast, trichilemmoma does not show peritumoural clefting, and the tumour-associated stroma is more eosinophilic. Figure 1 illustrates all five cases of clear-cell basal cell carcinoma.
Immunohistochemical staining: All five cases of basal cell carcinoma showed partial to diffuse membranous staining with Ber-EP4 [Figures 1a–1e]. The Ber-EP4 staining was strongly positive in the conventional basal cell carcinoma regions and stained the clear-cell areas in variable fashion, often with more intense staining near the periphery of tumour lobules. The clear-cell areas showed no staining for CD34 in four out of five cases [Figure 1, right column] and focal membranous staining in one case [Figure 1d]. Peritumoural endothelial cells and fibroblasts stained with CD34 served as internal controls. All seven cases of trichilemmoma showed membranous staining with CD34 and were negative for Ber-EP4 expression [Figure 2].
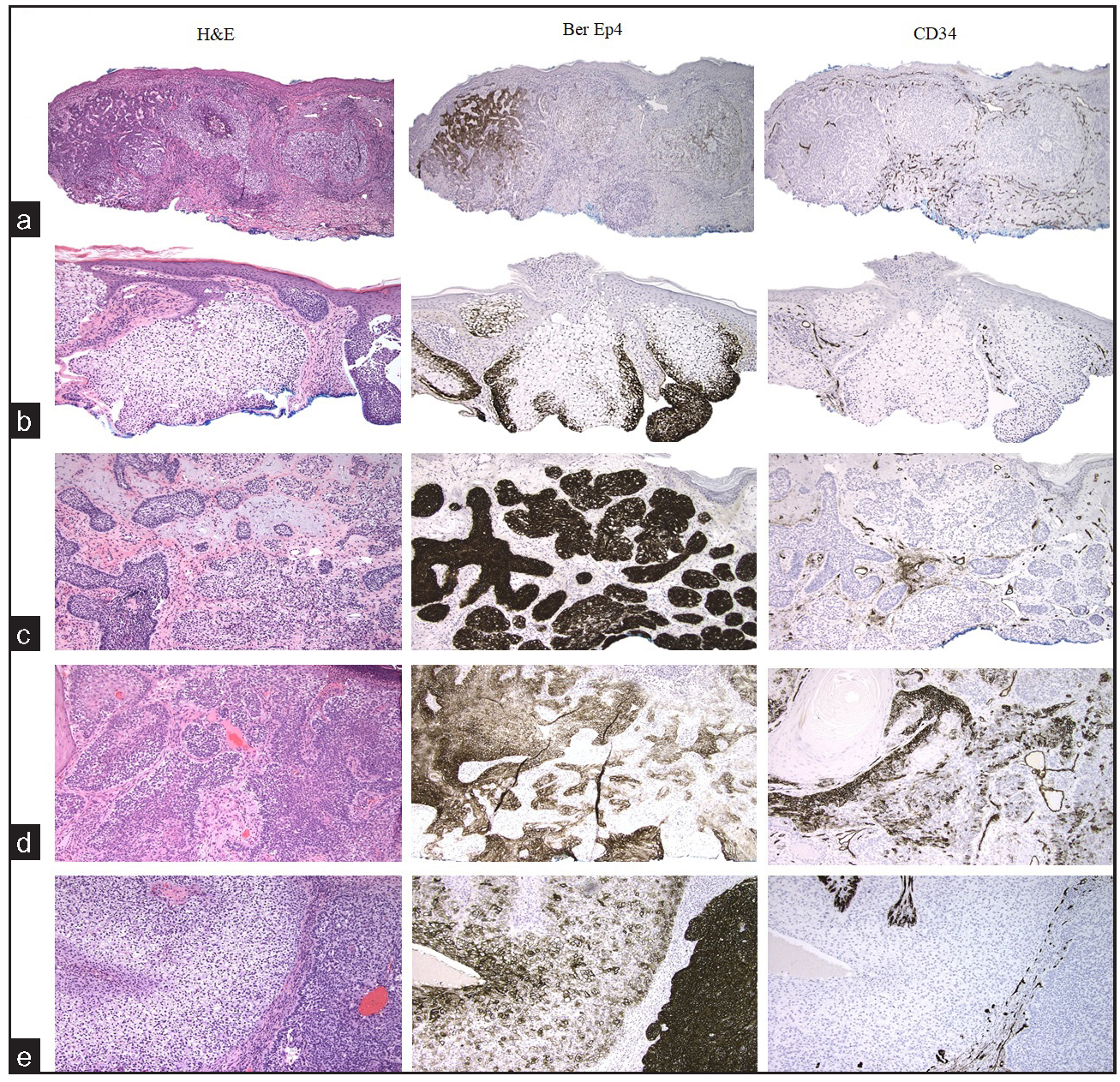
- Haematoxylin and eosin (H&E) and immunohistochemical stains of 5 cases of clear-cell basal cell carcinoma. Each row represents one case of clear-cell basal cell carcinoma; cases are serially designated as a–e. The left column H&E, middle and right columns represent Ber-EP4 and CD34 immunostaining of the same case respectively. (a) Case1, conventional basal cell carcinoma transitions to clear-cell basal cell carcinoma from left to right on H&E. Ber-EP4 staining is strongly positive in areas with conventional BCC and weaker in areas with clear-cell change. CD34 is negative in tumour cells. (b) Case 2, clear-cell basal cell carcinoma emanates from the epidermal undersurface with conventional basal cell carcinoma at the right edge of the H&E field. Ber-EP4 staining highlights the peripheral aspects of the clear-cell areas. CD34 is negative in tumour cells. (c) Case 3, conventional basal cell carcinoma is present predominantly in the left side of the image with clear-cell changes in the lower-central part of the image. Ber-EP4 staining is strongly positive. CD34 is negative in the tumour cells. (d) Case 4, Conventional basal cell carcinoma features predominate with admixed clear-cell areas at the periphery of tumour lobules and beneath the epidermal surface. Ber-EP4 expression is positive throughout. CD34 is focally positive in the tumour cells in a membranous fashion. (e) Case 5, clear-cell basal cell carcinoma is present on the left half of the image with conventional basal cell carcinoma at the right. Ber-EP4 strongly highlights the conventional basal cell carcinoma with patchier staining in the clear-cell area. CD34 staining is negative in the tumour cells. (100x)
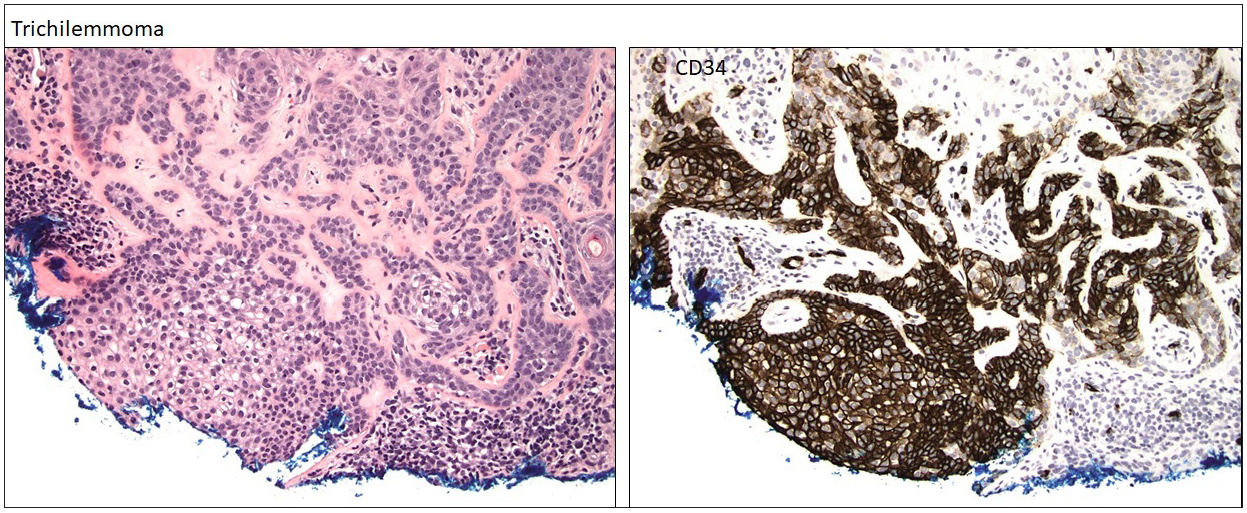
- H&E and CD34 immunohistochemistry stains of one representative case of trichilemmoma. The tumour cells show strong membranous CD34 staining (100x)
Clear-cell basal cell carcinoma, first described in 1984, is an uncommon variant of basal cell carcinoma that has likely been under-reported in the literature.1 There are only 32 cases of clear-cell basal cell carcinoma reported so far. Attempts to characterise these tumours based on glycogen content, sialomucin deposition, and ultrastructural findings have yielded often conflicting results, and the precise pathogenesis of the clear-cell change remains a topic of inquiry.2–9
Trichilemmomas are benign adnexal tumours and can be clinical and histopathologic mimickers of basal cell carcinoma. The use of CD34 and Ber-EP4 immunostaining to distinguish between basal cell carcinoma and trichilemmoma has been explored previously, notably by Turnbull et al.,10 who examined the utility of these stains in differentiating basaloid trichilemmomas from conventional basal cell carcinomas. Their report confirmed that trichilemmomas, both basaloid and those with clear-cell change, exhibit positive CD34 and negative Ber-EP4 staining, while the opposite result was seen in conventional basal cell carcinomas.
The related question of whether these immunostains can distinguish between conventional trichilemmomas and clear-cell basal cell carcinomas has previously been addressed in a much more limited fashion. In a study of basal cell carcinomas with thickened basement membrane, El-Shabrawi and LeBoit11 described only two cases of clear-cell basal cell carcinoma, with CD34 positivity identified in only one of the two cases. These results are inconclusive given the small sample size of the two cases. As CD34 generally stains the keratinocytes of the outer root sheath, the authors propose that trichilemmal differentiation must not necessarily be a feature of clear-cell basal cell carcinoma. Larger studies comparing clear-cell basal cell carcinoma with trichilemmoma have not been reported previously.
Thus, we focused on a relatively larger cohort of five cases of clear-cell basal cell carcinoma and seven cases of trichilemmoma and stained them with CD34 and Ber-EP4. In four out of five cases of clear-cell basal cell carcinoma, CD34 expression was entirely absent in the tumour aggregates, and in the remaining one case, membranous CD34 expression was identified focally. Thus, in most cases of clear-cell basal cell carcinoma, trichilemmal differentiation is not observed. All five cases of clear-cell basal cell carcinoma exhibit Ber-EP4 positivity. In contrast, all seven cases of trichilemmoma showed membranous CD34 positivity but were negative for Ber-EP4.
Our results show that CD34 and Ber-EP4 immunostaining can successfully distinguish clear-cell basal cell carcinoma from trichilemmoma, and these two immunostains can be used to differentiate these two entities in challenging situations. Our results confirm the observation that clear-cell change in basal cell carcinoma does not necessarily reflect trichilemmal differentiation.
Authors contributions
In this manuscript, both, Anupam Mitra and Joshua Schulman, contributed to the design, definition of intellectual content, literature search, experimental studies, data acquisition, data analysis, manuscript preparation, and manuscript editing and review, and Joshua Schulman contributed to the concepts of the study.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Clear cell basal cell carcinoma. Patholog Res Int 2011:386921.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clear cell basal cell epithelioma: Light and electron microscopic study of an unusual variant. J Cutan Pathol. 1988;15:1-7.
- [CrossRef] [PubMed] [Google Scholar]
- Clear cell basal cell carcinoma with sialomucin deposition. Yonsei Med J. 2006;47:870-2.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clear cell basal carcinoma: An unusual variant. Histopathology. 1996;29:390-1.
- [CrossRef] [PubMed] [Google Scholar]
- Clear-cell basal cell carcinoma: Differentiation from other clear-cell tumors. Am J Dermatopathol. 2007;29:208-9.
- [CrossRef] [PubMed] [Google Scholar]
- Clear cell basal cell carcinoma. Histopathology. 1990;17:401-5.
- [CrossRef] [PubMed] [Google Scholar]
- Clear-cell, basal cell carcinoma: Histopathological, histochemical, and electron microscopic findings. J Cutan Pathol. 1988;15:404-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clear cell basal cell carcinoma: An unusual degenerative variant. J Cutan Pathol. 1993;20:308-16.
- [CrossRef] [PubMed] [Google Scholar]
- CD34 and BerEP4 are helpful to distinguish basaloid tricholemmoma from basal cell carcinoma. Am J Dermatopathol. 2018;40:561-6.
- [CrossRef] [PubMed] [Google Scholar]
- Basal cell carcinoma with thickened basement membrane: A variant that resembles some benign adnexal neoplasms. Am J Dermatopathol. 1997;19:568-74.
- [CrossRef] [PubMed] [Google Scholar]






