Translate this page into:
Expression of CD117 and platelet-derived growth factor receptor α in patients with alopecia areata
2 Department of Pathology, Indira Gandhi Medical College and Research Institute, Puducherry, India
Correspondence Address:
Saritha Mohanan
Department of Dermatology, Indira Gandhi Medical College and Research Institute, Puducherry
India
| How to cite this article: Mohanan S, Sylvia MT, Carounanidy U, Bhat RV. Expression of CD117 and platelet-derived growth factor receptor α in patients with alopecia areata. Indian J Dermatol Venereol Leprol 2020;86:643-648 |
Abstract
Background: Alopecia areata is a disease of uncertain, probably autoimmune etiology. The role of growth factors like platelet-derived growth factor and C-kit (CD117) in alopecia areata is unknown.
Aims: To compare the expression of CD117 and platelet-derived growth factor receptor α in tissue samples of alopecia areata and normal controls.
Methods: Thirty biopsy samples of alopecia areata and eighteen normal control samples were included in this cross-sectional study. Immunohistochemistry was done to detect the expression of CD117 and platelet-derived growth factor receptor α in cases and controls. The mean percentage of follicles expressing CD117 and platelet-derived growth factor receptor α was compared among cases and controls.
Results: The mean number of follicles expressing CD117 in anagen and catagen hairs differed significantly among cases and controls. The extent and intensity of staining with platelet-derived growth factor receptor α correlated significantly with the severity of alopecia areata based on the severity of alopecia tool score.
Limitations: Confirmation of the expression pattern of molecules observed in immunohistochemistry with western blot or polymerase chain reaction would have strengthened the report.
Conclusions: The expression of CD117 varied in cases and controls. The expression of platelet-derived growth factor receptor α correlated with the severity of the disease. This could explain how platelet-rich plasma works in the treatment of alopecia areata. Further studies are required to explore the role of these molecules in autoimmune pathogenesis.
Introduction
Alopecia areata is an acquired inflammatory disease characterized by circumscribed patches of hair loss due to premature truncation of the anagen or growth phase of hair.[1] Although the exact etiology is unknown, the most accepted theory is the autoimmune theory due to its association with autoimmune disorders, the collection of T-lymphocytes in the affected tissue and the response to immunosuppressive agents.[2],[3] In view of the varied therapeutic strategies used in the treatment, other unknown factors may also play a role in the pathogenesis. Platelet-rich plasma is one of the newer therapies used in alopecia areata, and it possibly acts via the release of growth factors into the affected tissue.[4]
Many different growth factors play a role in the development and cycling of the hair follicle through epidermal-mesenchyme interactions.[5] It has been shown that isoforms of platelet-derived growth factor and its receptor (platelet-derived growth factor receptor α) play a role in hair follicle development and embryogenesis.[6],[7],[8] C-kit (CD117) is known to be essential for melanocyte migration during development and its expression has been found in the outer root sheath of hair follicles. Ashrafuzzaman et al. have demonstrated increased CD117 expression in the affected areas in alopecia areata and androgenetic alopecia.[9]
However, the exact role of these molecules in the autoimmune disease process is unknown. Hence, this study was planned to compare the expression of CD117 and platelet-derived growth factor receptor α in patients with alopecia areata and normal controls to investigate their possible role in the disease pathogenesis.
Methods
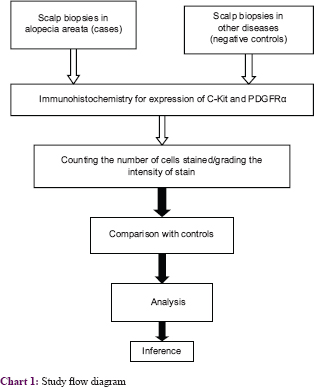
The study was designed as a cross-sectional study [chart 1]. After obtaining the approval from the Institutional Ethics Committee, the study was conducted in the Departments of Dermatology and Pathology in Indira Gandhi Medical College and Research Institute, Puducherry. Thirty consecutive patients of alopecia areata, clinically diagnosed by two independent dermatologists were recruited as cases. Patients on tyrosine kinase inhibitors or antihistamines were excluded from the study. After noting the demographic parameters, the severity of alopecia tool score was calculated for all patients. Poliosis was not seen in any of the patients. After obtaining informed consent, a punch biopsy was taken from the margin of the patch including normal skin to look for disease activity at the margin. Scalp biopsy material from biopsies done for other scalp conditions as well as by-products from scalp surgeries were taken as controls, as it was easier than subjecting patients to another biopsy wound. A total of 18 controls were included. As it was the first study (proof of concept) on immunohistochemistry of platelet-derived growth factor receptor α in alopecia areata, a convenience sample size of cases and controls was taken.
Immunohistochemistry
Horizontal and vertical sections were taken from the biopsies received. The histopathological parameters were studied. Immunohistochemistry was done as per standard protocol. The antibody used to identify CD 117 was rabbit monoclonal, clone EP10 (PathnSitu biotechnologies Pvt Ltd). For identifying platelet-derived growth factor receptor α, rabbit polyclonal antibodies (Thermo Scientific) were used. The slides were washed and counterstained with hematoxylin, cleared and mounted.
Analysis
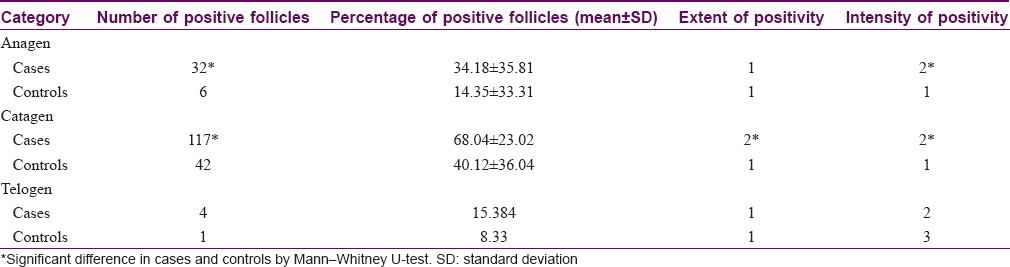
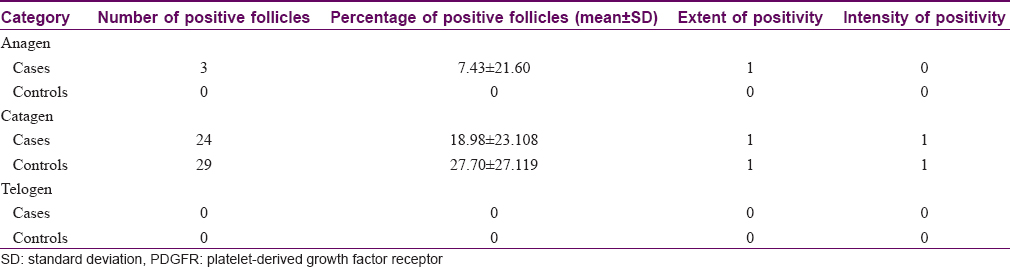
The percentage of anagen, catagen and telogen follicles showing positivity for CD117 and platelet-derived growth factor receptor α were calculated in each case and control and the means of the percentage of positive hair follicles were calculated. To increase objectivity of reporting, the staining was rated by extent (0 = no staining; 1 = 1%–24%; 2 = 25%–49%; 3 = 50%–74% and 4 = 75%–100%) of the cell population of interest per high power field and by the intensity of staining (1+, weak; 2+, moderate and 3+, strong). All the cells in the outer root sheath in all the follicles of each section were considered and the median scores were determined. The medians of the extent of staining and the intensity of staining among anagen, catagen and telogen follicles were estimated in each case and control. The pathologist was not blinded to cases and control slides.
Statistical analysis
The mean percentage of anagen and catagen follicles showing positivity for C-kit and platelet-derived growth factor receptor α were compared using the Mann-Whitney U test. The medians of the extent of staining and intensity of staining in the follicles between cases and controls were compared using the Mann-Whitney U test. The correlation between severity of alopecia tool score and staining scores and that between the duration of lesions and the staining scores was analyzed using Pearson's correlation test.
Results
We included thirty cases of alopecia areata and eighteen normal scalp control samples. The mean age of the patients was 31.2 ± 8.42 years. The average duration of illness in the patients was 15.71 weeks (interquartile range 4–12). One patient had comorbid hypertension. Two patients had atopy. Six patients had received previous treatment, four of them with topical steroids. There was no washout period before sampling as it was not considered prudent to stop treatment when no other intervention was planned. Three patients had ophiasis pattern while the rest had patchy hair loss. The severity of alopecia tool score ranged from 3 to 86. Histopathologically, the average follicular units in cases were 7.83 units (range 3–16). The average number of hair follicles in the controls was 18 (range 6–36). The average terminal vellus hair ratio was 1: 2 in the cases and 7:1 in the controls. Miniaturized hair follicles were present in ten cases (33%). Fibrous stellae were seen in fourteen (46%) and “swarm of bees” appearance in 23 (76%) cases.
All the cases had an expression of CD117 in catagen hair follicles [Figure - 1]a, whereas 12 (40%) cases were negative for CD117 in anagen hair follicles. Among controls, 12(66.6%) expressed positivity for CD117 in catagen hair follicles and only 4 expressed positivity for CD 117 in anagen hair follicles. Among catagen follicles, the difference in the mean percentage of follicles expressing CD 117 among cases and controls was statistically significant (P = 0.014) [Table - 1]. The difference in the mean number of follicles expressing CD117 in anagen hair among cases [Figure - 1]b and controls [Figure - 1]c was also statistically significant (P = 0.022). Among telogen follicles, only 4 follicles expressed CD117 among cases and one follicle was positive among controls. In both cases and controls, CD117 was expressed in the isthmus and infundibulum, the mesenchyme, eccrine and sebaceous glands. However, 11 cases also showed positivity in the outer root sheath. The difference in the extent of cells stained among cases and controls was statistically significant in catagen (P = 0.00) hair follicles. The difference in the intensity of staining in the anagen (P = 0.035) and catagen hair follicles (P = 0.01) was also significantly different among cases and controls.
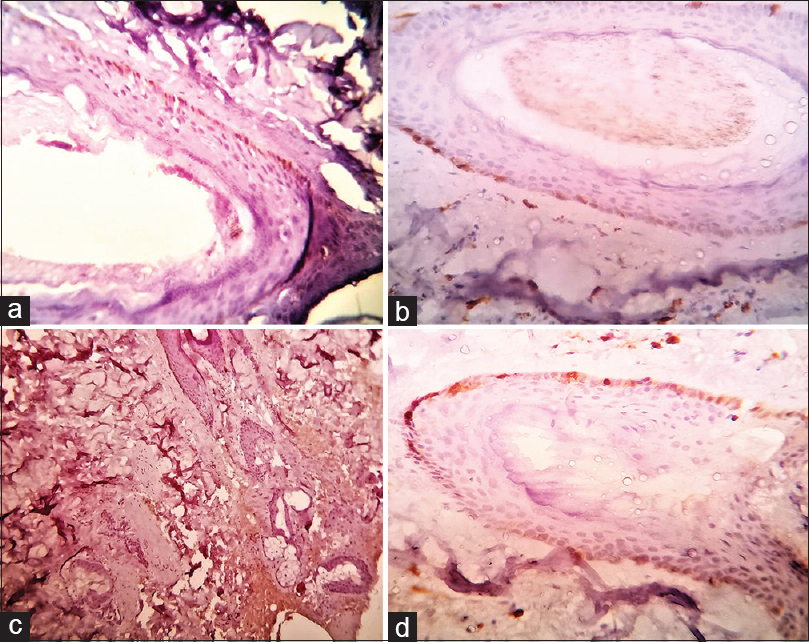 |
| Figure 1: Alopecia areata. Immunohistochemistry showing expression of CD117 (C-kit): (a) in the catagen hair follicle with the intensity of 1+ in 30% of cells (IHC, ×400); (b) in the anagen hair follicle with an intensity of 3+ in 5% of cells (IHC, ×400); (c) platelet-derived growth factor receptor α in the catagen hair follicle with the intensity of 1+ in 10% of cells (IHC, ×400). (d) Control. Immunohistochemistry showing lack of expression of CD117 (IHC, ×400) |
Platelet-derived growth factor receptor α was predominantly positive in catagen hair follicles [Figure - 1]d. The pattern of expression was similar to CD 117 with positivity in the outermost layer of the outer root sheath of the hair follicles, isthmus, infundibulum and in the inner root sheath and surrounding the bulb in a few cases. It was not expressed in the dermis, eccrine or sebaceous glands. Thirteen cases showed no expression of platelet-derived growth factor receptor α in catagen hair follicles while 6 controls were negative. Only 4 cases expressed positive anagen hair follicles. All the controls displayed negative anagen and telogen hair follicles. The difference in the mean number of anagen and catagen hair follicles expressing platelet-derived growth factor receptor α was not significant [Table - 2]. None of the cases or controls exhibited positivity for platelet-derived growth factor receptor α in telogen hair follicles. The differences in the extent of staining and the intensity of staining in anagen and catagen hair follicles among cases and controls was not statistically significant.
There was a significant correlation between the severity of alopecia tool score and the intensity of staining with platelet-derived growth factor receptor α in catagen follicles in the cases (R 0.419, P = 0.021). There was also a significant correlation between the severity of alopecia tool score and both the extent (R 0.507, P = 0.004) and the intensity of staining (R 0.599, P = 0.00) with platelet-derived growth factor receptor α in anagen follicles in cases [Figure - 2]. There was no correlation between the severity of alopecia tool score and the extent or intensity of staining with CD117 in both anagen and catagen follicles in cases. There was no correlation between the duration of lesions in the cases and the mean percentage of positive anagen and catagen follicles for CD117 and platelet-derived growth factor receptor α. There was no correlation between the duration of lesions and the extent and intensity of staining except for the intensity of platelet-derived growth factor receptor α in catagen hair follicles (R 0.37, P = 0.042). The difference in staining of CD117 and platelet-derived growth factor receptor α according to the type of alopecia areata and comorbid conditions could not be analyzed as only 3 patients had ophiasis type and comorbid conditions.
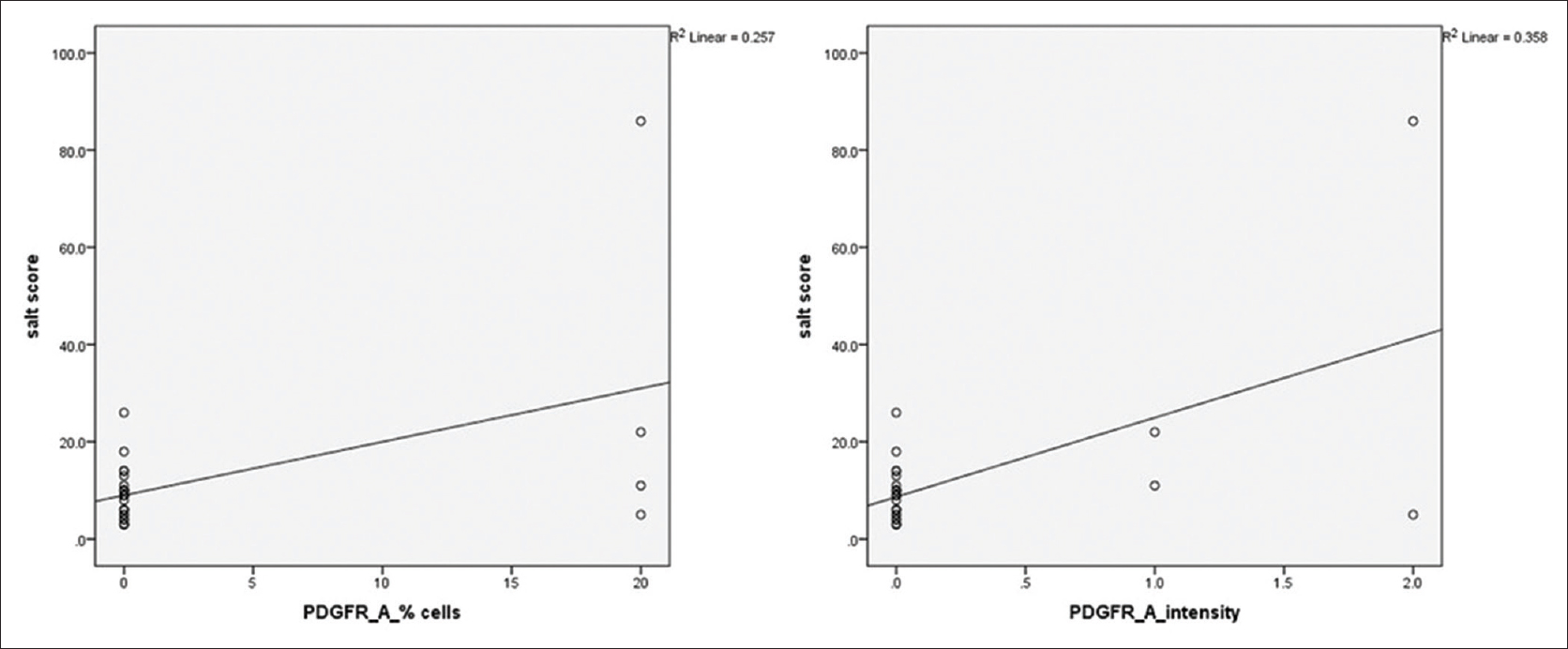 |
| Figure 2: Scatter plots showing the correlation of severity of alopecia tool score with the extent (left) and intensity (right) of expression of platelet-derived growth factor receptor α in anagen hair follicles in patients with alopecia areata |
Discussion
Alopecia areata is a distressing problem of hair loss with a great psychological burden to patients. It is associated with various other potentially disabling diseases such as atopic dermatitis, diabetes mellitus, autoimmune thyroiditis with which it could share many pathogenetic mechanisms. In that sense, alopecia areata serves as one of the models to study autoimmunity. Growth factors, among other factors, are presumed to play a role in the autoimmune pathogenesis of alopecia areata.
Many growth factors play a role in hair cycling and embryogenesis, through epidermal mesenchymal interactions. We studied and compared the expression of CD117 and platelet-derived growth factor receptor α in a series of alopecia areata specimens and normal scalp controls. Platelet-derived growth factor is secreted by platelets and other cells and acts via a tyrosine kinase signalling pathway. The exact role of platelet-derived growth factor in hair follicle development and hair follicle cycling is yet unknown and there have been conflicting reports about its role.
A role for platelet-derived growth factor-alpha (PDGF-A) in hair follicle development has been substantiated by injection of platelet-derived growth factor receptor α antibodies into new-born mice which perturbed hair formation.[8] Epithelial platelet-derived growth factor is said to activate mesenchymal platelet-derived growth factor receptor α which in combination with sonic hedgehog signalling activates Noggin secretion by mesenchymal (dermal) cells. This is reported to rescue stalled epithelial Wnt signalling which is a pivotal pathway in hair growth.[10] Platelet-derived growth factor plays a role in the induction and maintenance of murine anagen follicles.[11] Platelet-derived growth factor has also been shown to be important in hair canal formation during embryogenesis.[11] A recent study proposes that platelet-derived growth factor signalling is essential to maintain the hair follicle dermal stem cell pool and their regenerative capacity.[12] Conversely, other studies described that PDGF-A stimulated the growth of cultured rat fibroblasts but not rat vibrissae dermal papilla cells and that was consistent with a higher expression of platelet-derived growth factor receptor α in fibroblasts than in dermal papilla cells.[13] Another study has found that platelet-derived growth factor signalling is dispensable in hair follicle induction and formation.[5],[14] With this conflicting evidence in the background, we decided to study the expression of platelet-derived growth factor receptor α in alopecia areata and normal samples to look for a possible role of growth factors in the pathogenesis of alopecia.
Our study found no significant difference in the mean number of follicles expressing platelet-derived growth factor receptor α between cases of alopecia areata and controls. However, we found a significant correlation between the severity of alopecia tool score and the intensity of staining with platelet-derived growth factor receptor α in the catagen and anagen follicles. In catagen, expression of platelet-derived growth factor may be reduced causing increased expression of platelet-derived growth factor receptor α in follicles. It has been demonstrated that there is a significant down-regulatory effect by catagen-inducing cytokines like interleukin-1 (IL-1) beta or gamma-interferon (IFN-γ) on the expression of platelet-derived growth factor in hair follicle keratinocytes and dermal papilla cells, suggesting a possible involvement of platelet-derived growth factor signalling in the induction of catagen.[7] Correlation of this expression of platelet-derived growth factor receptor α with the severity of the disease indicates that platelet-derived growth factor may have a possible role in the premature truncation of anagen. This could explain the beneficial effect of platelet-rich plasma in alopecia areata.[4] One of the methods by which platelet-rich plasma is said to act is by increasing the AKT (Protein Kinase B) and ERK (extracellular-signal-regulated kinase) signalling pathway.[15] Curiously, platelet-derived growth factor also induces Akt phosphorylation. This suggests a pathway by which platelet-derived growth factor and platelet-rich plasma acts in alopecia areata.
There was a significant difference in the expression of CD117 in anagen and catagen follicles among cases and controls. Ashrafuzzaman et al. also demonstrated increased expression of CD117 in alopecia areata and androgenetic alopecia.[9] They proposed that this could be due to feedback due to low levels of stem cell factor or C-kit ligand in the surrounding tissue. Catagen inducing cytokines like IFN γ could reduce expression of stem cell factor, thereby increasing the expression of CD117 in catagen follicles. Patients on imatinib, a CD117 and platelet-derived growth factor inhibitor, have been reported to develop depigmentation and alopecia.[16] Histopathological examination of skin lesions induced by imatinib has shown perifollicular fibrosis, implicating a possible role for CD117 or platelet-derived growth factor or both in the pathogenesis of alopecia, as imatinib is a tyrosine kinase inhibitor with CD117 and platelet-derived growth factor receptor among its biological targets.[17]
It is not known what role these molecules play in the autoimmune etiology of alopecia areata. CD117 has been shown to confer protection against autoimmunity in mice.[1] Thus, anti-PDGF antibodies have been implicated in systemic sclerosis. The reduction in the severity of autoimmune nephritis in mice caused by calorie restriction is said to be associated with reduced expression of PDGF-A.[19] Further, research could unveil more mechanisms by which these molecules play a role in autoimmune disorders, particularly alopecia areata.
It would be interesting to review any therapeutic implications of the involvement of growth factors in the pathogenesis of the disease. Antihistamines have anecdotally been reported to be useful in alopecia areata, especially in alopecia areata associated with atopic dermatitis.[20] Increased perifollicular mast cell accumulation has been observed in alopecia areata. Antihistamines like fexofenadine reduce the production of IFN-γ and reduce expression of intercellular adhesion molecule -1 (ICAM-1). Cetirizine has been touted as a novel weapon against autoimmune disorders.[21] Topical becaplermin or rhPDGF-BB promotes the inflammatory phase of the wound healing process in healthy and healing-impaired animal models probably by promoting chemotaxis of neutrophils, monocytes and smooth muscle cells in wounds.[22] Any role of becaplermin in the treatment of alopecia areata has to be considered with the view that it promotes inflammation, although dermal injection of platelet derived growth factor-AA or platelet-derived growth factor-BB in mice triggers resting hair follicles to enter the hair growth cycle.[23]
The expression pattern of CD117 and platelet-derived growth factor receptor α in immunohistochemistry in our study could not be confirmed by western blot or real-time-polymerase chain reaction which would have enhanced the value of our results. Further, the research could shed more light on the role of these growth factors in autoimmunity in general and in alopecia areata, specifically. This could, in future, open new avenues of management, not only in alopecia areata but also in other autoimmune disorders.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity but anonymity cannot be guaranteed.
Financial support and sponsorship
Indian Association of Dermatology, Venereology and Leprology-L'oreal research grant.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Wasserman D, Guzman-Sanchez DA, Scott K, McMichael A. Alopecia areata. Int J Dermatol 2007;46:121-31.
[Google Scholar]
|
| 2. |
McElwee KJ, Hoffmann R. Alopecia areata – Animal models. Clin Exp Dermatol 2002;27:410-7.
[Google Scholar]
|
| 3. |
Hordinsky M, Ericson M. Autoimmunity: Alopecia areata. J Investig Dermatol Symp Proc 2004;9:73-8.
[Google Scholar]
|
| 4. |
Trink A, Sorbellini E, Bezzola P, Rodella L, Rezzani R, Ramot Y, et al. A randomized, double-blind, placebo- and active-controlled, half-head study to evaluate the effects of platelet-rich plasma on alopecia areata. Br J Dermatol 2013;169:690-4.
[Google Scholar]
|
| 5. |
Akiyama M, Smith LT, Holbrook KA. Growth factor and growth factor receptor localization in the hair follicle bulge and associated tissue in human fetus. J Invest Dermatol 1996;106:391-6.
[Google Scholar]
|
| 6. |
Karlsson L, Bondjers C, Betsholtz C. Roles for PDGF-A and sonic hedgehog in development of mesenchymal components of the hair follicle. Development 1999;126:2611-21.
[Google Scholar]
|
| 7. |
Kamp H, Geilen CC, Sommer C, Blume-Peytavi U. Regulation of PDGF and PDGF receptor in cultured dermal papilla cells and follicular keratinocytes of the human hair follicle. Exp Dermatol 2003;12:662-72.
[Google Scholar]
|
| 8. |
Takakura N, Yoshida H, Kunisada T, Nishikawa S, Nishikawa SI. Involvement of platelet-derived growth factor receptor-alpha in hair canal formation. J Invest Dermatol 1996;107:770-7.
[Google Scholar]
|
| 9. |
Ashrafuzzaman M, Yamamoto T, Shibata N, Hirayama TT, Kobayashi M. Potential involvement of the stem cell factor receptor C-kit in alopecia areata and androgenetic alopecia: Histopathological, immunohistochemical, and semiquantitative investigations. Acta Histochem Cytochem 2010;43:9-17.
[Google Scholar]
|
| 10. |
Rishikaysh P, Dev K, Diaz D, Qureshi WM, Filip S, Mokry J. Signaling involved in hair follicle morphogenesis and development. Int J Mol Sci 2014;15:1647-70.
[Google Scholar]
|
| 11. |
Tomita Y, Akiyama M, Shimizu H. PDGF isoforms induce and maintain anagen phase of murine hair follicles. J Dermatol Sci 2006;43:105-15.
[Google Scholar]
|
| 12. |
González R, Moffatt G, Hagner A, Sinha S, Shin W, Rahmani W, et al. Platelet-derived growth factor signaling modulates adult hair follicle dermal stem cell maintenance and self-renewal. NPJ Regen Med 2017;2:11.
[Google Scholar]
|
| 13. |
Yu D, Cao Q, He Z, Sun TT. Expression profiles of tyrosine kinases in cultured follicular papilla cells versus dermal fibroblasts. J Invest Dermatol 2004;123:283-90.
[Google Scholar]
|
| 14. |
Rezza A, Sennett R, Tanguy M, Clavel C, Rendl M. PDGF signalling in the dermis and in dermal condensates is dispensable for hair follicle induction and formation. Exp Dermatol 2015;24:468-70.
[Google Scholar]
|
| 15. |
Arshdeep., Kumaran MS. Platelet-rich plasma in dermatology: Boon or a bane? Indian J Dermatol Venereol Leprol 2014;80:5-14.
[Google Scholar]
|
| 16. |
Vinay K, Yanamandra U, Dogra S, Handa S, Suri V, Kumari S, et al. Long-term mucocutaneous adverse effects of imatinib in Indian chronic myeloid leukemia patients. Int J Dermatol 2018;57:332-8.
[Google Scholar]
|
| 17. |
Llamas-Velasco M, Fraga J, Kutzner H, Steegmann JL, García-Diez A, Requena L. Hypopigmented macules secondary to imatinib for the treatment of chronic myeloid leukemia: A histopathologic and immunohistochemical study. J Cutan Pathol 2014;41:417-26.
[Google Scholar]
|
| 18. |
Li H, Nourbakhsh B, Safavi F, Li K, Xu H, Cullimore M, et al. Kit (W-SH) mice develop earlier and more severe experimental autoimmune encephalomyelitis due to absence of immune suppression. J Immunol 2011;187:274-82.
[Google Scholar]
|
| 19. |
Troyer DA, Chandrasekar B, Barnes JL, Fernandes G. Calorie restriction decreases platelet-derived growth factor (PDGF)-A and thrombin receptor mRNA expression in autoimmune murine lupus nephritis. Clin Exp Immunol 1997;108:58-62.
[Google Scholar]
|
| 20. |
Atanaskova Mesinkovska N. Emerging Unconventional Therapies for Alopecia Areata. J Investig Dermatol Symp Proc 2018;19:S32-3.
[Google Scholar]
|
| 21. |
Namazi MR. Cetirizine and allopurinol as novel weapons against cellular autoimmune disorders. Int Immunopharmacol 2004;4:349-53.
[Google Scholar]
|
| 22. |
Nagai MK, Embil JM. Becaplermin: Recombinant platelet derived growth factor, a new treatment for healing diabetic foot ulcers. Expert Opin Biol Ther 2002;2:211-8.
[Google Scholar]
|
| 23. |
Andrae J, Gallini R, Betsholtz C. Role of platelet-derived growth factors in physiology and medicine. Genes Dev 2008;22:1276-312.
[Google Scholar]
|
Fulltext Views
4,368
PDF downloads
1,646





