Translate this page into:
Extensive keloidal healing of pemphigus vulgaris
Correspondence Address:
Neena Khanna
Department of Dermatology and Venereology and Department of Pathology, All India Institute of Medical Sciences, New Delhi -110 029
India
| How to cite this article: Khanna N, Rathi S, Shantharaman R, Gupta S D. Extensive keloidal healing of pemphigus vulgaris. Indian J Dermatol Venereol Leprol 1997;63:199-200 |
Abstract
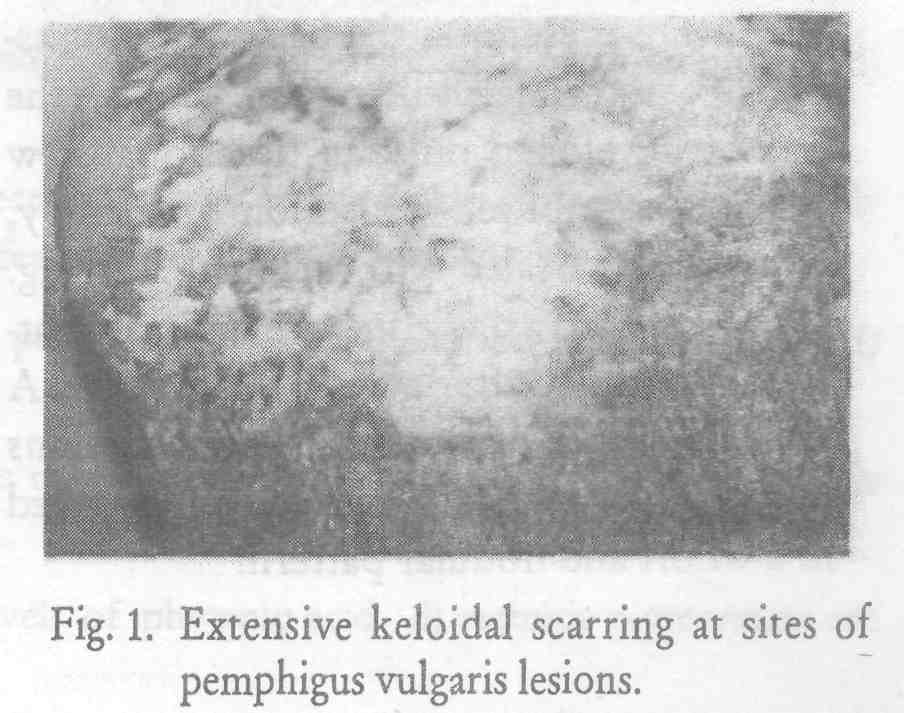
Bullae of pemphigus vulgaris heal without scarring. We here report a patient of pemphigus vulgaris whose lesions healed with a one-month history of extensive flaccid bullae and uninfected erosions on the trunk and extremities along with superficial erosions in the oral mucosa. The clinical suspicion of pemphigus vulgaris was confirmed by histopathological and immunohistological examination. Pulse therapy with monthly parenteral dexamethasone and cyclophosphamide pulse was instituted. The cutaneous lesions on healing formed extensive keloidal scars despite high dose of monthly corticosteroid therapy.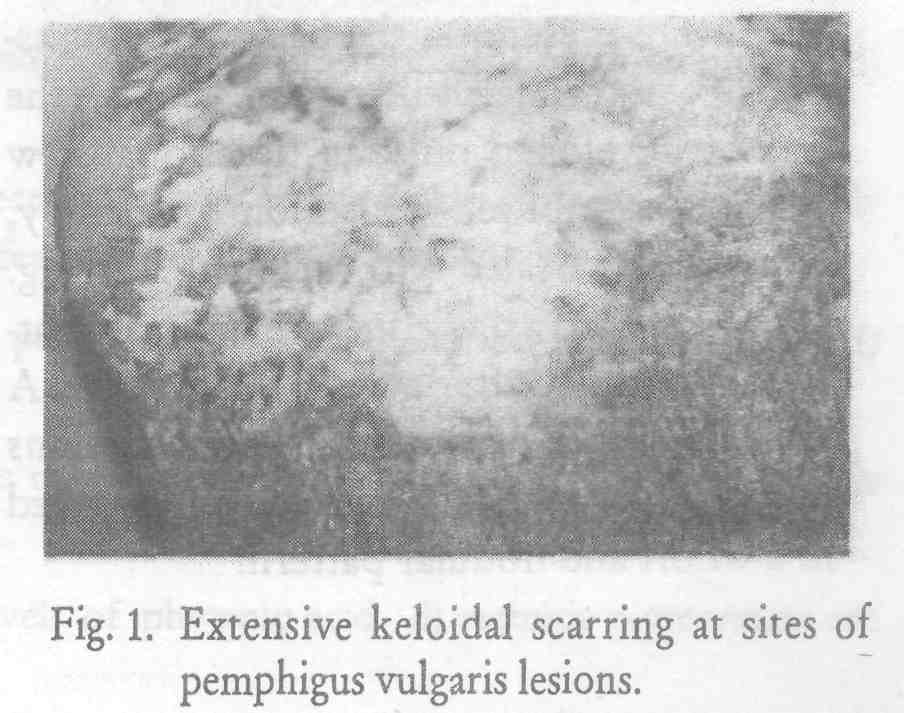 |
 |
Pemphigus vulgaris is the commonest immunological bullous disorder we see in our practice. Skin lesions generally heal without scarring. Transient hyperpigmentation commonly present at the site of healed lesions usually resolves with time.[1] We report a patient of pemphigus vulgaris whose uninfected skin lesions healed with extensive keloidal scarring despite high dose corticosteroid pulse therapy. This phenomenon has, to the best of our knowledge, not been described earlier.
Case Report
A 50-year-old farmer presented with a one month history of extensive bullous lesions involving the trunk and extremities. He also complained of oral ulcers of the same duration. He had received several courses of antibiotics with minimal response. On examination the patient had numerous flaccid bullae on normal looking skin. Extensive areas of denuded skin were present. Nikolsky′s sigh and Asoboe-Hansen sign were positive. Patient also had multiple superficial erosions on the buccal mucosa.
Routine investigations of the patient were within normal limits. Tzanck smear done from the base of an intact bulla was positive for acantholytic cells. Pus culture from a lesion did not reveal growth of any micro-organism. Biopsy from an intact bulla was compatible with diagnosis of pemphigus vulgaris and this was confirmed by direct immunofluorescence studies.
The patient was started on dexamethasone-cyclophosphamide pulse therapy (dexamethasone injection 100 mg for 3 consecutive days and injection cyclophosphamide 500 mg single dose) every month. The patient′s lesions started healing soon after the first dose of pulse therapy. On healing, the lesions formed multiple small keloids and in several areas became confluent forming a reticulate pattern [Figure - 1]. These keloidal lesions were present on the back, anterior aspect of chest, and deltoid region. Though the patient developed only an occasional new bullous lesion after institution of therapy, most lesions healed with keloidal scarring. These scars had a tendency to marginally flatten temporarily after every steroid pulse. A skin biopsy performed on the healed lesions showed compact hyalinised collagen arranged in a whorl and nodular pattern.
Discussion
Pemphigus vulgaris is a blistering disorder in which extensive bullous lesions may be present. The bullae in pemphigus, being intraepidermal, heal without scarring unless there has been secondary bacterial, infection.[1] In our patient the bullous lesions healed, in the absence of secondary infection, with small keloidal scars. The patient did not have a predisposition to keloid formation, nor a similar familial predisposition. He had been put on high doses of corticosteroids within a month of onset of his disease and he developed keloids despite this. Corticosteroids are known to inhibit the activity of enzymes involved in collagen biosynthesis and have been shown to depress collagen synthesis both in-vitro and in fibroblast cultures.[2] Steroids also inhibit the formation of glycosaminoglycans.[3] Therefore, it was surprising that our patient′s lesions healed with keloid formation.
| 1. |
Korman N. Pemphigus, J Am Acad Dermatol 1988;18:1219-1238.
[Google Scholar]
|
| 2. |
Ristel J. Effect of prednisolone on the activities of intracellular enzymes of collagen biosynthesis in rat skin, Bio Chem Pharmacol. 1977;26:1295-1298.
[Google Scholar]
|
| 3. |
Pinnel SR. Regulation of collagen synthesis, J Invest Dermatol 1982;69:73-76.
[Google Scholar]
|





