Translate this page into:
Facial multiple xanthogranuloma in an adult
2 Department of Dermatology, Tianjin Academy of Traditional Chinese Medicine Affiliated Hospital, Tianjin, China
Correspondence Address:
Haixia Guo
Beima Road 354#, Hongqiao District, Tianjin 300120
China
| How to cite this article: Gu A, Guo H, Zhang L, Ma F. Facial multiple xanthogranuloma in an adult. Indian J Dermatol Venereol Leprol 2017;83:696-698 |
Sir,
Xanthogranuloma is a normolipemic non-Langerhans-cell histiocytosis. Though this condition predominantly occurs in infancy and childhood and is also called “juvenile xanthogranuloma”, around 10% of all affected patients are adult. Solitary lesions have been observed in approximately 90% of either juvenile or adult cases.[1],[2] The appearance of multiple lesions is rare in the juvenile form of xanthogranuloma and even rarer in the adult form. Here, we report a case with multiple adult xanthogranulomas who presented with brown, flat wart-like papules on the face.
A 23-year-old man with a 5-year history of brown papules on the face was referred to our dermatology department. Four years ago, he was diagnosed with flat warts and received laser treatments at a local clinic with no response. On examination, there were numerous small light brown papules distributed over the patient's cheeks, root of the nose, temples, and forehead [Figure 1a] and [Figure 1b]. These papules were ill-defined and coalescent, round or irregularly shaped with a shiny surface and size of 0.2 cm to 0.5 cm. [Figure 1c]. These lesions were soft upon palpation and did not exhibit any subjective symptoms. No similar lesion was found on any other part of the patient's body. Ophthalmologic examination of the patient was normal. The patient denied any special exposure, such as fatty food, outdoor work, drugs, radiation, chemicals and so on. No other family member was affected. The laboratory test results, including routine hematological examination, liver and renal function tests, and serum lipid and sugar levels were all normal. Chest and skull radiographs and abdominal ultrasonographic examination revealed no abnormalities. A biopsy was taken from the left temporal region which showed dermal infiltration with histiocytes, lymphocytes, foam cells, and eosinophils [Figure 2a]. Touton giant cells which are multinucleated giant histiocytes with wreath-shaped nuclei and foamy cytoplasm were also seen [Figure 2b]. The infiltrating histiocytes expressed CD68 [Figure 2c] and did not express either S-100 or CD1a, as determined by immunohistochemistry. A final diagnosis of multiple adult xanthogranuloma was made based on the previously mentioned clinical, histopathological, and immunohistochemical findings.
 |
| Figure 1a: Multiple, light brown papules with a shiny surface, measuring 0.2–0.5 cm, present over the entire face - lateral view |
 |
| Figure 1b: Frontal view of lesions |
 |
| Figure 1c: Close-up of lesions over the temporal region |
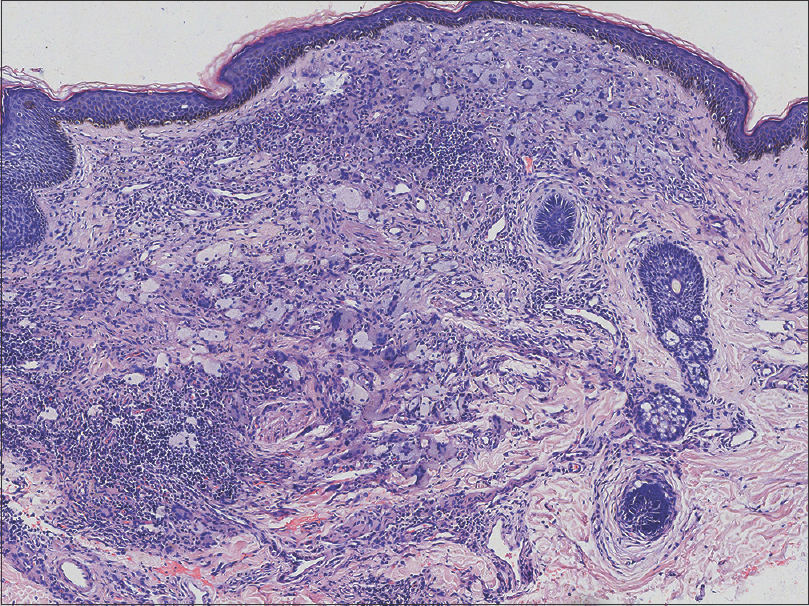 |
| Figure 2a: Mixed infiltration of histiocytes, lymphocytes, foam cells and eosinophils (H and E, ×40) |
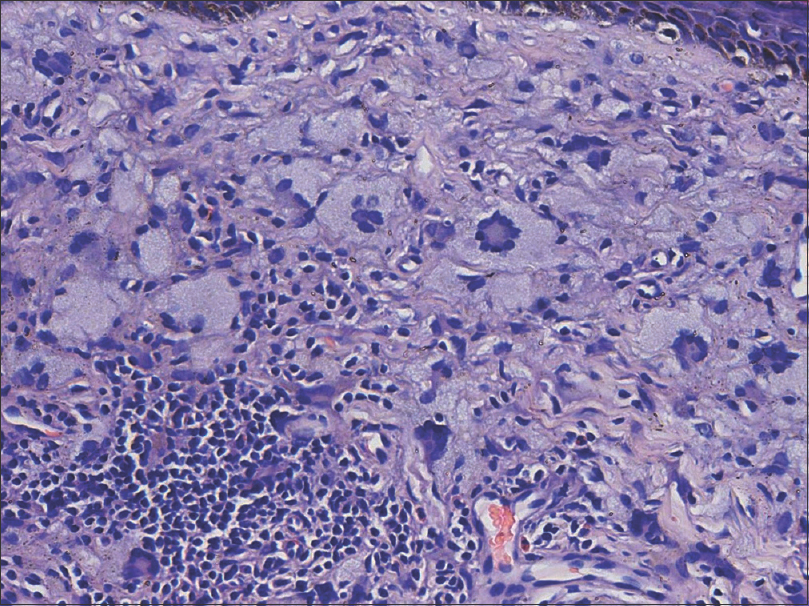 |
| Figure 2b: Touton giant cells - multinucleated giant histiocytes with wreath-shaped nuclei and foamy cytoplasm (H and E, ×200) |
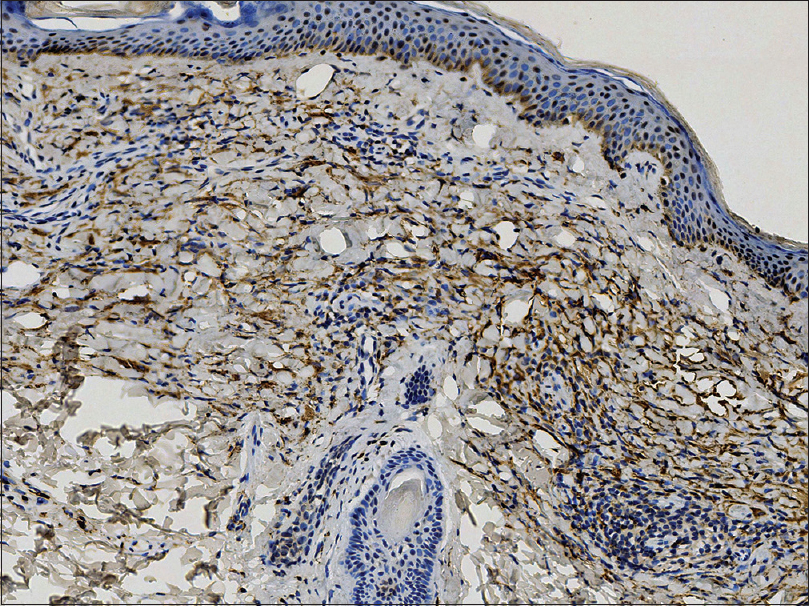 |
| Figure 2c: Positive immunohistochemical staining for CD68 (×100) |
Xanthogranuloma is a benign, self-healing condition which is clinically characterized by one to a few orange or brown papules or nodules commonly located on the upper body, particularly the head and neck.[2],[3],[4] The male-to-female ratio of its incidence is approximately 1.3:1.[3],[4] Approximately 20–30% of juvenile xanthogranuloma cases occur at birth with up to 80% of cases occurring in the first year of life.[1] Only around 10% of xanthogranuloma cases manifest in adulthood, particularly between the late 20s and early 30s.[5] Most of the adult patients have a solitary cutaneous lesion (70–89%).[2] Adult xanthogranuloma presenting with multiple lesions is extremely rare, with only about 20 cases reported since 1963.[1],[2],[6] This condition is defined by the presence of more than five xanthogranuloma lesions in any patient older than 14 years of age.[2],[4] Our patient had a unique clinical presentation with hundreds of xanthogranulomas of an atypical morphology localized only to the face. The initial differential diagnoses considered were flat warts or eruptive syringomas, which were ruled out on histopathologic findings. Other differential diagnoses include generalized eruptive histiocytosis (without Touton giant cells or foam cells), papular xanthoma (with Touton giant cells and foam cells but no inflammatory cells), and xanthoma disseminatum (lesions tend to appear over flexures, have mucous membrane involvement, and associated diabetes insipidus in 40% of the patients). Therefore, based on the presenting symptoms and clinical results, a final diagnosis of multiple adult xanthogranuloma was made. Our case report highlights this rare presentation of xanthogranulomas mimicking other common disorders like flat warts, eruptive syringomas, or xanthomas on the face.
The etiology of xanthogranuloma is unknown. Patients with both the juvenile and adult forms have normal serum lipid profiles.[4] One earlier published report of adult xanthogranuloma did not indicate any spontaneous resolution.[4] However, Saad et al. found that approximately 54% of these cases had a spontaneous resolution.[2] Our patient was advised to remain under regular follow-up the following year because xanthogranuloma is a benign condition and spontaneous regression may occur in some instances.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Nayak S, Acharjya B, Devi B, Patra MK. Multiple xanthogranulomas in an adult. Indian J Dermatol Venereol Leprol 2008;74:67-8.
[Google Scholar]
|
| 2. |
Saad N, Skowron F, Dalle S, Forestier JY, Balme B, Thomas L. Multiple adult xanthogranuloma: Case report and literature review. Dermatology 2006;212:73-6.
[Google Scholar]
|
| 3. |
Dehner LP. Juvenile xanthogranulomas in the first two decades of life: A clinicopathologic study of 174 cases with cutaneous and extracutaneous manifestations. Am J Surg Pathol 2003;27:579-93.
[Google Scholar]
|
| 4. |
Chang SE, Cho S, Choi JC, Choi JH, Sung KJ, Moon KC, et al. Clinicohistopathologic comparison of adult type and juvenile type xanthogranulomas in Korea. J Dermatol 2001;28:413-8.
[Google Scholar]
|
| 5. |
Redbord KP, Sheth AP. Multiple juvenile xanthogranulomas in a 13-year-old. Pediatr Dermatol 2007;24:238-40.
[Google Scholar]
|
| 6. |
Achar A, Naskar B, Mondal PC, Pal M. Multiple generalized xanthogranuloma in adult: Case report and treatment. Indian J Dermatol 2011;56:197-9.
[Google Scholar]
|
Fulltext Views
3,843
PDF downloads
2,071





