Translate this page into:
Falknor's needling method as a potential immunotherapy in palmo-plantar warts
2 Department of General Surgery, GMC, Kota, Rajasthan, India
Correspondence Address:
Devendra Yadav
KR207, MBS Hospital Campus, Opposite Circuit House, Kota, Rajasthan
India
| How to cite this article: Kumari P, Yadav D, Vijay A, Jain SK, Kumar M, Kumar R, Nyati A. Falknor's needling method as a potential immunotherapy in palmo-plantar warts. Indian J Dermatol Venereol Leprol 2019;85:129 |
Abstract
Background and Aim: Treatment of palmoplantar warts is a challenge for dermatologists. We aimed to study the efficacy and safety of Falknor's needling method in palmoplantar warts.
Methods: In an open, nonrandomized study, the index wart of eligible patients was punctured several times with a 26-gauge needle to produce a “beefy” red wound. Patients were followed up to 6 months.
Results: Out of 82 patients, complete resolution occurred in 58 (70.7%) and partial response in 5 (6.1%) patients. Nine (10.9%) patients developed secondary infection.
Limitations: Small sample size, No comparison group.
Conclusion: Falknor's needling method provides a high rate of complete resolution after a single treatment session. It is easy to perform and is cost effective.
Introduction
Viral wart is a common skin disease caused by human papilloma virus. Usually asymptomatic, sometimes they are unsightly, painful and debilitating. Though warts may disappear without treatment, sometimes they may persist for years.[1] More than 100 serotypes of human papilloma virus have been identified. Site and morphology of the lesions is usually determined by the serotype.[2] Palmoplantar warts are usually caused by serotypes 1, 2 and 4.[1]
Human papilloma virus prevents lysis of affected cells. There is only limited release of viral proteins resulting in inadequate antigen presentation to the immune system. Human papilloma virus proteins inhibit immune responses by activating T suppressor cells.[3],[4] Frazer concluded that induction of cell-mediated immunity by exposure to early proteins of human papilloma virus may prove helpful as a therapeutic approach.[4] There is a lack of immune response against the virus.,[5] So stimulation of immune response (immuno-modulation) against human papilloma virus is an emerging treatment strategy.[6]
Treatment of warts is often difficult despite availability of several modalities. There is no single method effective in all patients. An ideal treatment should result in resolution of all or majority of the warts, be painless, need only one or a part of a lesion to be treated, cosmetically acceptable and offer immunity against human papilloma virus for a lifetime.[7] It was Falknor who first described direct needling procedure, without the use of chemicals (other than local anaesthesia), as a treatment for warts.[8] His method comprised of anesthetizing the area, followed by thrusting in a needle “in dart fashion, so as to penetrate the full depth of the wart and exiting through the base of the capsule into the fat.” He claimed that there were only two recurrences out of 126 lesions treated with this technique. Subsequent published research using this method have been sparse. The aim of this study was to evaluate the safety and efficacy of needling procedure for the treatment of palmar and plantar warts.
Methods
An open label, prospective nonrandomized study was carried out between September 2015 and August 2016 at government medical college and hospital, Kota (Rajasthan) after obtaining clearance from institutional ethics committee. A total of 82 patients who were clinically diagnosed to have single/multiple plantar/palmar/palmoplantar warts were included in the study subject to the following criteria: All participants included in the study were aged 16 years and older. A treatment-free washout period of 3 months was ensured before the study All enrolled patients were found to be human immunodeficiency virus (HIV) - negative on testing. Written informed consent was obtained from all participants after counselling. Participants who were not previously immunized against tetanus were given injection tetanus toxoid 0.5ml intramuscularly at the screening visit. Baseline data was collected using a predesigned proforma.
Patients with a history of hypersensitivity reaction to local anesthesia, pregnancy and lactation, patients who had infection or poor tissue viability at the site of injection, who did not give consent to be a part of the study (refusal) were excluded. Other exclusion criteria were immunosuppression due to drugs or disease, advanced diseases of vital organs, inability to come for monthly follow-up and alcohol or other substance abuse.
The procedure was performed under strict aseptic conditions. In those patients with mosaic warts or multiple plantar warts, the index wart (the largest and thickest lesion) was selected for treatment. After cleansing with surgical spirit and infiltration with 2% lignocaine, the wart was paired superficially with an 11-number surgical blade. A fresh surgical needle (26 gauge) was used to puncture through the lesion repeatedly up to the level of subcutaneous tissue. Each puncture was just enough to produce pinpoint bleeding. This was continued till no more resistance or reactive pressure was felt from the epidermis. The end point was to produce a “beefy” red wound (video- 1). The number of punctures varied according to the size of the lesion (average number being 20–30/cm2).
Firm pressure was applied to the wound till there was no active bleeding and then a sterile gauze dressing was given. Patients were instructed to keep the dressing dry for 24 to 48 hours. To induce a successful controlled inflammatory response, each patient was advised to avoid taking nonsteroidal anti-inflammatory drugs for 48 hours.
Five follow-up visits were scheduled, first at 2 weeks then at 1, 2, 3 and 6 months. Efficacy of the procedure and adverse events were assessed and noted at each follow-up visit. Response was graded as complete (complete clearance of all lesions), partial (reduction in size and/or number of lesions) and no response (no response at all). If the wart/s had not cleared in six months, alternative treatments were offered. All participants were asked whether they were satisfied with the procedure or not.
Data was entered in Microsoft excel sheet and was analyzed using statistical package for social sciences (SPSS Version 16). P value of < 0.05 was considered to be statistically significant.
Results
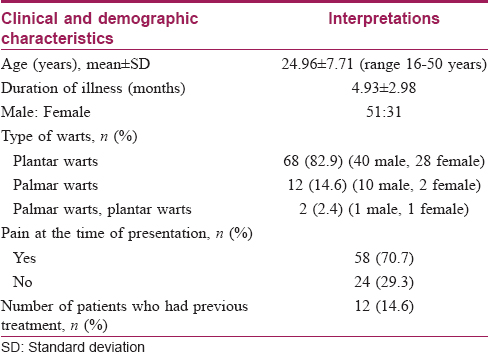
A total of 82 patients (51 males, 31 females) underwent the standardized needling procedure [Table - 1]. Mean age of the study group was 24.96 ± 7.71 years. The average reported duration of warts was 4.93 ± 2.98 months. Six patients had single plantar warts and others had multiple (range: 2–11) plantar/palmar warts. Out of 82 patients, 68 (82.9%) had plantar warts (40 males; 28 females), 12 (14.6%) patients had palmar warts (10 males; 2 females) and two (2.4%) patients had palmar and plantar warts. Twelve (14.6%) patients were previously unsuccessfully treated either with radiosurgery or autoimplantation. Out of 82 patients, 58 (70.7%) had pain prior to the procedure whereas in 24 patients (29.3%) the lesions were painless.
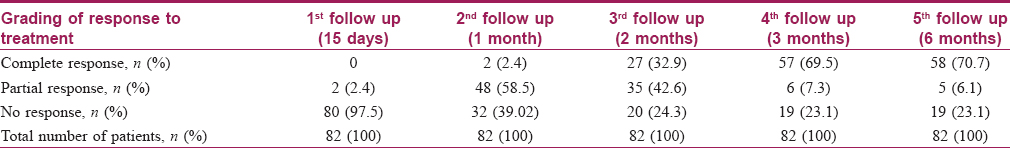
All patients returned for follow-up as advised. Fifty-eight (70.7%) patients (36 males and 22 females) showed complete response [Figure - 1] and [Figure - 2]. Five (6.1%) patients (three males and two females) showed partial response and 19 (23.1%) patients (12 males and 7 females) showed no response[Table - 2]. Average duration of resolution of lesions was 2.76 ± 1.1 months. There was no significant difference between response rate of plantar and palmar warts. Subgroup analysis showed no significant difference in response with respect to sex (P value = 0.99) or previous treatment. There was also no difference in the outcome between index warts and other warts (P value = 0.32) and that between single and multiple warts (P value = 0.72). Earliest response seen was at one month (two patients). Nine out of 82 patients (11%) patients developed secondary infection which was treated with a short course of empirical oral antibiotics. Post procedure pain was minimal and did not necessitate any drug intake. Out of 82 patients, 61 (74.4%) were satisfied with the given treatment, and there was no recurrence during the 6-month follow-up period in any of the patients.
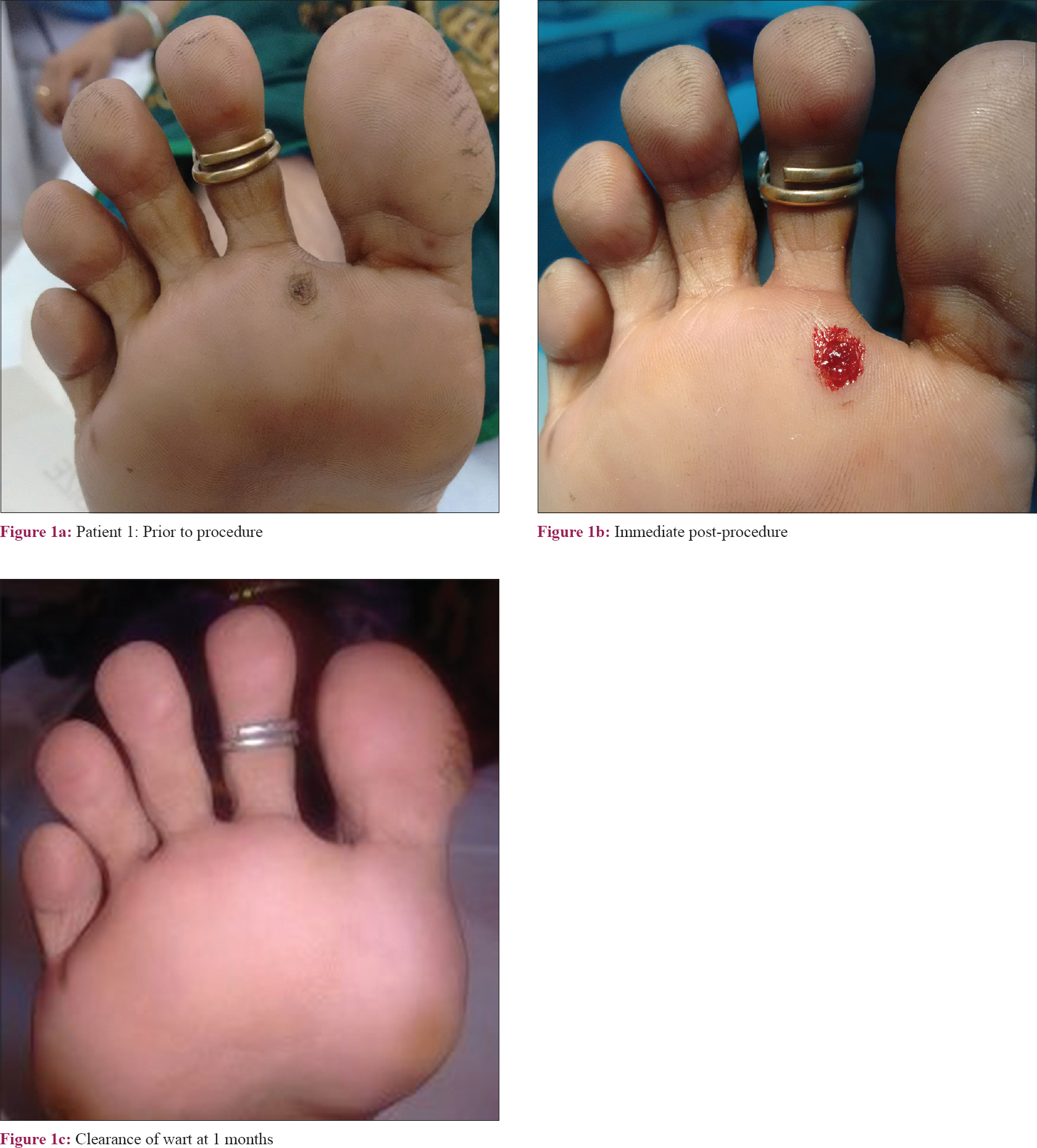 |
| Figure 1 |
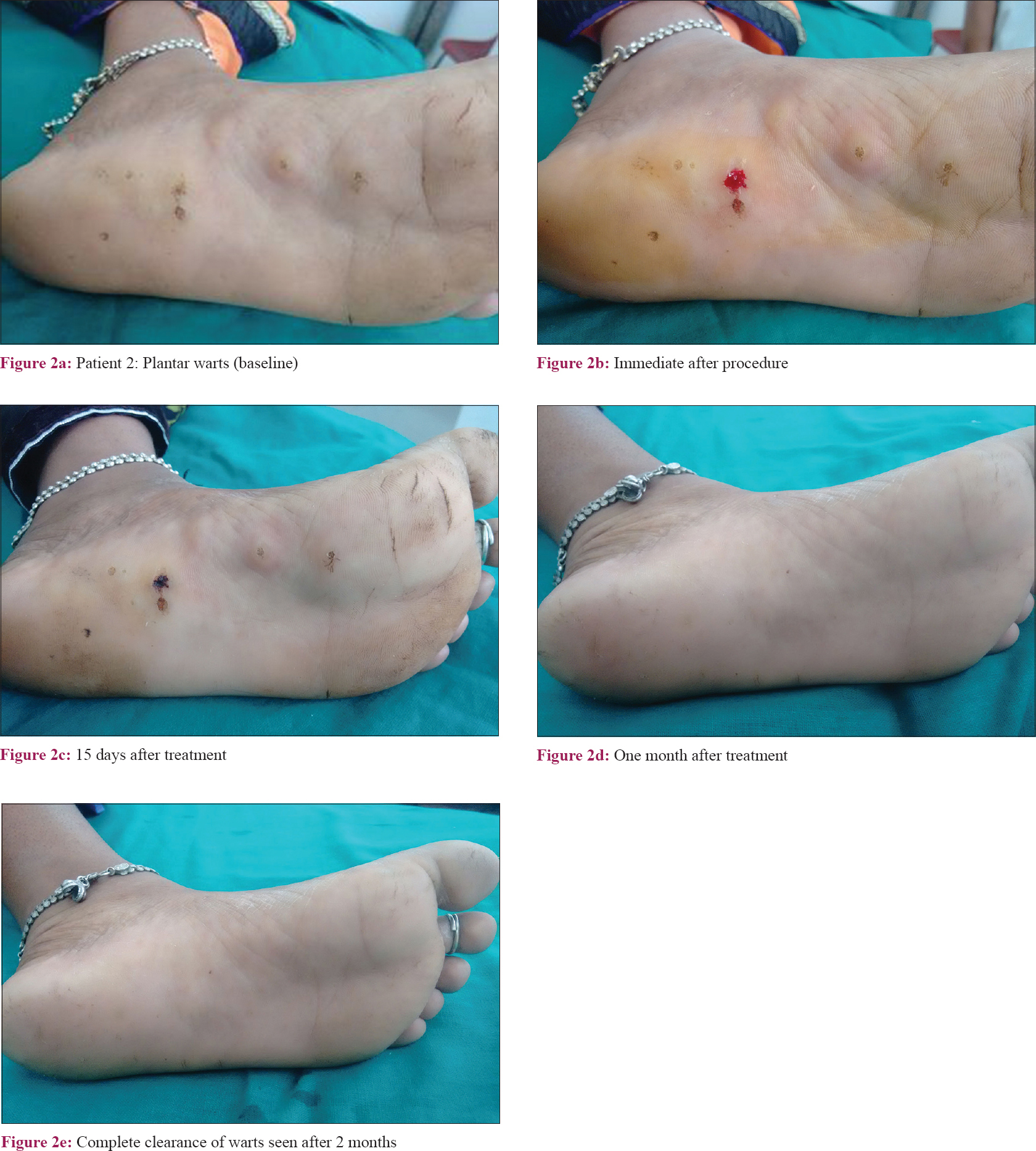 |
| Figure 2 |
Discussion
Although benign in nature, warts cause disfigurement and physical discomfort. They also have a tendency to koebnerize and carries risk of spread to others.[9] No single treatment is completely effective in all patients. Treatment options include cryotherapy, lasers, intralesional bleomycin, topical application of 5% imiquimod cream, systemic retinoids, photodynamic therapy and topical sensitizers such as dinitrochlorobenzene, squaric acid dibutylester and diphencyprone. Surgical excision, curettage, electrocautery and radiofrequency surgery are also commonly used. The success rate of these procedures is between 65% and 85%.[10],[11] Destructive or surgical treatments may be painful and can result in unsightly scars. The lesions may recur too.[12] Destructive procedures are especially inappropriate and impractical in the treatment of multiple warts, especially on the palms and soles.
Immunotherapy, which can act on lesions not intervened directly, would be particularly useful when treating patients with numerous warts, especially on areas difficult to access.
Cell-mediated immunity plays an important role in the treatment of warts.[5] Autoimplantation aims at stimulating cell-mediated immunity to human papilloma virus infection by introducing a high load of viral antigens.[13]
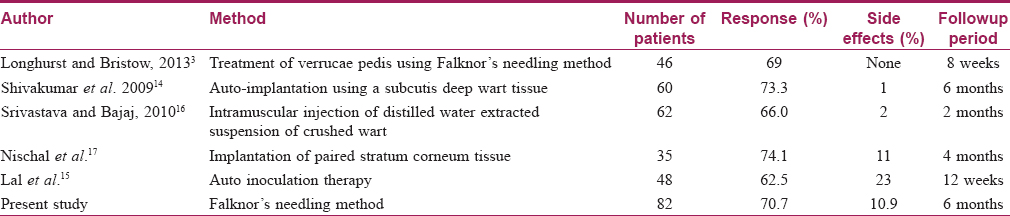
The current study represents the largest case series published to date using Falknor's method since the original paper was published in 1969. The procedure is simple and cost effective. There was complete resolution in 70.7% of patients with a single treatment session. Selecting only adults for the study minimised chances of spontaneous regression which is common in children. An article by Longhurst and Bristow of 46 patients with only plantar warts, using Falknor's needling method, showed complete resolution in 69% cases with 8 weeks of follow-up without recurrence [Table - 3].[3] A study by Shivakumar et al. involving 60 patients using autoimplantation technique (in which minced particles of wart tissue were introduced in dermal pocket), showed 73% clearing of warts within two months.[14] Lal et al. reported complete resolution of cutaneous warts in 62.5% of patients eight weeks after autoimplantation in a study involving 48 patients.[15] Eleven patients developed adverse events.[15] Adverse events were less frequent and mild in our study compared to other studies using auto-implantation methods.
Needling stimulates immune system resulting in clearance of even untreated lesions, in several patients. Introduction of human papilloma virus infected keratinocytes into the subcutaneous layer may facilitate a desired immune response.[3] Intra-lesional antigen therapy can, induce strong cellmediated immunity of predominantly Th1 type,[1] which could help to clear treated as well as distant warts.[14]
Overall, the results of this study are promising and further studies with comparison groups may be useful.
Limitations
As this study is a relatively small case series any inherent placebo effect cannot be excluded. We also could not check levels of Th1 cytokines to ascertain its in the mechanism of action.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patient understand that names and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Sterling JC, Gibbs S, Haque Hussain SS, MohdMustapa MF, Handfield-Jones SE. British Association of Dermatologists' guidelines for the management of cutaneous warts 2014. Br J Dermatol 2014;171:696-712.
[Google Scholar]
|
| 2. |
Colver G. Cryosurgery in podiatric practice. Podiatry Now 2005;8:S1-8.
[Google Scholar]
|
| 3. |
Longhurst B, Bristow I. The treatment of verrucae pedis using Falknor's needling method: A review of 46 cases. J Clin Med 2013;2:13-21.
[Google Scholar]
|
| 4. |
Frazer IH. Interaction of human papillomaviruses with the host immune system: A well evolved relationship. Virology 2009;384:410-4.
[Google Scholar]
|
| 5. |
Johnson SM, Roberson PK, Horn TD. Intralesional injection of mumps or candida skin test antigens: A novel immunotherapy for warts. Arch Dermatol 2001;137:451-5.
[Google Scholar]
|
| 6. |
Sterling JC. Virus infections. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 8th ed. Oxford: Blackwell Publishing; 2010. p. 33.48.
[Google Scholar]
|
| 7. |
Kuykendall-Ivy TD, Johnson SM. Evidence-based review of management of nongenital cutaneous warts. Cutis 2003;71:213-22.
[Google Scholar]
|
| 8. |
Falknor GW. Needling – A new technique in verruca therapy. J Am Podiatry Assoc 1969;59:51-2.
[Google Scholar]
|
| 9. |
Singh S, Chouhan K, Gupta S. Intralesional immunotherapy with killed Mycobacterium indicuspranii vaccine for the treatment of extensive cutaneous warts. Indian J Dermatol Venereol Leprol 2014;80:509-14.
[Google Scholar]
|
| 10. |
Lipke MM. An armamentarium of wart treatments. Clin Med Res 2006;4:273-93.
[Google Scholar]
|
| 11. |
Iwatsuki K, Tagami H, Takigawa M, Yamada M. Plane warts under spontaneous regression. Immunopathologic study on cellular constituents leading to the inflammatory reaction. Arch Dermatol 1986;122:655-9.
[Google Scholar]
|
| 12. |
Arndt KA, Bowers KE, Alam M, Reynolds R, Tsao S, editors. Warts. In: Manual of Dermatologic Therapeutics. 6th ed. Philadelphia: Lippincott, Williams & Wilkins; 2002. p. 241-51.
[Google Scholar]
|
| 13. |
Thappa DM, Chiramel MJ. Evolving role of immunotherapy in the treatment of refractory warts. Indian Dermatol Online J 2016;7:364-70.
[Google Scholar]
|
| 14. |
Shivakumar V, Okade R, Rajkumar V. Autoimplantation therapy for multiple warts. Indian J Dermatol Venereol Leprol 2009;75:593-5.
[Google Scholar]
|
| 15. |
Lal NR, Sil A, Gayen T, Bandyopadhyay D, Das NK. Safety and effectiveness of autoinoculation therapy in cutaneous warts: A double–blind, randomized, placebo–controlled study. Indian J Dermatol Venereol Leprol 2014;80:515-20.
[Google Scholar]
|
| 16. |
Srivastava PK, Bajaj AK. Autowart injection therapy for recalcitrant warts. Indian J Dermatol 2010;55:367-9.
[Google Scholar]
|
| 17. |
Nischal KC, Sowmya CS, Swaroop MR, Agrawal DP, Basavaraj HB, Sathyanarayana BD, et al. Anovel modification of the autoimplantation therapy for the treatment of multiple, recurrent and palmoplantar warts. J Cutan Aesthet Surg 2012;5:26-9.
[Google Scholar]
|
Fulltext Views
8,521
PDF downloads
4,067





