Translate this page into:
Familial reactive perforating collagenosis in three siblings
2 Department of Pathology, National Institute of Pathology, ICMR, New Delhi, India
Correspondence Address:
Rajat Kandhari
11 Munirka Marg, Vasant Vihar, New Delhi - 110 057
India
| How to cite this article: Kandhari R, Sharma V, Ramesh V, Singh A. Familial reactive perforating collagenosis in three siblings. Indian J Dermatol Venereol Leprol 2014;80:86-87 |
Sir,
Reactive perforating collagenosis (RPC) is an uncommon, benign, perforating dermatosis of multifactorial etiology first described in 1967. [1] It is characterized by transepidermal elimination [2] of altered collagen through the epidermis and clinically presents as spontaneously involuting papules with a scab-like central plug, which on removal reveals a crateriform lesion. The common variant of RPC is acquired in adulthood and is typically associated with diabetes mellitus and chronic renal failure. The familial variant of RPC is rare, affects one or more family members, presents at an early age and is usually triggered by simple trauma. [3]
Three sisters aged 8, 11 and 13 years presented to us with multiple, shallow, well defined facial scars that had appeared spontaneously around the age of 3. The mother added that the scars were preceded by raised, erythematous lesions, associated with mild itching, often appearing during the summer and regressing over a month in a cyclical pattern. No similar lesions were noted in any other family members and there was no history of parental consanguinity. On examination, all three sisters had multiple, shallow, well-defined, atrophic scars of varying morphology present bilaterally on the cheeks [Figure - 1]a-c. A single "crateriform" lesion was seen in the youngest sibling on the left cheek [Figure - 2] and a few, discrete, skin colored papules with central plugging were present on the face of the eldest sibling. Similar lesions of varying size, approximately 2-4 mm, were also present on bilateral forearms and dorsae of the hands [Figure - 3]. No evidence of koebnerization was noted. Routine laboratory investigations including blood sugar and renal function tests were normal. Histopathological examination from the papules revealed a cup shaped invagination of the epidermis showing keratotic debris along with vertically oriented collagen indicating extrusion. Van Gieson staining demonstrated transepidermal elimination of collagen fibers [Figure - 4].
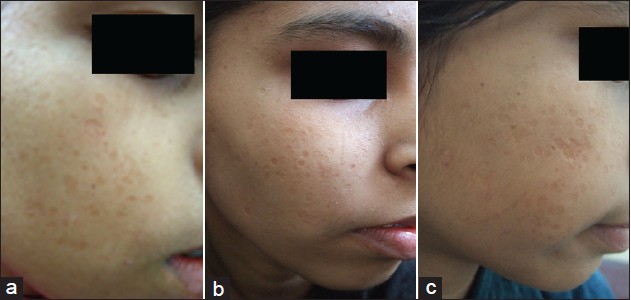 |
| Figure 1: (a-c) Well defi ned, atrophic scars of varying morphology present on the cheeks of all three siblings |
 |
| Figure 2: "Crateriform" lesion with adjacent scars |
 |
| Figure 3: Discrete, skin colored papules with central plugging seen on the dorsum of the hand |
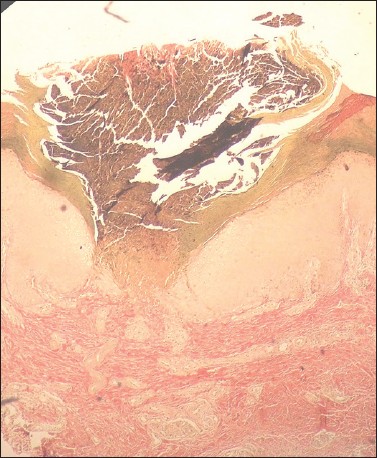 |
| Figure 4: Crateriform lesion showing epidermal perforation (Van Gieson x 100) |
The abnormal collagen fibers along with the keratinous material of the epidermis, serum and inflammatory cells form the inspissated central plug, which is later extruded. [3] Some authors have reported no abnormalities in collagen, [4] whereas others believe that RPC may be a result of a biochemical alteration in the collagen [5] or predisposing trauma, which results in altered collagen in genetically predisposed individuals. [6] The pattern of inheritance in familial RPC is unclear.
The extreme variability in expression necessitates careful examination of all family members. [3] Familial RPC is more common in males and commonly involves the extremities with facial involvement being relatively uncommon. All our cases were females with facial involvement and presence of atrophic scarring. The scars varied in size and shape, some were round whereas others were linear in configuration. Atrophic scarring is uncommon and may be due to spontaneous occurrence of facial lesions in cold weather [7] and the habit of picking.
Treatment of RPC is challenging and involves the use of topical keratolytics and corticosteroids. Topical tretinoin has shown successful results. [8] Vitamin A, methotrexate and tetracyclines have been tried with variable success. Surgical debridement, improved diabetic control, bio-occlusive dressings and even split skin grafting has been tried for recalcitrant lesions. [9] All of our cases were given tretinoin 0.05% cream, following which the lesions healed with scarring over a period of 1 month. Patients were subsequently lost to follow-up.
| 1. |
Mehregan AH, Schwartz OD, Livingood CS. Reactive perforating collagenosis. Arch Dermatol 1967;96:277-82.
[Google Scholar]
|
| 2. |
Ortega del Olmo RM, de Dulanto Escofet F, Naranjo Sintes R, Camacho Martinez F. Dermatosis with the phenomenon of transepidermal elimination. Med Cutan Ibero Lat Am 1988;16:1-9.
[Google Scholar]
|
| 3. |
Ramesh V, Sood N, Kubba A, Singh B, Makkar R. Familial reactive perforating collagenosis: A clinical, histopathological study of 10 cases. J Eur Acad Dermatol Venereol 2007;21:766-70.
[Google Scholar]
|
| 4. |
Millard PR, Young E, Harrison DE, Wojnarowska F. Reactive per forating collagenosis: Light, ultrastructural and immunohistological studies. Histopathology 1986;10:1047-56.
[Google Scholar]
|
| 5. |
Herzinger T, Schirren CG, Sander CA, Jansen T, Kind P. Reactive perforating collagenosis-transepidermal elimination of type IV collagen. Clin Exp Dermatol 1996;21:279-82.
[Google Scholar]
|
| 6. |
Bovenmyer DA. Reactive perforating collagenosis. Experimental production of the lesion. Arch Dermatol 1970;102:313-7.
[Google Scholar]
|
| 7. |
Kanan MW. Familial reactive perforating collagenosis and intolerance to cold. Br J Dermatol 1974;91:405-14.
[Google Scholar]
|
| 8. |
Cullen SI. Successful treatment of reactive perforating collagenosis with tretinoin. Cutis 1979;23:187-91,193.
[Google Scholar]
|
| 9. |
Oziemski MA, Billson VR, Crosthwaite GL, Zajac J, Varigos GA. A new treatment for acquired reactive perforating collagenosis. Australas J Dermatol 1991;32:71-4.
[Google Scholar]
|
Fulltext Views
3,847
PDF downloads
3,075





