Translate this page into:
Foamy histiocytes in sarcoidosis! Puzzle resolved with the aid of tattoo
Corresponding author: Dr. Shreya K Junior Resident, Department of Dermatology and Venereology AIIMS, Habibganj, Saketnagar, Bhopal. shreyakgowda@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shreya K, Rout AN, Asati DP, Panwar H. Foamy histiocytes in sarcoidosis! Puzzle resolved with the aid of tattoo. Indian J Dermatol Venereol Leprol 2023;89:84-7.
Sir,
A 35-year-old immunocompetent, healthy woman from Bihar, presented with multiple asymptomatic papules over her neck, which gradually progressed to involve her chest, back and extremities over last six months. She also reported multiple hypopigmented macules on her back and extremities for same duration. She revealed a history of tattooing over right forearm in her childhood. On examination, two different types of lesions were noted- multiple, discrete, shiny, juicy red-brown papules with generalised distribution [Figure 1a] and multiple, hypopigmented, non-scaly discrete macules with preserved sensation, over bilateral extremities and back [Figures 1b and c]. There was no evidence of nerve thickening, sensory loss, ear lobule infiltration or lymphadenopathy, induration over tattoo area, respiratory or ocular symptoms, history of fever, malaise or arthralgia.

- Multiple discrete shiny juicy red-brown papules over neck, trunk and extremities

- Multiple hypopigmented non-scaly discrete macules with preserved sensation over bilateral lower extremities
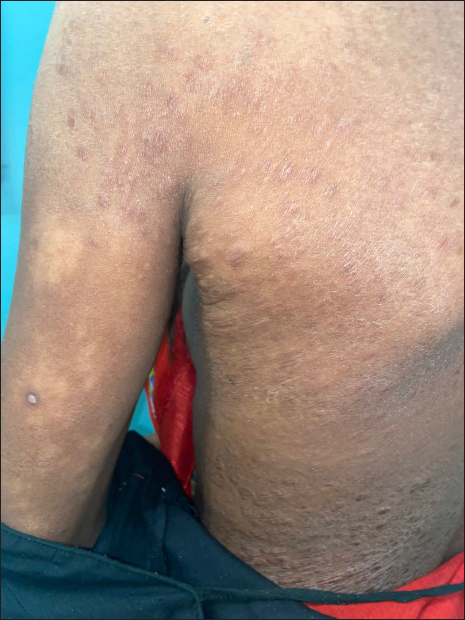
- Multiple hypopigmented non-scaly macules with intact sensation over back
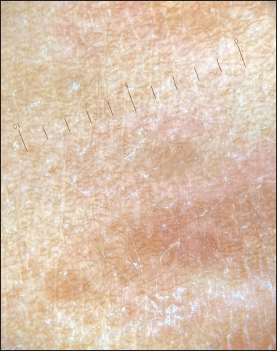
We considered clinical differentials of sarcoidosis, lepromatous leprosy, post-kala-azar dermal leishmaniasis, generalised granuloma annulare and histoplasmosis. Biopsy from brown papule and hypopigmented macule demonstrated multiple well-defined granulomas, composed of foamy histiocytes, lymphocytes and Langhan’s giant cells in periadnexal distribution, suggestive of borderline tuberculoid Hansen disease [Figure 2]. However, staining for acid-fast bacilli, periodic acid Schiff (PAS) and Giemsa were negative. Slit skin smear from papule and ear lobule was negative. Routine investigations like complete hemogram, liver function, fasting sugar and renal function were non-contributory.
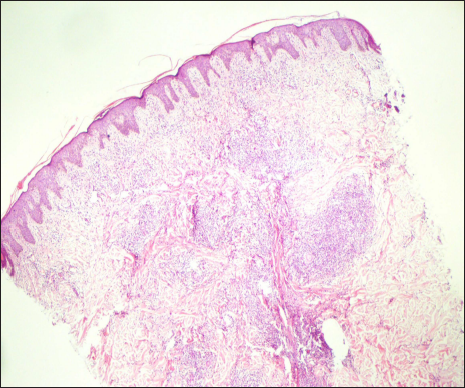
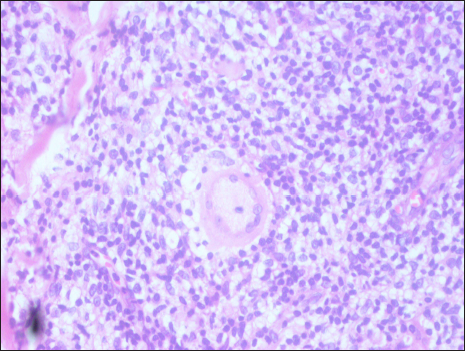
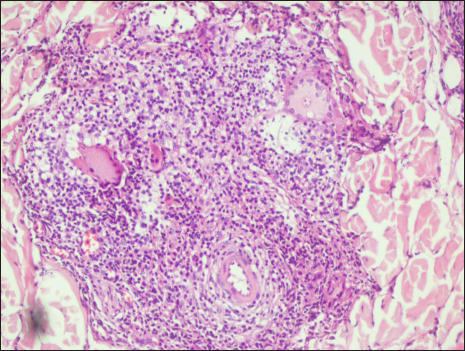
- Perivascular and periadnexal well-defined granuloma composed of lymphocytes, foamy histiocytes and giant cells (haematoxylin and eosin, 4×)
Thus, although clinically suspected as lepromatous leprosy, histology favored borderline tuberculoid Hansen. Despite discrepancy, we administered MB-MDT for three months, without any appreciable improvement. On her next visit, examination revealed induration and tiny studded papules on amateur tattoo over the right forearm [Figure 3a], and linearly arranged papules over abdomen, suggestive of Koebnerization. Dermoscopy (Dermlite DL3 Polarized mode) of papules over tattoo revealed orange-yellow structureless area corresponding to granuloma, orange-yellow hue and haziness in blue tattoo suggestive of tattoo granuloma [Figures 3b and c]. Repeat biopsy from a papule showed multiple well-defined granulomas composed of foamy histiocytes, lymphocytes and Schaumann bodies within Langhan’s giant cells [Figures 4a and b]. Reticulin stain was also done to find intact reticulin fibres, consistent with diagnosis of sarcoidosis over borderline tuberculoid Hansen disease. [Figure 4c]. Chest X-ray demonstrated subtle bilateral reticulonodular opacities without lymphadenopathy, while elevated erythrocyte sedimentation rate (60 mm/hour), serum calcium level (15 mg/dL) and serum Angiotensin Converting Enzyme level (400 nmol/mL/min) were noted on biochemistry. Ophthalmological evaluation was normal. We started oral prednisolone at 1 mg/kg/day, with significant resolution of skin lesions after three months of therapy [Figures 5a and b]. Pulmonary reference was sought for lung involvement.
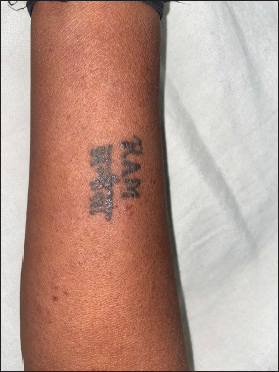
- Increase in induration of amateur tattoo over the right forearm
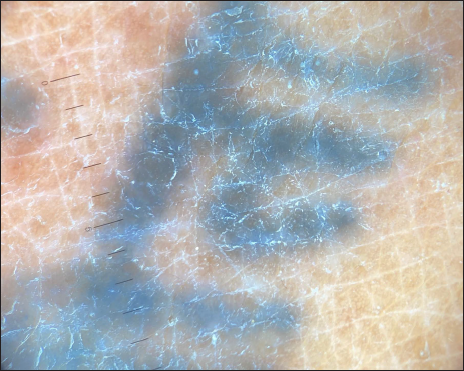
- Dermlite DL3 polarized mode shows haziness in blue tattoo
- Dermoscopy using dermlite DL3 polarized mode show brown to slight orange hue from papule over chest
- Well-defined granuloma composed of foamy histiocytes and Schaumann bodies within Langhans giant cells with no fungal elements (periodic acid-Schiff, 40×)
- Perivascular and periadnexal well-defined granuloma composed of foamy histiocytes and Schaumann bodies within Langhans giant cells (Haematoxylin and eosin, 40×)
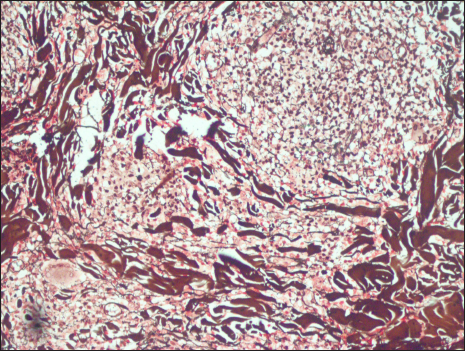
- Reticulin stain positivity

- Decrease in thickness and number of papules over neck and chest

- Resolution of papules over back
Various lesional morphologies (like hypopigmented macule, juicy papule and tattoo granuloma), development of tattoo sarcoid reaction late in the disease course, single colour (blue pigment amateur tattoo) tattoo granuloma, foamy histiocytic infiltrate in histopathology makes our case an unusual presentation. Thus, a keen clinical acumen and clinicopathological correlation are necessary for diagnosing granulomatous disorders.
Sarcoidosis is a multisystem granulomatous disorder, of idiopathic origin. Lungs, lymph nodes, eyes and skin are involved in decreasing the order of frequency, skin involvement being reported in 9–37% cases. Cutaneous sarcoidosis manifests as maculopapular, nodular, subcutaneous sarcoidosis, hypopigmented, vegetating, lichenoid, ichthyosiform, erythrodermic, livedo–like and scar sarcoidosis.1
Tattooing is an ancient art which can be amateur or professional. It can cause several reaction patterns such as lichenoid, granulomatous and foreign body. Photoallergic reaction due to cadmium in the yellow tattoo, foreign body reaction following red tattoo due to mercury, and sarcoidal reaction in red and yellow tattoos have been described.2 Systemic sarcoidosis manifests as sarcoid tattoo granuloma in 10% cases. The first case of tattoo sarcoid granuloma was described by Lubeck and Epstein. Sole manifestation as sarcoid tattoo reaction has also been reported by Madden without any evidence of lung involvement.3 Various theories have been proposed concerning pathogenesis of tattoo sarcoidal reaction [Table 1].
| Sl no | Proposed mechanism | References | |
|---|---|---|---|
| 1 | Koebnerization | Sarcoidosis develops many years after the application of the tattoo site. | 4 |
| 2 | Specific tattoo pigments induce scar formation | Parallel to the development of sarcoidosis within scars. | 7 |
| 3 | Immunologic reaction directed at one or more specific tattoo pigments. | Pigments within the tattoos act as a nidus for granuloma formation in systemic sarcoidosis. Specific antigen in the tattoo pigment may induce a cell-mediated immune response. | 8 |
Biopsy of sarcoidosis classically shows naked sarcoid granuloma. Interstitial and tuberculoid granulomas are rarely seen. Perineural and peri adnexal granulomas have also been reported, along with fibrinoid and caseous necrosis. Sarcoidosis is a diagnosis of exclusion.5 In our case, periadnexal granuloma with foamy histiocytes was seen, which is rarely described in the literature. The patient is usually counselled regarding the risk of scar site sarcoid reaction prior to biopsy. There is no US FDA approved drug for cutaneous sarcoid reaction. The first-line therapy includes topical, oral and intralesional steroids. Immunosuppressants like methotrexate are added as adjuvants when systemic involvement is present. Other treatment options include thalidomide and tumor necrosis factor alfa inhibitor.6 Recently, Janus kinase inhibitors are being tried with a promising response.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Sarcoidosis: A comprehensive review and update for the dermatologist: Part I. Cutaneous disease. J Am Acad Dermatol. 2012;66:699.e1-e18.
- [CrossRef] [PubMed] [Google Scholar]
- Sarcoid granuloma on black tattoo. J Am Acad Dermatol. 2006;55:S71-3.
- [CrossRef] [PubMed] [Google Scholar]
- Systemic sarcoidosis presenting with multiple tattoo granulomas and an extra-tattoo cutaneous granuloma. J Eur Acad Dermatol Venereol. 1999;12:51-3.
- [PubMed] [Google Scholar]
- From silica granuloma to scar sarcoidosis. Clin Exp Dermatol. 1983;8:171-5.
- [CrossRef] [PubMed] [Google Scholar]
- Weedon’s Skin Pathology E-Book: Expert Consult-Online and Print Elsevier Health Sciences; 2009.
- [Google Scholar]
- Skin as a marker of internal disease: A case of sarcoidosis. Indian J Dermatol. 2011;56:439-41.
- [CrossRef] [PubMed] [Google Scholar]
- Sarcoidosis presenting as tattoo changes in a patient undergoing treatment with interferon-alpha and ribavirin. Clin Exp Dermatol. 2004;29:547-8.
- [CrossRef] [PubMed] [Google Scholar]





