Translate this page into:
Fractional CO2 laser with topical 1% terbinafine cream versus oral itraconazole in the management of onychomycosis: A randomized controlled trial
Corresponding author: Dr. Eeshaan Ranjan, Department of Dermatology, Military Hospital Jammu, Satwari Cantt, Jammu 180003, Jammu and Kashmir, India. eeshaan.ranjan@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ranjan E, Arora S, Sharma N. Fractional CO2 laser with topical 1% terbinafine cream versus oral itraconazole in the management of onychomycosis: A randomized controlled trial. Indian J Dermatol Venereol Leprol 2023;89:47-53.
Abstract
Background
Onychomycosis accounts for 20-40% of all nail disorders. It is difficult to cure with resistance to anti-fungal drugs, their side effects and drug interactions limiting treatment options. Itraconazole is a widely accepted oral medication used for onychomycosis while fractional CO2 laser along with a topical anti-fungal has shown promising results for nail plate clearance in onychomycosis.
Aim
To compare the efficacy of fractional CO2 laser with 1% terbinafine cream versus itraconazole in the management of onychomycosis.
Methods
A prospective, randomised, single-centre, two-arm, parallel-group interventional study was conducted at Command Hospital Air Force, Bangalore. Onychomycosis cases confirmed by KOH mount/culture-positive were included. Patients were randomly divided into two groups. Group A received 4 sessions of fractional CO2 laser every fourth week with twice-daily application of 1% terbinafine cream; Group B received one-week pulse therapy with capsule itraconazole once every four-week for three pulses. The response was assessed by Onychomycosis Severity Index, a validated onychomycosis assessment scale, at baseline and at six months.
Results
Group A had 50 patients with a total of 98 nails. Clinical improvement was seen in 83/98 (84.7%) nails. The average reduction in Onychomycosis Severity Index was 8.65 (P < 0.05). Group B had 50 patients with a total of 136 nails. Clinical improvement was seen in 104/136 (76.5%) nails. The average reduction in Onychomycosis Severity Index was 7.37 (P < 0.05). Both groups showed statistically significant improvement measured by ‘Reduction in Onychomycosis Severity Index’ at six months; however, there was no significant difference between the two arms.
Limitations
The main limitations of the study are the small sample size and lack of long-term follow-up to assess recurrence of infection.
Conclusion
Fractional CO2 laser with 1% terbinafine cream is an effective and safe method for inducing nail clearance in onychomycosis and has efficacy similar to itraconazole pulse therapy.
Keywords
Fractional CO2 laser
itraconazole
onychomycosis
terbinafine
Plain Language Summary
Onychomycosis is the fungal infection of nail. Reported incidence is 0.5-5 percent in India. Itraconazole is an antifungal medicine used for treatment. Side effects like headache, diarrhoea, liver abnormalities and contraindication like heart failure limit its use. Recent studies have found Fractional carbon-dioxide (FCO2) laser with anti-fungal cream to be effective. We conducted a study in a hospital in India to compare FCO2 laser with 1% terbinafine cream versus itraconazole in management of onychomycosis. Patients were distributed into 2 groups of 50 each. First group was treated with FCO2 laser, 4-sessions at 4-week intervals alongwith daily application of terbinafine. Second group was treated with Itraconazole 200 mg twice-daily, one-week per month for three months. Severity scores of nail infection and photographs were documented at baseline and at six months. Severity scores in both groups were similar at baseline and at 6 months, showing similar response with treatment. Patient satisfaction and compliance was better in first group, no side effects were observed. The study shows that FCO2 laser with 1% terbinafine cream is equally effective in onychomycosis. It can be used in patients where itraconazole is contraindicated as it has no significant side effects and drug interactions.
Introduction
Onychomycosis describes the fungal infection of the nail unit caused by dermatophytes, yeasts, or non-dermatophyte moulds.1 Various workers have reported the incidence between 0.5 and 5% in the general population in India.2,3 It can have significant negative effect on patients’ quality of life and occupational functioning.4 The most frequently implicated causative agents in onychomycosis are dermatophytes. Previously regarded as contaminants, yeasts and some moulds are now increasingly recognised as pathogens in fingernail infections.5
Itraconazole, a triazole antifungal, has the broadest spectrum of antifungal activity against dermatophytes, candida, and non-dermatophyte moulds. Intermittent therapy is effective and results in higher plasma concentrations, lower cumulative dose as compared to continuous therapy6 and results in equal mycological and higher clinical cure when compared to the continuous regimen.7 The common adverse effects include headache, nausea and gastrointestinal upset as well as asymptomatic liver function abnormalities. Hepatitis tends to occur with continuous therapy usually after four weeks. It is contraindicated in patients with congestive cardiac failure due to the increased risk of negative inotropic effects.8
Laser therapy for onychomycosis is a newer treatment modality. Using the principle of selective photothermolysis, lasers have a photothermal effect on fungi, with chitin augmenting the heating effect.9 More recent trials have explored fractional carbon dioxide lasers in combination with topical treatment and found it to be a viable option for management of onychomycosis.10-15
In this context, we conducted a randomised controlled trial to compare the efficacy of a combination of fractional carbon dioxide laser with topical 1% terbinafine cream versus itraconazole in the management of onychomycosis and to find the possible superiority of one treatment over other.
Methods
A prospective, randomised, interventional parallel-arm study was conducted at the dermatology department of Command Hospital Air Force, Bangalore from December 2017 to May 2019 after institutional ethical clearance and informed patient consent. All consecutive patients over the age of 18 years of either gender presenting with one or more toenails and/or fingernails onychomycosis were included. Diagnosis of onychomycosis was confirmed on demonstration of fungal hyphae on direct microscopy and fungal culture. Pregnant and lactating women, cases with negative KOH mount for fungal hyphae and negative fungal culture, persons on systemic or topical anti-fungals in the past three months and those with nail disorders due to psoriasis, chronic eczema, lichen planus, bacterial infections, subungual hematoma were excluded.
All the cases were assessed clinically, and objectively scored using “Onychomycosis Severity Index”16 [Table 1] and the pattern of involvement was determined as distal lateral subungual onychomycosis, proximal subungual onychomycosis, white superficial onychomycosis, total dystrophic onychomycosis. The patients were randomised through a draw of cards and allocated to either study arm. One study arm received treatment with fractional carbon dioxide laser once in four weeks along with the topical application of 1% terbinafine cream and the other was administered capsule itraconazole.
| Area of involvement | |
|---|---|
| Affected nail percentage | Number of points |
| 0 | 0 |
| 1-10 | 1 |
| 11-25 | 2 |
| 26-50 | 3 |
| 51-75 | 4 |
| 76-100 | 5 |
| Proximity of disease to matrix | |
| Amount of involvement from distal edge | Number of points |
| <1/4 | 1 |
| 1/4-1/2 | 2 |
| >1/2-3/4 | 3 |
| >3/4 | 4 |
| Matrix involvement | 5 |
| Presence of dermatophytoma or subungal hyperkeratosis >2 mm | |
| Present | Number of points |
| No | 0 |
| Yes | 10 |
| Final score (OSI): (Score for area of involvement) × (score for proximity of disease to matrix) + 10 (if dermatophytoma or subungual hyperkeratosis >2 mm) | |
For topical anaesthesia before laser therapy, topical anaesthesia (lidocaine 7% w/w + tetracaine 7% w/w) was applied under occlusion on the infected nail and periungual area for 45 minutes. All the infected nails were treated with fractional carbon dioxide laser using pulse energy of 110 mJ, the energy density of 256 spots/cm2, a pulse interval of 0.5 mm, pulse duration of 0.1 milliseconds, and a rectangular spot size of 2-10 mm length and 0.6-5 mm breadth. three passes were given in static operating mode over the affected area including 1 mm normal-appearing nail around them. Altogether four sessions of laser therapy were given, each at four-week intervals. Topical 1% terbinafine cream was then advised to be applied to the affected nails twice daily. In the other arm, itraconazole 200 mg twice daily was administered for one week per month for three months. Follow-up was performed at each visit at four-week intervals with an assessment of clinical improvement using Onychomycosis Severity Index score and photography. Analysis of the data was carried out six months after the institution of therapy. The data was maintained prospectively in a computerized database. Side effects, due to fractional carbon dioxide laser-like, erythema, itching or burning or oral itraconazole were monitored and followed up every week for 12 weeks. Liver function tests were done every month in patients taking itraconazole.
Data were tabulated into an excel sheet and analysed using SPSS version 16.0. The data were expressed in means and proportions. Repeated measurement analysis of variance was used to evaluate the changes in the Onychomycosis Severity Index score before and after treatments and the difference between the groups was evaluated using an independent t -test. A P value of <0.05 was taken as statistically significant.
Results
A total of 261 patients of onychomycosis were assessed for eligibility out of which 122 patients satisfying the above-mentioned criteria were identified and included in the study [Figure 1]. The data of 100 patients was analysed finally after excluding the patients lost to follow up.
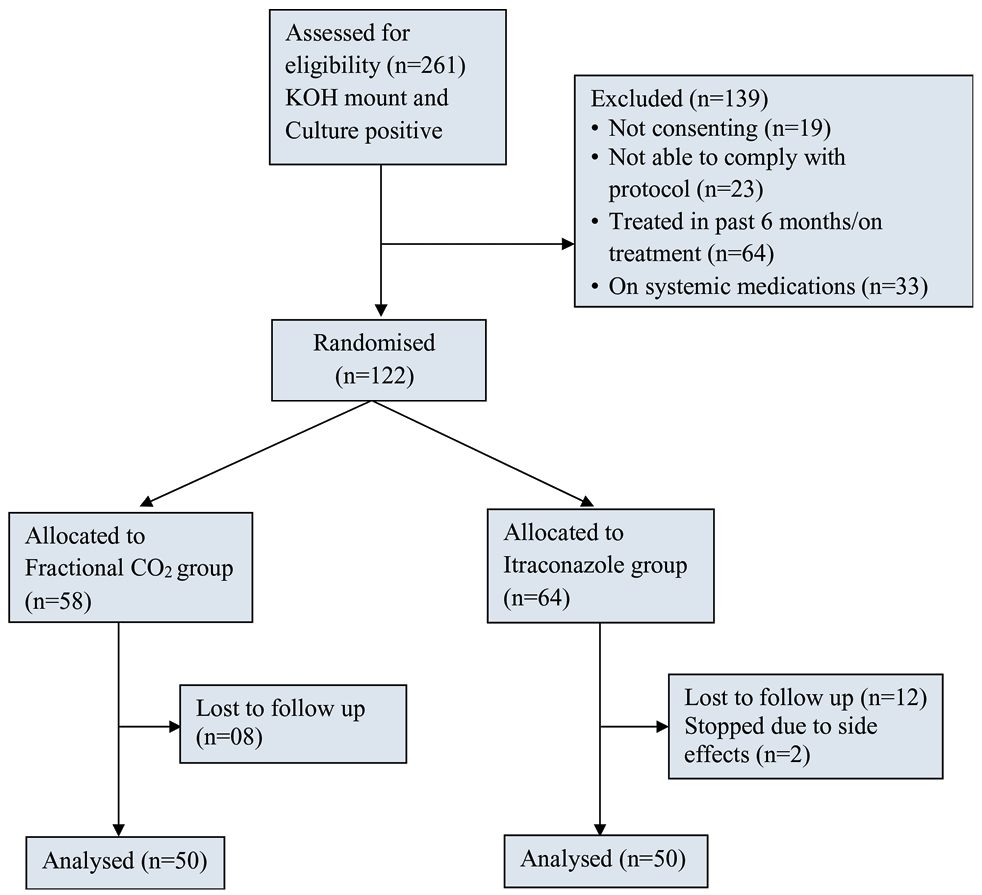
- CONSORT Statement of the study
The clinico-demographic distribution between two arms is shown in [Table 2]. Both groups were matched for gender and age [Table 2]. The total number of nails studied in the fractional carbon dioxide laser arm was 98 among 50 patients and in the itraconazole arm were 136 among 50 patients. Most of the nails involved in both groups were toenails [Table 2]. The most common type of onychomycosis found in our study was distal lateral subungual onychomycosis, followed by total dystrophic onychomycosis type. White superficial onychomycosis type of onychomycosis was found to be the least common in both arms [Table 2].
| Fractional CO2 laser | Itraconazole | Total* | |
|---|---|---|---|
| Age in years | |||
| ≤30 | 8 (16%) | 13 (26%) | 21 (21%) |
| 31-40 | 10 (20%) | 8 (16%) | 18 (18%) |
| 41-50 | 13 (26%) | 10 (20%) | 23 (23%) |
| 51-60 | 11 (22%) | 16 (32%) | 27 (27%) |
| >60 | 8 (16%) | 3 (6%) | 11 (11%) |
| Total | 50 (100) | 50 (100) | 100 (100) |
| Gender | |||
| Females | 22 (44%) | 30 (60%) | 52 (52%) |
| Males | 28 (56%) | 20 (40%) | 48 (48%) |
| Total | 50 (100) | 50 (100) | 100 (100%) |
| Type | |||
| Toenail | 77 (78.6%) | 101 (74.3%) | 178 (76%) |
| Fingernail | 21 (21.4%) | 35 (25.7%) | 56 (24%) |
| Total | 98 (100) | 136 (100) | 234 (100%) |
| Pattern of onychomycosis | |||
| DLSO | 68 (69.4%) | 109 (80.1%) | 177 (75.6) |
| TDO | 23 (23.5%) | 17 (12.5%) | 40 (17.1) |
| WSO | 7 (7.1%) | 10 (7.4%) | 17 (7.3) |
| Total | 98 (100%) | 136 (100%) | 234 (100%) |
At the end of the study, clinical improvement was seen in 83 nails out of 98 nails (84.7%) in the fractional carbon dioxide arm. In the itraconazole arm, clinical response was seen in 104 nails out of 136 nails (76.5%). The mean of Onychomycosis Severity Index scores in the itraconazole group was lower as compared to the fractional carbon dioxide group at baseline and higher as compared to fractional carbon dioxide after six months’ follow-up. However, the difference in the means among the patients in both the groups was not statistically significant [Table 3]. Also, improvement in terms of decrease in Onychomycosis Severity Index was higher in fractional carbon dioxide arm as compared to itraconazole arm but it was not found to be statistically significant (P- value 0.157) [Table 3]. Among the toenails of study subjects of fractional carbon dioxide and itraconazole groups, though the means of Onychomycosis Severity Index scores were higher in the itraconazole group compared to the fractional carbon dioxide group, at baseline and after six months follow-up, the difference in the means among the patients in both the groups were not statistically significant. Also, improvement in terms of decrease in Onychomycosis Severity Index was higher in fractional carbon dioxide arm but it was not found to be statistically significant [Table 3].
| Fractional CO2 laser (Mean ± SD) |
Itraconazole (Mean ± SD) |
P-value | |
|---|---|---|---|
| All nails | |||
| OSI before treatment | 17.06 ± 9.66 | 16.92 ± 9.59 | 0.911 |
| OSI at 6 months | 8.40 ± 9.76 | 9.55 ± 9.79 | 0.378 |
| Mean reduction in OSI with treatment | 8.65 ± 7.09 | 7.36 ± 6.65 | 0.157 |
| Toenail | |||
| OSI before treatment | 18.13 ± 9.15 | 18.45 ± 9.10 | 0.813 |
| OSI at 6 months | 8.8 ± 9.41 | 10.56 ± 9.70 | 0.22 |
| Mean reduction in OSI with treatment | 9.32 ± 7.12 | 7.89 ± 6.09 | 0.15 |
| Fingernail | |||
| OSI before treatment | 13.14 ± 11 | 12.48 ± 9.73 | 0.814 |
| OSI at 6 months | 6.95 ± 11 | 6.63 ± 9.59 | 0.908 |
| Mean reduction in OSI with treatment | 6.19 ± 6.58 | 5.85 ± 7.96 | 0.872 |
| DLSO | |||
| OSI before treatment | 14.35 ± 8.87 | 15.52 ± 9.32 | 0.409 |
| OSI at 6 months | 5.30 ± 7.21 | 8.76 ± 8.61 | 0.650 |
| Mean reduction in OSI with treatment | 9.05 ± 7.11 | 6.76 ± 6.08 | 0.243 |
| TDO | |||
| OSI before treatment | 26.78 ± 5.31 | 26.29 ± 6.63 | 0.797 |
| OSI at 6 months | 19.21 ± 9.67 | 18.58 ± 13.43 | 0.864 |
| Mean reduction in OSI with treatment | 7.57 ± 7.34 | 7.71 ± 8.68 | 0.956 |
| WSO | |||
| OSI before treatment | 11.42 ± 6.60 | 16.20 ± 8.29 | 0.22 |
| OSI at 6 months | 3.0 ± 5.19 | 2.80 ± 3.67 | 0.92 |
| Mean reduction in OSI with treatment | 8.42 ± 6.52 | 13.40 ± 6.36 | 0.13 |
| Author | No. of patients | Treatment protocol | Assessment tool | Result | |
|---|---|---|---|---|---|
| Zhou et al. | 29 (115 nails) | Fractional CO2 laser and 1% luliconazole cream for 6 months | 12 sessions at 2-week intervals Follow up at 6 months |
Clinical efficacy rate and mycological clearance rate | 92% showed response 34% complete response 8% no response |
| Bhatta et al.11 | 75 (356 nails) | Fractional CO2 laser and 1% terbinafine cream for 3 months | 3 sessions at 4-week intervals Follow up at 6 months |
Scoring Clinical Index for Onychomycosis | 80% showed response 33% complete response 20% no response |
| Shi et al.12 | 30 (124 nails) | Fractional CO2 laser and 1% terbinafine cream for 6 months | 12 sessions at 2-week intervals Follow up at 6 months |
Clinical efficacy rate and mycological clearance rate | 68.5% showed response |
| Lim et al.13 | 24 (119 nails) | Fractional CO2 laser and amorolfine cream for 3 months | 3 sessions at 4-week intervals Follow up at 6 months |
Clinical efficacy rate (based on area of involvement) | 92% showed response 50% completeresponse 8% no response |
| Arora et al.14 | 26 (50 nails) | Fractional CO2 laser and 1% terbinafine cream for 6 months | 3 sessions at 4-week intervals Follow up at 6 months |
Onychomycosis Severity Index | 88% showed response |
| Zaki et al.15 | 40 | Fractional CO2 laser and topical tioconazole 28% solution for 16 weeks | Five sessions at 3-weeks interval Follow up at 4 months |
Scoring Clinical Index for Onychomycosis | 95% showed response |

- Right great toenail with onychomycosis treated with fractional CO2 laser combined with 1% terbinafine cream (a) before treatment (b) after 4 months (c) at 6 months

- Right great toenail with onychomycosis treated with fractional CO2 laser combined with 1% terbinafine cream (a) before treatment (b) after 4 months (c) at 6 months
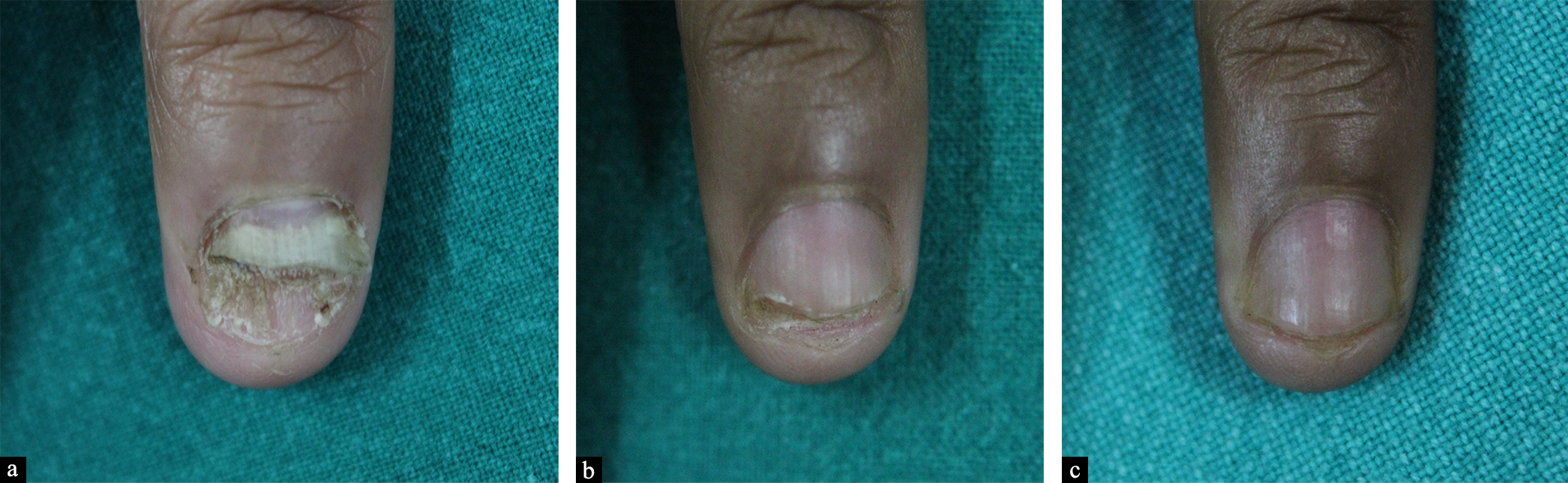
- Fingernail with onychomycosis treated with capsule itraconazole (a) before treatment (b) after 4 months (c) at 6 months

- Right thumbnail with onychomycosis treated with capsule itraconazole (a) before treatment (b) after 4 months (c) at 6 months
Similarly, in the fingernails of study subjects of fractional carbon dioxide and itraconazole groups, the means of Onychomycosis Severity Index scores were lower in the itraconazole group compared to the fractional carbon dioxide group, at baseline and after six months follow-up, the difference in the means among the patients in both the groups were not statistically significant (P > 0.05). However, improvement in terms of decrease in Onychomycosis Severity Index was higher in the fractional carbon dioxide arm but it was not found to be statistically significant [Table 3].
Also, all types of onychomycosis responded to fractional carbon dioxide with topical terbinafine, as well as itraconazole as assessed by a decrease in Onychomycosis Severity Index. The response was found to be statistically significant in both groups [Table 3].
Discussion
Onychomycosis is known to be difficult to treat. Reported cure rates for combination treatment with both topical and systemic antifungals range from 59.2 to 88.2%.17 Antifungal drugs are contraindicated in active liver, renal diseases and long-term treatment leads to poor patient compliance. This has led to the need for non-pharmacologic treatment modalities for rapid treatment of nail infection. Laser therapy for onychomycosis, although described, is yet to be recognised as a treatment modality. It is thought that the fungal elements get decomposed by heat because temperatures exceeding 50°C lead directly to thermal killing.18 Further fungicidal effect is achieved through the absorption of energy by fungal chromophores like xanthomegnin, chitin and melanin.
Bhatta et al.11 Lim et al.13 and Arora et al.14 also conducted a clinical trial using multiple sessions of fractional carbon dioxide laser along with a topical antifungal agent. Treatment of onychomycosis by urea occlusion prior to a single session of fractional carbon dioxide laser has also been reported.19 Lim et al.13 reported that 71% of participants (17 participants) had full or >60% normal-appearing nails at three months after the last treatment. Bhatta et al.11 reported that 73.32% of participants (55 participants) had fully or >60% normal-appearing nails. However, a validated objective score was not used for assessment in these studies. Arora et al.14 also used Onychomycosis Severity Index for assessment of onychomycosis and reported improvement in 88% of nails (44 nails) with a significant reduction in Onychomycosis Severity Index at the end of six months. In the present study, the efficacy of fractional carbon dioxide laser along with 1% terbinafine cream was compared with capsule itraconazole among 100 cases of onychomycosis. Similar to the previous reported studies, we found that fractional carbon dioxide laser along with 1% terbinafine cream was effective in 84.7% of nails. Not only it was effective in achieving nail plate clearance in onychomycosis, but it also had similar efficacy to oral itraconazole.
Clinico-epidemiologic characteristics
Gender and age distribution among the two study arms was found to be similar to previous studies11,12 [Table 2]. Most of the nails involved in both groups were toenails [Table 2]. This was found to be similar to studies by Bhatta et al.11 and Zhou et al.10
Types of onychomycosis
Most common type of onychomycosis found in our study was distal lateral subungual onychomycosis, 69.4% and 80.1% in fractional carbon dioxide laser arm and itraconazole arm, respectively. Lim et al.13 also found distal lateral subungual onychomycosis and total dystrophic onychomycosis to be the most common type of onychomycosis in their study.
Onychomycosis Severity Index
Mean Onychomycosis Severity Index scores in fractional carbon dioxide group and itraconazole group at baseline were 17.06 ± 9.66 and 16.92 ± 9.59, respectively. This is similar to a study by Zhou et al.10 who also used Onychomycosis Severity Index as a measure of severity of onychomycosis and found a baseline Onychomycosis Severity Index of 18.0 ± 11.5 and 16.6 ± 10.6 in two study groups. Mean Onychomycosis Severity Index scores in the fractional carbon dioxide group and itraconazole group at six months after treatment initiation were 8.40 ± 9.76 and 9.55 ± 9.79, respectively. Significant improvement in terms of reduction in the Onychomycosis Severity Index was found in both arms. It was higher in the fractional carbon dioxide arm (8.65 ± 7.09) as compared to the itraconazole arm (7.36 ± 6.65). However, this was not found to be statistically significant with P -value of 0.157 (P > 0.05) [Table 3]. Our study showed considerable improvement post-treatment in both groups when compared with the baseline. However, the difference between the two groups was statistically insignificant.
A few patients experienced mild pain during laser treatment. There was no bleeding or oozing during or after treatment. No adverse effects were reported during the observation period. Similar effects were seen in previous studies by Zhou et al.10 and Bhatta et al.11 Two patients in the itraconazole arm had side effects of nausea and diarrhoea and dropped out of the study.
Limitations
The major limitations of our study were the small sample size and unavailability of long-term follow-up data. The main limitation of fractional carbon dioxide laser is the high cost and low availability of treatment as compared to itraconazole.
Conclusion
Fractional carbon dioxide laser along with 1% terbinafine cream and capsule itraconazole are both significantly effective in the management of onychomycosis. The efficacy of fractional carbon dioxide laser along with 1% terbinafine cream is comparable to oral itraconazole alone, with no statistically significant difference. However, patients treated with fractional carbon dioxide laser along with 1% terbinafine cream did not show any adverse effects and had better satisfaction and compliance as compared to the itraconazole group. Hence, fractional carbon dioxide laser along with 1% terbinafine cream seems to be a promising therapy that can lead to results similar to the gold standard agent itraconazole with no significant and serious adverse effects.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Dermatophytoses in a desert district of western Rajasthan. Indian J Dermatol Venereol Leprol. 1995;61:280-3.
- [PubMed] [Google Scholar]
- Clinical and mycological study of superficial fungal infections at Government General Hospital: Guntur and their response to treatment with Hamycin, Dermostatin and Dermamycin. Indian J Dermatol Venereol. 1970;36:209-14.
- [PubMed] [Google Scholar]
- Onychomycosis: Pathogenesis, diagnosis, and management. Clin Microbiol Rev. 1998;11:415-29.
- [CrossRef] [PubMed] [Google Scholar]
- Mycology of nail disorders. J Am Acad Dermatol. 1994;31:S68-74.
- [CrossRef] [PubMed] [Google Scholar]
- The use of oral antifungal agents to treat onychomycosis. Dermatol Clin. 2003;21:469-79.
- [CrossRef] [PubMed] [Google Scholar]
- A double-blind, randomized study comparing itraconazole pulse therapy with continuous dosing for the treatment of toe-nailonychomycosis. Br J Dermatol. 1997;136:230-4.
- [PubMed] [Google Scholar]
- Onychomycosis and diabetes. J Eur Acad Dermatol Venereol. 2009;23:1119-22.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomycosis: Treatment and prevention of recurrence. J Am Acad Dermatol. 2019;80:853-67.
- [CrossRef] [PubMed] [Google Scholar]
- The efficacy of fractional carbon dioxide (CO2) laser combined with luliconazole 1% cream for the treatment of onychomycosis: A randomized, controlled trial. Medicine (Baltimore). 2016;95:e5141.
- [CrossRef] [PubMed] [Google Scholar]
- Fractionaldioxide (CO2) laser-assisted topical therapy for the treatment of onychomycosis carbon dioxide. J Am Acad Dermatol. 2016;74:916-23.
- [CrossRef] [PubMed] [Google Scholar]
- The efficacy of fractional carbon dioxide (CO2) laser combined with terbinafine hydrochloride 1% cream for the treatment of onychomycosis. J Cosmet Laser Ther. 2017;19:353-9.
- [CrossRef] [PubMed] [Google Scholar]
- Toenail onychomycosis treated with a fractionallaser and topical antifungal cream carbon dioxide. J Am Acad Dermatol. 2014;70:918-23.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional CO2 laser in the management of onychomycosis. J Mar Med Soc. 2020;22:50-3.
- [CrossRef] [Google Scholar]
- Fractional CO2 laser plus topical antifungal versus fractional CO2 laser versus topical antifungal in the treatment of onychomycosis. Dermatol Ther. 2020;33(1):e13155..
- [CrossRef] [PubMed] [Google Scholar]
- A new classification system for grading the severity of onychomycosis: Onychomycosis Severity Index. Arch Dermatol. 2011;147:1277-82.
- [CrossRef] [PubMed] [Google Scholar]
- A multicentre, randomized, controlled study of the efficacy, safety and cost-effectiveness of a combination therapy with amorolfine nail lacquer and oral terbinafine compared with oral terbinafine alone for the treatment of onychomycosis with matrix involvement. Br J Dermatol. 2007;157:149-57.
- [CrossRef] [PubMed] [Google Scholar]
- New therapeutic options in the management of superficial fungal diseases. Dermatol Ther 2019:e12855.
- [CrossRef] [PubMed] [Google Scholar]
- Urea occlusion prior to single session fractional CO2 laser as a treatment in onychomycosis. Indian J Dermatol Venereol Leprol. 2020;86:331-33.
- [CrossRef] [PubMed] [Google Scholar]






