Translate this page into:
Fractional lasers in dermatology - Current status and recommendations
2 Manipal Hospital, Bangalore, India
3 Skin and Laser Clinic, Begumpet Hyderabad, India
4 Department of Dermatology, Adichunchanagiri Institute of Medical Sciences, BG Nagara, Karnataka, India
5 VIkram Perfect Clinic, Mysore, India
6 Venkat Charmalaya - Centre for Advanced Dermatology, Bangalore, India
Correspondence Address:
Venkataram Mysore
Department of Dermatology, Venkat Charmalaya - Centre for Advanced Dermatology, 3437, 1st G cross, 7th Main, Subbanna Garden, Vijay Nagar, Bangalore - 560 040
India
| How to cite this article: Goel A, Krupashankar D S, Aurangabadkar S, Nischal K C, Omprakash H M, Mysore V. Fractional lasers in dermatology - Current status and recommendations. Indian J Dermatol Venereol Leprol 2011;77:369-379 |
Abstract
Introduction: Fractional laser technology is a new emerging technology to improve scars, fine lines, dyspigmentation, striae and wrinkles. The technique is easy, safe to use and has been used effectively for several clinical and cosmetic indications in Indian skin.Devices: Different fractional laser machines, with different wavelengths, both ablative and non-ablative, are now available in India. A detailed understanding of the device being used is recommended. Indications: Common indications include resurfacing for acne, chickenpox and surgical scars, periorbital and perioral wrinkles, photoageing changes, facial dyschromias. The use of fractional lasers in stretch marks, melasma and other pigmentary conditions, dermatological conditions such as granuloma annulare has been reported. But further data are needed before adopting them for routine use in such conditions. Physician qualification: Any qualified dermatologist may administer fractional laser treatment. He/ she should possess a Master's degree or diploma in dermatology and should have had specific hands-on training in lasers, either during postgraduation or later at a facility which routinely performs laser procedures under a competent dermatologist or plastic surgeon with experience and training in using lasers. Since parameters may vary with different systems, specific training tailored towards the concerned device at either the manufacturer's facility or at another center using the machine is recommended. Facility: Fractional lasers can be used in the dermatologist's minor procedure room for the above indications. Preoperative counseling and Informed consent: Detailed counseling with respect to the treatment, desired effects and possible postoperative complications should be provided to the patient. The patient should be provided brochures to study and also adequate opportunity to seek information. A detailed consent form needs to be completed by the patient. Consent form should include information on the machine, possible postoperative course expected and postoperative complications. Preoperative photography should be carried out in all cases of resurfacing. A close-up front and 45-degree lateral photographs of both sides must be taken. Laser parameters: There are different machines based on different technologies available. Choice parameters depend on the type of machine, location and type of lesion, and skin color. Physician needs to be familiar with these requirements before using the machine. Anesthesia: Fractional laser treatment can be carried out under topical anesthesia with eutectic mixture of lidocaine and prilocaine. Some machines can be used without any anesthesia or only with topical cooling or cryospray. But for maximal patient comfort, a topical anesthetic prior to the procedure is recommended. Postoperative care: Proper postoperative care is important in avoiding complications. Post-treatment edema and redness settle in a few hours to a few days. A sunscreen is mandatory, and emollients may be prescribed for the dryness and peeling that could occur.
Introduction
The field of laser resurfacing for esthetic enhancement continues to improve with new developments since the 1980s. Fractional photothermolysis (FP) has revolutionized the use of lasers for resurfacing. Much variation exists with different machines and techniques, and newer indications are being described for these technologies. It is necessary, therefore, to examine current available evidence and make appropriate recommendations based on the evidence. It is emphasized hereby that this technology is new and rapidly evolving; therefore, this review and recommendations made in it are based on the evidence available so far and may need to be reviewed periodically as technology evolves.
The laser-resurfacing industry has produced a multitude of devices employing ablative, non-ablative and fractional technologies. The three approaches largely differ in their method of thermal damage, degrees of efficacy, downtime and side effect profiles against each other. Ablative technologies have been seen to have higher incidences of side effects, especially in darker skin types. Non-ablative technologies generated some interest, but the results were mild and slow. Recently fractional laser technology is gaining wide popularity because of its favorable side effect profile, reduced recovery time and significant clinical outcome. [1]
Fractional laser technology represents a major advantage over the previous conventional ablative methods (CO 2 and erbium:YAG lasers). [2],[3] Ablative lasers had the advantages of predictability in the depth of tissue ablation and thermal denaturation. Erbium:YAG laser represented an improvement on the CO 2 laser in producing lesser downtime. However, traditional ablative laser resurfacing suffered from several disadvantages, such as the need for effective anesthesia; prolonged downtime; the risk of dyspigmentation and scarring, particularly in darker skin types; the need for intensive postoperative care; the long-lasting erythema; and the need for prolonged avoidance of sun exposure after treatment. These drawbacks were sought to be overcome by fractional laser technology. [4],[5]
References
- Brightman LA, Brauer JA, Anolik R, Weiss E, Karen J, Chapas A, et al. Ablative and fractional ablative lasers. Dermatol Clin 2009;27:479-89.
- Fitzpatrick RE, Goldman MP, Satur NM, Tope WD. Pulsed carbon dioxide laser resurfacing of photoaged facial skin. Arch Dermatol 1996;132:395-402.
- Alexiades-Armenakas MR, Dover JS, Arndt KA. The spectrum of laser skin resurfacing: Nonablative, fractional, and ablative laser resurfacing. J Am Acad Dermatol 2008;58:719-37.
- Alexiades-Armenakas MR. What is new in lasers and cosmetic procedures from the 2007 AAD annual meeting. J Drugs Dermatol 2007;6:464.
- Susan W, Brian ST, James C, Gregory A, Andrei E, Ilya Y, et al. Fractional photothermolysis: A novel aesthetic laser surgery modality. Dermatol Surg 2007;33:525-34.
Principle of Fractional Photothermolysis
Manstein and colleagues introduced the concept of fractional photothermolysis (FP) in 2004. [1] Their FP device emitted light in a pixilated fashion and transmitted it to the skin, producing an array of microthermal zones (MTZs) and creating small microscopic columns of thermal injury to the skin. [1] Fractional resurfacing thermally ablates microscopic columns of epidermal and dermal tissue in regularly spaced arrays over a fraction of the skin surface; in contrast to ablative skin resurfacing, in which a confluent, uniform patch of epidermal or dermal injury is induced. [2],[3] Fractional photothermolysis therefore denotes induction of thermal alteration of a fraction or a column of skin, leaving intervening areas of normal skin untouched, which rapidly repopulate the ablated columns of tissue. [2],[3] The number, depth and size of these vertical columns of MTZs are variable and depend on the type of machine, wavelength of the laser used, fluence and the number of stackings or applications of laser. These zones comprise approximately 15% to 25% of the skin surface area per treatment session. The diameter of each MTZ is and ranges from 100 to 160 ΅. At the energies commonly used for facial rejuvenation (8-12 mJ/MTZ), the depth of penetration ranges from 300 to 700 ΅. The density of MTZs is adjustable, and typically, a final density of 2,000 MTZs/cm 2 is delivered at each treatment, a density corresponding to approximately 20% of the surface area of the skin. The resulting dermal-epidermal debris are incorporated into the columns of microscopic epidermal necrotic debris (MENDs) and eliminated by the phenomenon of transepidermal elimination. [2],[3],[4] Subsequently, there is stimulation of re-epithelialization and repair mediated by the adjacent columns of intact tissue. Similar to ablative laser resurfacing, the areas of thermally ablated tissue are repopulated by fibroblast-derived neocollagenogenesis and epidermal stem cell reproduction. Non-ablative fractional lasers too operate through a similar principle of the creation of microthermal zones of damage to the treated tissue, but without ablation of epidermis, extrusion of dermal contents, and rapid resurfacing.
Since a large percentage of intervening skin is unaffected, healing occurs quickly, thereby minimizing the downtime. At each subsequent session, such fractions are treated; and over 2 to 6 sittings, treatment is completed. [5] The advantages claimed for fractional lasers include reduced postoperative edema and erythema, minimum downtime, reduced dyschromic changes and, importantly, suitability for darker skin types. Neither non-ablative nor fractional resurfacing produces results comparable to ablative laser skin resurfacing, but both have become much more popular than the latter because of lesser downtime and better patient compliance.
References
- Manstein D, Herron GS, Sink RK, Tanner H, Anderson RR. Fractional photothermolysis: A new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med 2004;34:426-38.
- Hantash BM, Bedi VP, Sudireddy V, Struck SK, Herron GS, Chan KF. Laser-induced transepidermal elimination of dermal content by fractional photothermolysis. J Biomed Opt 2006;11:041115.
- Walgrave S, Zelickson B, Childs J, Altshuler G, Erofeev A, Yaroslavsky I, et al. Pilot investigation of the correlation between histological and clinical effects of infrared fractional resurfacing lasers. Dermatol Surg 2008;34:1443-53.
- Trelles MA, Velez M, Mordon S. Correlation of histological findings of single session er:yag skin fractional resurfacing with various passes and energies and the possible clinical implications. Lasers Surg Med 2008;40:174-7.
- Susan W, Brian BC, Gregory A, Andrei E, Ilya Y. Fractional photothermolysis: A novel aesthetic laser surgery modality. Dermatol Surg 2007;33:525-34.
Technology and Information about Different Machines
This is a rapidly advancing field and several machines continue to be introduced, with varying claims of efficacy and safety by the manufacturers. However, controlled data as evidence for their efficacy may not always be available, and their final status will be confirmed by their performance in due course of time.
As stated earlier, both non-ablative and ablative fractional lasers are available. [1],[2],[3] Both these technologies have their respective advocates. [Table - 1] lists commonly used machines and their specifications. However, the list mentioned in [Table - 1] is not claimed to be inclusive of all models currently available in the market. It is not the mandate of the task force to make recommendations for individual machines. Hence a prospective buyer should carefully look at different parameters before making a choice. The task force suggests that the following parameters should be considered while choosing a fractional laser machine:

- Ability to deliver higher fluencies per micro-beam
- Variable microthermal zone (MTZ) settings-density of the micro-beams
- Variable micro-beam sizes
- Ability to choose various shapes for treatment so as to fit properly on the face
- Ease of use
- Degree of procedural pain or discomfort
- Ability to alter micro-beam density, size and fluence
- Number of treatment sessions required to attain clinical endpoints
- Patient downtime
- Treatment duration
- Clinical validation of the product
References
- Alexiades-Armenakas MR, Dover JS, Arndt KA. The spectrum of laser skin resurfacing: Nonablative, fractional, and ablative laser resurfacing. J Am Acad Dermatol 2008;58:719-37.
- Tierney EP, Kouba DJ, Hanke CW. Review of fractional photothermolysis: treatment indications and efficacy. Dermatol Surg 2009;35:1445-61.
- Hantash BM, Mahmood MB. Fractional photothermolysis: A novel aesthetic laser surgery modality. Dermatol Surg 2007;33:525-34.
Indications for Fractional Laser Treatment
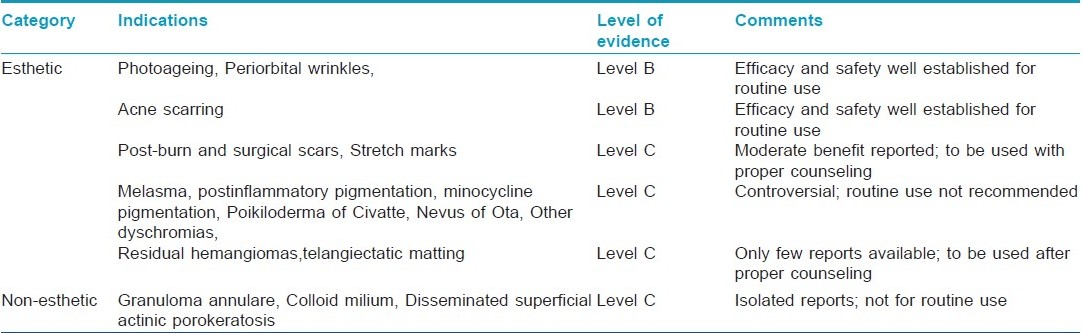
Fractional lasers have been used for a number of conditions, because of their remarkable safety profile. [Table - 2] indicates the list of conditions for which fractional lasers have been reported to be effective. The list of indications continues to grow, with several new applications being reported. While some indications such as ageing skin, wrinkles, acne scars have a number of supporting studies with higher levels of evidence, others such as poikiloderma of Civatte, stretch marks, milium need further validation.
1. Ageing and photo-damaged skin
Mild-to-moderate facial wrinkles and periorbital wrinkles constitute important indications for fractional laser treatment. [1] Both fractional ablative and non-ablative lasers can be used for the treatment of mild-to-moderate lines and wrinkles. [1],[2] Multiple treatments at intervals of 1 month are needed to achieve satisfactory improvement. Fractional lasers can also be used effectively for the treatment of photo-damaged skin. [3],[4],[5],[6],[7] Greater improvement has been reported in rhytides; and in fine lines as compared to deep lines. Ablative fractional lasers have been reported to produce greater textural improvement and dermal remodeling simultaneously and to produce significant improvement in dyschromias too. Lapidoth reported the efficacy of ablative fractionated Er:YAG laser (2,940 nm) in treatment of photo-aging. [8] Weiss et al.[9] reported a greater efficacy for fractional CO 2 laser than 1,550-nm erbium laser in a comparative split-face trial. A comparative split-face trial with fractional Er:YAG and microfractional CO 2 laser resurfacing showed greater efficacy and patient satisfaction for the fractional CO 2 laser. [10] However, the Er:YAG-treated side required a lesser healing time and had lesser crusting. Foster and colleagues recently reported the efficacy of a dual-wavelength device (1,320 and 1,440 nm), with benefits in the treatment of skin laxity and facial wrinkles. [11]
References
- Rahman Z, Alam M, Dover JS. Fractional laser treatment for pigmentation and texture improvement. Skin Therapy Lett 2006;11:7-11.
- Bass LS. Rejuvenation of the aging face using fraxel laser treatment. Aesthet Surg J 2005;25:307-9.
- Geronemus R. Fractional photothermolysis: Current and future applications. Lasers Surg Med 2006;38:169-76.
- Jih MH, Goldberg LH, Kimyai-Asadi A. Fractional photothermolysis for photoaging of hands. Dermatol Surg 2008;34:73-8.
- Wanner M, Tanzi EL, Alster TS. Fractional photothermolysis: Treatment of facial and nonfacial cutaneous photodamage with a 1,550-nm erbium-doped fiber laser. Dermatol Surg 2007;33:23-8.
- Rahman Z, Alam M, Dover JS. Fractional laser treatment for pigmentation and texture improvement. Skin Therapy Lett 2006;11:7-11.
- Mezzana P, Valeriani M. Rejuvenation of the aging face using fractional photothermolysis and intense pulsed light: A new technique. Acta Chir Plast 2007;49:47-50.
- Lapidoth M, Yagima Odo ME, Odo LM. Novel use of erbium: YAG (2,940-nm) laser for fractional ablative photothermolysis in the treatment of photodamaged facial skin: A pilot study. Dermatol Surg 2008;34:1048-53.
- Weiss R, Weiss M, Beasley K. Prospective split-face trial of a fixed spacing array computed scanned fractional CO2 laser versus hand scanned 1550nm fractional for rhytides. Abstract presented at American Society for Laser Medicine and Surgery Conference, April 2008, Kissimmee, FL.
- Lomeo G, Cassuto D, Scrimali L, Sirago P. Er: YAG versus CO2 ablative fractional resurfacing: A split face study. Abstract presented at American Society for Laser Medicine and Surgery Conference, April 2008, Kissimmee, FL.
- Foster KW, Kouba DJ, Fincher EE, Glicksman ZS, Hayes J, Valerie F, et al. Early improvement in rhytides and skin laxity following treatment with a combination fractional laser emitting two wavelengths sequentially. J Drugs Dermatol 2008;7:108-11.
2. Post-acne scars and other scars
a) Post-acne scars
Management of acne scars presents a challenge for any clinician. Treatment of acne scars depends on the type and severity of scarring. Though several treatment options are available, results are not fully satisfactory. Fractional lasers have been used successfully and safely in the treatment of acne scars with good results in superficial and medium-depth scars, and represent a significant advance in the management of this challenging condition. [1],[2],[3],[4],[5],[6],[7],[8],[9],[10] Improvement has also been reported in pores, an otherwise difficult condition to treat. [11] While macular, superficial and medium-depth scars respond well, deep scars and ice-pick scars may improve only marginally. In cases with severe scarring, combination with other approaches such as chemical peels, subcision, surgical dermabrasion, dermaroller and trichloroacetic acid CROSS technique [12] may be needed. In a case series, Chapas and colleagues [9] demonstrated improvements of 26% to 50% in texture and atrophy, as well as overall improvement, in moderate-to-severe acne scarring with fractionated CO2 laser. Fractional non-ablative lasers too have been found to be effective in acne scarring. Geronemus reported initially on the treatment of acne scarring with non-ablative fractional lasers. [6] Alster and colleagues reported a study on 53 patients with atrophic acne scars treated with Fraxel SR (Reliant Technologies, Inc.). [2] After 3 monthly treatments, clinical improvement ranged from 51% to 95%, in 90% of patients. Similar improvements have been reported in other studies by Lee et al. [7] in Asian patients and by Glaich et al. [8] Glaich reported 2 cases of treatment of marked atrophic acne scarring and postinflammatory erythema with FP. Marked improvement was noted in the postinflammatory erythema after 1 treatment session. Significant improvement in the atrophic acne scars was noted 3 months after a series of 5 FP treatments.
Because of its safety profile and greater tolerance, fractional laser technology has become an increasingly popular treatment modality to treat acne scarring in individuals of darker skin types, including Indian skin, in which the conventional ablative laser treatments and surgical treatment modalities carry the risk of permanent postinflammatory hyperpigmentation. Despite the reported safety of fractional lasers in post-acne scarring, there is still the possibility for transient erythema or edema, dryness, scabbing, milia or acne, hyperpigmentation or hypopigmentation, prolonged healing, or infection. [13] Hence proper counseling of patients and appropriate adjuvant medical treatment are essential.
References
-
Hasegawa T, Matsukura T, Mizuno Y, Suga Y, Ogawa H, Ikeda S. Clinical trial of a laser device called fractional photothermolysis system for acne scars. J Dermatol 2006;33:623-7.
- Alster TS, Tanzi EL, Lazarus M. The use of fractional laser photothermolysis for the treatment of atrophic scars. Dermatol Surg 2007;33:295-9.
- Gold M, Gold MH, Heath AD, Biron JA. Clinical evaluation of the SmartSkin fractional laser for the treatment of photodamage and acne scars. J Drugs Dermatol 2009;8:s4-8.
- Hu S, Chen MC, Lee MC, Yang LC, Keoprasom N. Fractional resurfacing for the treatment of atrophic facial acne scars in asian skin. Dermatol Surg 2009;35:826-32.
- Rahman Z, Tanner H, Jiang K. Treatment of atrophic scars with the 1550nm erbium-fiber fractional laser. Lasers Surg Med 2006;38:24.
- Geronemus R. Fractional photothermolysis: current and future applications. Lasers Surg Med 2006;38:169-76.
- Lee HS, Lee JH, Ahn GY, Lee DH, Shin JW, Kim DH, et al. Fractional photothermolysis for the treatment of acne scars: A report of 27 Korean patients. J Dermatolog Treat 2008;19:45-9.
- Glaich AS, Goldberg LH, Friedman RH, Friedman PM. Fractional photothermolysis for the treatment of postinflammatory erythema resulting from acne vulgaris. Dermatol Surg 2007;33:842-6.
- Chapas AM, Brightman L, Sukal S, Hale E, Daniel D, Bernstein LJ, et al. Successful treatment of acneiform scarring with CO2 ablative fractional resurfacing. Lasers Surg Med 2008;40:381-6.
- Kim S. Clinical trial of a pinpoint irradiation technique with the CO2 laser for the treatment of atrophic acne scars. J Cosmet Laser Ther 2008;29:1-4.
- Cho SB, Lee JH, Choi MJ, Lee KY, Oh SH. Efficacy of the fractional photothermolysis system with dynamic operating mode on acne scars and enlarged facial pores. Dermatol Surg 2009;35:108-14.
- Kim HJ, Kim TG, Kwon YS, Park JM, Lee JH. Comparison of a 1,550 nm Erbium: Glass fractional laser and a chemical reconstruction of skin scars (CROSS) method in the treatment of acne scars: a simultaneous split-face trial. Lasers Surg Med 2009;41:545-9.
- Rivera AE. Acne scarring: A review and current treatment modalities. J Am Acad Dermatol 2008;59:659-76.
b) Surgical scars
Surgical, post-traumatic and burn scars can also be treated with fractional lasers. [1],[2],[3] Multiple treatments lead to improvement in texture, quality and pigmentation of the scars in both atrophic and hypertrophic types. However, atrophic and pigmented scars tend to improve better than the hypertrophic scars.
In a case report, Behroozan and colleagues noted 75% overall improvement in a surgical scar on the chin after a single treatment with the 1,550-nm Fraxel SR. [4] Glaich et al. [5] demonstrated 51% to 75% improvement in hypopigmented facial scars in 6 of the 7 treated patients, by using 1,550-nm Fraxel SR. In a study performed by Tierney et al., [6] fractional photothermolysis (using 1,550-nm fractionated erbium laser - Fraxel SR, Reliant Technologies, Inc.) was found to be more effective than pulse dye laser (Candela Corporation Inc., Wayland, MA) for the cosmetic improvement of surgical scars.
c) Burn scar
A single report on the efficacy of FP in burn scar has been published, and this indication therefore needs further study. [7]
References
-
Haedersdal M, Moreau KE, Beyer DM, Nymann P, Alsbjψrn B. Fractional nonablative 1540 nm laser resurfacing for thermal burn scars: A randomized controlled trial. Lasers Surg Med 2009;41:189-95.
- Lee Y. Combination treatment of surgical, post-traumatic and post-herpetic scars with ablative lasers followed by fractional laser and non-ablative laser in Asians. Lasers Surg Med 2009;41:131-40.
- Niwa AB, Mello AP, Torezan LA, Osprio N. Fractional Photothermolysis for the Treatment of Hypertrophic Scars: Clinical Experience of Eight Cases. Dermatol Surg 2009;35:773-8.
- Behroozan DS, Goldberg LH, Dai T, Geronemus RG, Friedman PM. Fractional photothermolysis for the treatment of surgical scars: A case report. J Cosmet Laser Ther 2006;8:35-8.
- Glaich AS, Rahman Z, Goldberg LH, Friedman PM. Fractional resurfacing for the treatment of hypopigmented scars: A pilot study. Dermatol Surg 2007;33:289-94.
- Tierney E, Mahmoud BH, Srivastava D, Ozog D, Kouba DJ. Treatment of surgical scars with fractional photothermolysis versus pulse dye laser: Randomized control trial. Dermatol Surg 2009;35:1172-80.
- Waibel J, Beer K. Fractional laser resurfacing for thermal burns. J Drugs Dermatol 2008;7:59-61.
3. Stretch marks (Striae)
Management of striae has remained a challenge, and hitherto no satisfactory treatment has been reported. Recent reports suggest that fractional photothermolysis may improve striae, with improvement in texture, and dyschromia [1,2] ; however, these findings are preliminary and need to be reproduced in larger and controlled studies.
References
- Stotland M, Chapas AM, Brightman L, Sukal S, Hale E, Karen J, et al. The safety and efficacy of fractional photothermolysis for the correction of striae distensae. J Drugs Dermatol 2008;7:857-61.
- Kim BJ, Lee DH, Kim MN, Song KY, Cho WI, Lee CK, et al. Fractional photothermolysis for the treatment of striae distensae in Asian skin. Am J Clin Dermatol 2008;9:33-7.
4. Pigmentary disorders
a) Melasma
Fractional lasers have been used successfully in the management of melasma and postinflammatory pigmentation in a number of studies. [1],[2],[3] Rokhsar and Fitzpatrick published an initial report on the efficacy of FP for the treatment of melasma. [2] After 4 to 6 treatment sessions, 60% of treated patients (n= 10) achieved 75% to 100% clearance, with only 30% of patients demonstrating less than 25% improvement. Only 1 of the 10 patients reported postinflammatory hyperpigmentation (which resolved within 3 months of treatment). Goldberg and colleagues [3] treated 10 melasma patients (skin types III-IV), with a total of 4 treatments at 2-week intervals, using a non-ablative fractional photothermolysis (FP) device (Fraxel SR 750). By both light microscopy and electron microscopy, post-treatment specimens demonstrated a relative decrease in melanocytes. Six patients with skin type III had good improvement, whereas 4 patients with skin type IV had only fair improvement.
Manstein et al.[4] established the possible mechanism for the above-reported efficacy of fractional photothermolysis in melasma - that MTZ creation and tissue destruction by FP results in elimination of melanocytes- and keratinocytes-containing melanin granules through a "melanin shuttle." This melanin shuttle formation results in significant improvement in epidermal and dermal pigmentation associated with conditions such as melasma and dyschromia of photoageing.
However, more recent publications have reported the limitations of FP with regard to its efficacy in the treatment of melasma, especially in patients with darker skin types, with more modest improvement rates and high recurrence rates after treatment. [5] This should therefore lead to a proper reappraisal of the possible benefit of FP in melasma. As would be expected in a chronic, recurrent condition such as melasma, response to treatment is variable, pigmentation frequently recurs and postinflammatory pigmentation is common in patients with darker skin. For these reasons, lasers are not routinely recommended as the treatment of choice for treating melasma in Indian patients. Further studies need to be carried out before fractional lasers can be recommended for routine treatment of melasma in darker skin types.
References
- Tannous SZ, Astner S. Utilizing fractional resurfacing in the treatment of therapy resistant melasma. J Cosmet Laser Ther 2005;7:39-43.
- Rokhsar CK, Fitzpatrick RE. The treatment of melasma with fractional photothermolysis: A Pilot study. Dermatol Surg 2005;31:1645-50.
- Goldberg DJ, Berlin AL, Phelps R. Histologic and ultrastructural analysis of melasma after fractional resurfacing. Lasers Surg Med 2008;40:134-8.
- Manstein D, Herron GS, Sink RK, Tanner H, Anderson RR. Fractional photothermolysis: A new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med 2004;34:426-38.
- Naito SK. Fractional photothermolysis treatment for resistant melasma in Chinese females. J Cosmet Laser Ther 2007;9:161-3.
b) Other pigmentary disorders
Poikiloderma of Civatte (PC), [1] minocycline-induced pigmentation, [2] nevus of Ota [3] and postinflammatory pigmentation [4] have been treated by FP. Ablative fractional laser was found to be both safe and effective for the treatment of the vascular, pigmentary and textural components of PC. [1]
References
- Tierney EP, Hanke CW. Treatment of Poikiloderma of Civatte with ablative fractional laser resurfacing: Prospective study and review of the literature. J Drugs Dermatol 2009;8:527-34.
- Izikson L, Anderson RR. Resolution of blue minocycline pigmentation of the face after fractional photothermolysis. Lasers Surg Med 2008;40:399-401.
- Kouba DJ, Fincher EF, Moy RL. Nevus of Ota successfully treated by fractional photothermolysis using a fractionated 1440-nm Nd: YAG laser. Arch Dermatol 2008;144:156-8.
- Rokhsar CK, Ciocon DH. Fractional Photothermolysis for the Treatment of Postinflammatory Hyperpigmentation after Carbon Dioxide Laser Resurfacing. Dermatol Surg 2009;35:535-7.
5. Miscellaneous indications
Other reported conditions for which FP has been beneficial include residual hemangiomas, [1] telangiectatic matting, [2] granuloma annulare, [3] colloid milium [4] and disseminated superficial actinic porokeratosis. [5]
References
- Blankenship TM, Alster TS. Fractional photothermolysis of residual hemangioma. Dermatol Surg 2008;34:1112-4.
- Glaich AS, Goldberg LH, Dai T, Friedman PM. Fractional photothermolysis for the treatment of telangiectatic matting: A case report. J Cosmet Laser Ther 2007;9:101-3.
- Karsai S, Hammes S, Rόtten A, Raulin C. Fractional photothermolysis for the treatment of granuloma annulare: A case report. Lasers Surg Med 2008;40:319-22.
- Marra DE, Pourrabbani S, Fincher EF, Moy RL. Fractional photothermolysis for the treatment of adult colloid milium. Arch Dermatol 2007;143:572-4.
- Chrastil B, Glaich AS, Goldberg LH, Friedman PM. Fractional photothermolysis: A novel treatment for disseminated superficial actinic porokeratosis. Arch Dermatol 2007;143:1450-2.
Patient Selection and Preoperative Management
Detailed informed consent should be obtained from all patients (Appendix 1).[SUPPORTING:1] Patients should be informed about the nature of treatment, precise procedural details, results expected and the need for multiple sessions. Realistic expectation on the part of the patient should be stressed. Patients with dyspigmentation require 2 to 3 treatments, whereas those with significant rhytides require at least 5 or more treatments. Acne scars may need up to 4 to 6 sessions, depending on the depth, the type of scar and also the machine used. Pre-procedure photography is recommended in all patients before treatment and at each session.
Pre-treatment history
Previous history of herpes labialis; keloid or hypertrophic scar; postinflammatory hyperpigmentation; isotretinoin intake; topical retinoid use; and lidocaine allergy should be noted.
Special considerations
a) Use in darker skin patients: All skin types can be treated with fractional lasers, and the treatment is safe for use in darker skin. However, it should be used with caution in patients with tendency for pigmentation and/ or keloid formation. Proper counseling, priming with depigmenting agents and sunscreens, and initiation of treatment at lower fluences are advised in such patients.
b) All patients for facial resurfacing, with previous history of herpes labialis, should receive prophylactic oral antivirals such as acyclovir, famciclovir or valacyclovir, starting 1 day before fractional resurfacing and continuing for 5 days postoperatively.
c) Oral antibiotics, such as cloxacillin or azithromycin, may be prescribed to patients with a history of bacterial infections of the facial skin to reduce the chance of secondary bacterial infection.
d) While treating patients with melasma and postinflammatory pigmentation, prior priming with sunscreens and depigmenting agents for about 2 to 4 weeks is advised.
e) Pregnancy and lactation: Laser resurfacing in women who are pregnant or lactating, is contraindicated.
f) Isotretinoin and fractional lasers: Care should be exercised in patients with a history of recent isotretinoin use. A 6- to 12-month waiting period following discontinuation of isotretinoin has been recommended before performing resurfacing procedures. [1] This recommendation is based on earlier reports of keloid formation and atypical scar formation after use of dermabrasion and argon lasers, which are more invasive and ablative procedures. [2],[3],[4],[5] However, several recent publications have documented the safety of different procedures such as laser hair removal and dermabrasion in patients recently treated with isotretinoin. [6],[7],[8],[9],[10] A paper by Bagatin [11] suggested that "The current recommendation to wait 6 to 12 months after treatment with oral isotretinoin for acne scar revision using dermabrasion should be re-evaluated. Abrasion of a small test area may be a useful predictor of wound healing, enabling earlier acne scar treatment using this procedure." Therefore, studies and published data on Indian skin are needed to make proper recommendations in this matter.
References
- Rivera AE. Acne scarring: A review and current treatment modalities. J Am Acad Dermatol 2008;59:659-76.
- Dogan G. Possible isotretinoin-induced keloids in a patient with Behηet′s disease. Clin Exp Dermatol 2006;31:535-7.
- Rubenstein R, Roenigk HH Jr, Stegman SJ, Hanke CW. A typical keloids after dermabrasion of patients taking isotretinoin. J Am Acad Dermatol 1986;15:280-5.
- Katz BE, Mac Farlane DF. Atypical facial scarring after isotretinoin therapy in a patient with previous dermabrasion. J Am Acad Dermatol 1994;30:852-3.
- Peteiro C, Toribio J. Keloid formation induced by isotretinoin therapy. Int J Dermatol 1999;38:228-9.
- Cassano N, Arpaia N, Vena GA. Diode laser hair removal and isotretinoin therapy. Dermatol Surg 2005;31:380-1.
- Khatri KA, Garcia V. Light-assisted hair removal in patients undergoing isotretinoin therapy. Dermatol Surg 2006;32:875-7.
- Khatri KA. Diode laser hair removal in patients undergoing isotretinoin therapy. Dermatol Surg 2004;30:1205-7.
- Khatri KA. The safety of long-pulsed Nd:YAG laser hair removal in skin types III-V patients during concomitant isotretinoin therapy. J Cosmet Laser Ther 2009;11:56-60.
- Roenigk HH Jr, Pinski JB, Robinson JK, Hanke CW. Acne, retinoids, and dermabrasion. J Dermatol Surg Oncol 1985;11:396-8.
- Bagatin E, Guadanhim LR, Yarak S, Kamamoto CS, De Almeida FA. Dermabrasion for Acne Scars during Treatment with Oral Isotretinoin. Dermatol Surg 2010;36:483-9.
Contraindications for fractional lasers
History of immunocompromised status or active systemic disease that might interfere with wound healing, any active local or systemic infection, connective tissue disorders, lactation, history of allergy to any medication necessary for treatment, active psoriasis or vitiligo, unrealistic expectations and body dismorphic disorder - all constitute relative contraindications. [1]
Reference
- Tannous Z. Fractional resurfacing. Clin Dermatol 2007;25:480-6.
Anesthesia
This is patient specific and dosage specific. Lower fluences are tolerated well by most patients; but at higher fluence levels, topical anesthesia with mixture of lidocaine and prilocaine for 60 minutes prior to the procedure may be needed. As an alternative, cold air or ice may be used to minimize discomfort. [1]
Reference
-
Fisher GH, Kim KH, Bernst;ein LJ, Geronemus RG. Concurent use of a handheld forced cold air device minimizes patient discomfort during fractional photothermolysis. Dermatol Surg 2005;31:1242-3.
Postoperative care
Minimal care is needed after the procedure. Sunscreens, avoidance of sun, moisturizers are started soon after the procedure, and diligently used daily. Mild topical steroid may be prescribed if erythema and edema persist. Postoperative antibiotics are usually not necessary. Avoidance of rubbing and scratching is advised.
Side effects or complications of fractional lasers
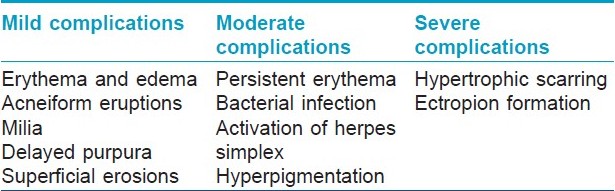
In general, the side effects of fractional lasers are minimal and transient. Mild erythema, edema and peeling are common and can be managed by use of sunscreens and moisturizers. However, side effects do occur, particularly when aggressive doses / higher stackings are used, particularly in patients with darker skin. [1] Fractional ablative lasers are more likely to produce side effects than fractional non-ablative lasers. [1] The complications observed are shown in [Table - 3].
1. Erythema
This is usually mild and stays for 2 to 3 days but can persist up to 1 week. However, more prolonged erythema and linear abrasions, often persisting up to 3-4 weeks, have been observed when fractional laser treatments with higher fluences and multiple stackings are used. [1],[2],[3]
2. Post-treatment edema
Post-treatment edema is patient-dependent. The average patient experiences edema for 1 to 3 days; though in some patients, it may last up to 1 week. The risk of edema also increases with higher fluence levels. It can be treated easily by applying ice at 10-minute intervals for the first 24 hours after treatment. Some physicians advocate the use of topical or short-course systemic corticosteroids following treatment.
3. Petechiae
Occasional petechiae can be seen, especially in periorbital area, following use of higher fluences. [4] Often such petechiae are delayed, occurring after 3 days. Avoidance of nonsteroidal anti-inflammatory drugs, aspirin and other blood thinners in the immediate postoperative period is recommended to decrease the risk of such purpura in these patients. Patients should also be advised to avoid rubbing or scratching of treated skin, because of increased skin fragility during the immediate post-treatment period.
4. Postinflammatory hypopigmentation and hyperpigmentation
Though incidence of hyperpigmentation is considerably less than that with ablative lasers, it may be seen in darker skin patients, particularly in those patients with history of post inflammatory hypopigmentation (PIH) or melasma. [5] Caution should be exercised while using higher fluences or multiple stackings in such patients. Precautionary 2 weeks of pretreatment with depigmenting agents and a strict sun protection scheme are advisable while treating such patients. Hypopigmentation is rare.
5. Bacterial infection
Bacterial infection is rare but has been reported in 0.1% of cases. [6]
6. Transient acneiform eruptions and milia may occur. [7],[8],[9] Antibiotics can be used to prevent flareups of acneiform eruptions.
7. Cicatricial ectropion is a rare but potentially serious complication and has been reported after fractional CO 2 laser treatment. [10]
8. Hypertrophic scarring, though rare, has been reported after fractional CO 2 laser use for neck rejuvenation. [11] Focal areas of erythema and induration, 2 to 4 weeks after treatment, are the first signs of potential scar formation. Neck is an area prone to such scarring. Postoperative wound infection, contact dermatitis and tendency for keloidal scarring are other potential risk factors.
References
- Metelitsa AI, Alster TS. Fractionated laser skin resurfacing treatment complications: A review. Dermatol Surg 2010;36:299-306.
- Ross RB, Spencer J. Scarring and persistent erythema after fractionated ablative CO2 laser resurfacing. J Drugs Dermatol 2008;7:1072-3.
- Rokhsar CK, Fitzpatrick RE. The treatment of melasma with fractional photothermolysis: A pilot study. Dermatol Surg 2005;31:1645-50.
- Fife DJ, Zachary CB. Delayed pinpoint purpura after fractionated carbon dioxide treatment in a patient taking ibuprofen in the postoperative period. Dermatol Surg 2009;35:553.
- Chan HH, Manstein D, Yu CS. The prevalence and risk factors of post-inflammatory hyperpigmentation after fractional resurfacing in Asians. Lasers Surg Med 2007;39:381-5.
- Setyadi HG, Jacobs AA, Markus RF. Infectious complications after nonablative fractional resurfacing treatment. Dermatol Surg 2008;34:1595-8.
- Fisher GH, Geronemus RG. Short-term side effects of fractional photothermolysis. Dermatol Surg 2005;31:1245-9.
- Graber EM, Tanzi EL, Alster TS. Side effects and complications of fractional laser photothermolysis: Experience with 961 treatments. Dermatol Surg 2008;34:301-5.
- Wanner M, Tanzi EL, Alster TS. Fractional photothermolysis: Treatment of facial and nonfacial cutaneous photodamage with a 1,550-nm erbium-doped fiber laser. Dermatol Surg 2007;33:23-8.
- Fife DJ, Fitzpatrick RE, Zachary CB. Complications of fractional CO 2 laser resurfacing: Four cases. Lasers Surg Med 2009;41:179-84.
- Avram MM, Tope WD, Yu T, Szachowicz E, Nelson JS. Hypertrophic scarring of the neck following ablative fractional carbon dioxide laser resurfacing. Lasers Surg Med 2009;41:185-8.
Task force recommendations
It is important to note that fractional laser modality has established itself as a safer modality than the previous ablative lasers. However, with its continued usage, several side effects have been reported as stated above. This becomes particularly relevant, as physicians start using higher, more aggressive fluences and increased number of stackings. Also, because of its safety profile, treatments are often performed by physician assistants/technicians. Task force recommends proper counseling and assessment of all patients, adherence to proper guidelines, and proper physician supervision of all treatments.
Summary
Fractional photothermolysis technology is an exciting new technology to treat ageing changes of skin, dyspigmentation, acne scars and striae. The technique is easy, safe to use and has been used effectively for several conditions in Indian skin. As in all esthetic treatments, proper training, judicious case selection, patient counseling about realistic expectations and proper preoperative and postoperative care are important. Further, as in all new modalities, their use has to be done with caution, keeping the possible side effects in mind.
Acknowledgment
The authors thank Drs. Anitha B and Geethika Seth for their help in preparation of tables and in editing.
Fulltext Views
17,893
PDF downloads
4,434





