Translate this page into:
Generalized eruptive histiocytosis mimicking leprosy
2 Department of Pathology, Kempegowda Institute of Medical Sciences, Bangalore, India
Correspondence Address:
B C Sharath Kumar
Department of Dermatology, KIMS Hospital, Bangalore - 560 004
India
| How to cite this article: Sharath Kumar B C, Nandini A S, Niveditha S R, Gopal M G, R. Generalized eruptive histiocytosis mimicking leprosy. Indian J Dermatol Venereol Leprol 2011;77:498-502 |
Abstract
Generalized eruptive histiocytosis (GEH) is a rare cutaneous histiocytosis that mainly affects adults and presents with multiple symmetric papules on face, trunk, and proximal extremities. GEH is included in type IIa (histiocytes involving cells of dermal dendrocyte lineage) of histiocytic disorders. Clinical and pathological correlations are required for differentiating GEH from other histiocytic disorders and from lepromatous leprosy which clinically mimic GEH and is prevalent in India. We report a case of a middle-aged woman who presented with generalized asymptomatic papules and nodules and was treated for leprosy but was finally diagnosed to have GEH after clinical, histopathological, and immunohistochemical correlation. Furthermore, the newer lesions also showed features of progressive nodular histiocytosis.Introduction
Generalized eruptive histiocytosis (GEH) is a rare cutaneous histiocytosis that mainly affects adults and presents with multiple symmetric papules on face, trunk, and proximal extremities. [1] Clinical, histopathological, and immunohistochemical studies play an important role in coming to a final diagnosis and to differentiate it from other infiltrative conditions common in this geographical location, like leprosy. We report a case of a middle-aged woman who presented with generalized asymptomatic papules and nodules and was treated for leprosy but was finally diagnosed to have GEH which had progressed to progressive nodular histiocytosis (PNH).
Case Report
A 28-year-old woman presented with generalized erythematous papules and nodules with a symmetric distribution since the preceding 5 years [Figure - 1] and [Figure - 2]. Lesions had initially started on the extremities and the face was involved later. No history of joint pains or weight loss was reported. No history of tingling or numbness of the extremities was reported. However, there was a history of spontaneous resolution of some of the lesions on the extremities but new lesions appeared in other parts of the body. The lesions on the face were persistent without any spontaneous regression. The patient was treated for leprosy in her native place based on clinical examination and had completed one year of multibacillary multidrug therapy (MB-MDT) adult regimen (three drug regimen) with no improvement except for resolution of few lesions which was happening even before the treatment. On examination, there were no signs of peripheral nerve involvement or joint involvement. At this point, a provisional differential diagnosis of histiocytoses (multicentric reticulohistiocytosis, GEH, indeterminate cell histiocytosis, PNH, xanthoma disseminatum), lepromatous leprosy (histoid), post-kala azar dermal leishmaniasis, sarcoidosis, secondary syphilis, follicular mucinosis, and cutaneous T-cell lymphoma was made and the patient investigated.
 |
| Figure 1: Clinical picture of infiltrated papules, nodules, and plaques on face. Inset: Note the prominent medial eyebrow involvement and papules coalesced to form plaques on cheek |
 |
| Figure 2: Infiltrated papules on face with prominent ear lobe nodules mimicking leprosy. Infiltrated papules and nodules seen on extremities |
Investigations done include routine hematology; erythrocyte sedimentation rate (ESR); renal and hepatic function tests which were normal; Venereal Disease Research Laboratory (VDRL) test which was nonreactive; slit skin smears (SSS) which were negative for acid fast bacilli (AFB); abdominopelvic ultrasound, chest X-ray, and lipid profile which were normal. Histopathology revealed nodular aggregates in the papillary and reticular dermis but with a grenz zone [[Figure - 3] inset]. The nodular aggregates were comprised of large histiocytes with abundant granular to foamy cytoplasm and irregular to indented nuclei which were intimately admixed with small mature lymphocytes and occasional epithelioid cells [Figure - 3] and [Figure - 4]. Section did not show any giant cells. Special stains were negative for AFB or fungi. Immunohistochemistry (IHC) studies were negative for CD 10, CD30, EMA (epithelial membrane antigen), CD43, CD20, LCA (leucocyte common antigen), CK (cytokeratin), S 100, and CD3, but CD 68 was positive [Figure - 5]. Electron microscopy showed no Birbeck granules. With all these findings, a final diagnosis of GEH progressing to PNH was made and the patient was started on phototherapy (PUVA). Even after 25 sessions of PUVA, there was not much improvement and patient did not continue further treatment and was lost for follow-up.
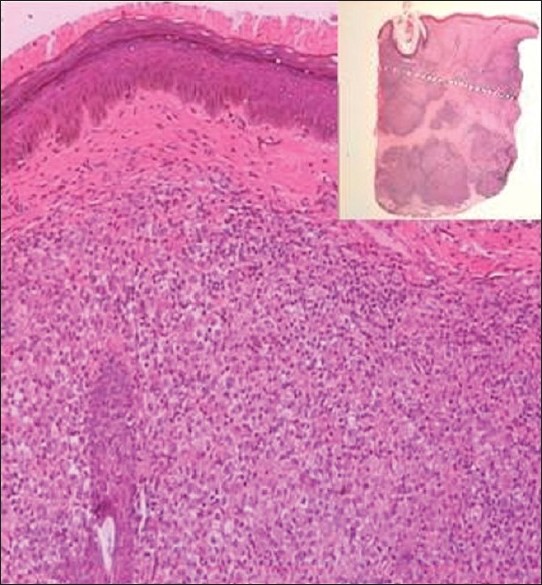 |
| Figure 3: Papillary dermis showing predominantly histiocytes admixed with few lymphocytes (H and E, ×100). Inset: whole mount of nodule showing nodular aggregates in the papillary and reticular dermis (H and E, scanner view) |
 |
| Figure 4: Nodule showing large histiocytes with abundant eosinophilic to foamy cytoplasm and vesicular nucleus admixed with lymphocytes (H and E, ×400). Inset: focal granular PAS positivity in the cytoplasm of the histiocytes (PAS, ×400) |
 |
| Figure 5: Left: focal CD 68 positivity in histiocytes (CD 68 (DAKO), ×400). Right: S 100 negativity (S 100 (DAKO), ×400) |
Discussion
Histiocytosis is classified into type I - Langerhans cell histiocytosis, type IIa - histiocytes involving cells of dermal dendrocyte lineage, type IIb - histiocytosis involving cells other than Langerhans cells and dermal dendrocytes, and type III - malignant histiocytic disorders. [1] GEH is included in Type IIa - reactive histiocytoses involving cells of dermal dendrocyte lineage. [1] GEH is a rare cutaneous histiocytosis that mainly affects adults, [1],[2],[3] although children with these disorders have been reported. [4],[5],[6] Ever since Winkelmann and Muller described cases of GEH in three patients in 1963, many cases have been reported. [7] Clinically, GEH presents with multiple asymptomatic skin colored, brownish or blue-red symmetric papules on face, trunk, and proximal extremities which tend to come in crops. Mucosal lesions are rare. [1] Spontaneous resolution of the lesions seen in GEH may be due to apoptosis. [8] GEH may rarely be associated with underlying hematological malignancies like acute monocytic leukemia. [9]
The features in this case which favored the diagnosis of GEH include age of the patient (adult), presence of multiple asymptomatic, skin colored to erythematous, symmetrical papules on face, trunk, and extremities, absence of systemic involvement and absence of mucosal lesions, history of spontaneous resolution of the lesions seen on the extremities, histopathological features of nodular aggregates of large histiocytes and absence of giant cells, and lastly the IHC studies showing histiocytes being CD 68 positive and S 100 negative, and electron microscopy showing absence of Birbeck granules.
The differential diagnosis considered for GEH included lepromatous leprosy (histoid variant); the skin colored infiltrated papules; and plaques predominantly on face involving medial aspect of eyebrows and ear lobe infiltration had led to a diagnosis of Hansen′s disease in her native place, the disease being more prevalent in a country like India. Our patient had also received a complete course of MB- MDT for 1 year (WHO guidelines for leprosy treatment) but had only some improvement at times which can be attributed to the spontaneous resolution of lesions seen in GEH. Absence of peripheral nerve involvement clinically and failure to demonstrate AFB in SSS ruled out the possibility of leprosy.
Post kala azar dermal leishmaniasis, sarcoidosis, secondary syphilis, follicular mucinosis, and cutaneous T-cell lymphoma were ruled out based on blood investigations and histopathologic examination.
Other histiocytoses considered were xanthoma disseminatum which occurs in young men, with prominent flexural involvement and mucocutaneous involvement, [1],[3] and hence was ruled out. Multicentric reticulohistiocytosis is more common in older age, has acral predominance and associated arthropathy, [1],[10] and hence did not fit into the present case. [Table - 1] summarizes the differential diagnosis of generalized non-Langerhans′ cell (non X) histiocytoses.

PNH is a rare histiocytosis first described by Taunton et al. [11] It consists of superficial papules and deep nodules with random distribution. Mucosal involvement may be present. [11],[12] Histologically, this is a dermal disease. Early lesions show an accumulation of xanthomatized and scalloped histiocytes with some infiltrating lymphocytes. In older lesions, the histiocytes are spindle-shaped and arranged in storiform pattern. [13] Occasional giant cells may be present. [13] Although patients remain in good health, with no signs of spontaneous resolution over years, new lesions may develop and may be very disfiguring. [1],[14] Association of PNH with systemic disorders has been reported. [15]
Many of the features in our case are also seen in PNH such as prominent face involvement, grouping of few lesions on the face, more of nodular lesions on face, [1],[14] and HPE showing nodular aggregates comprising of large histiocytes with abundant granular to foamy cytoplasm and irregular to indented nuclei which were intimately admixed with small mature lymphocytes and occasional epithelioid cells. No giant cells were seen. These HPE features can be seen in early lesions of PNH. Though PNH is common in children and involves mucosa, cases of adults without mucosal involvements are reported. [15] Hence, a possibility of GEH progressing onto PNH or both being variants of the same disease can be considered.
The case also reinforces the fact that some of the conditions described under histiocytoses IIa classification may not be specific disease entities but clinical variants or spectrum of a single disease, [1],[16],[17] as reported in a case of a 4-year-old boy with GEH who later developed lesions confirmed to be as xanthoma disseminatum. [4] In fact, Jang et al. [18] proposed that GEH be divided into the following two subsets: an indifferent stage of other histiocytic disorders and a specific condition without subsequent disorder. [18] Hence, a frequent follow-up of patients is to be done to look for any change in lesions or systemic involvement and if present, it necessitates a repeat biopsy from newer lesion and systemic review. [6] According to a review, PNH has been considered as the last stage of particular forms of non-langerhans cell histiocytoses such as GEH, xanthoma disseminatum, papular xanthoma, and multicentric reticulohistiocytosis. [14]
Our patient was started on phototherapy (PUVA) and took it for 25 sessions (over a period of 2 months) and stopped after that as she did not have any response. Nonresponsiveness to PUVA can be attributed to the progression of the disease to PNH. Treatments known to be effective in GEH include PUVA [19] and isotretinoin. [20] Treatments tried for PNH including intralesional [12] and systemic corticosteroids [21] and cyclophosphamide were unable to modify the progressive course of the disease. Surgical excision [11],[12] and carbon dioxide laser [15] have been tried.
Acknowledgement
The authors thank NIMHANS, Bangalore, for the immunohistochemistry and electron microscopy studies.
| 1. |
Chu AC. Histiocytosis. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 8 th ed. Oxford: Blackwell Publishing; 2010. pp. 55.1-55.33.
th ed. Oxford: Blackwell Publishing; 2010. pp. 55.1-55.33. '>[Google Scholar]
|
| 2. |
Muller SA, Wolff K, Winkelmann RK. Generalized eruptive histiocytoma: Enzyme histochemistry and electronmicroscopy. Arch Dermatol 1967;96:11-7.
[Google Scholar]
|
| 3. |
Seward JL, Malone JC, Callen JP. Generalized eruptive histiocytosis. J Am Acad Dermatol 2004;50:116-20.
[Google Scholar]
|
| 4. |
Repiso T, Miralles RM, Kanitakis J, Rodellas CA. Generalized eruptive histiocytoma evolving into xanthoma disseminatum in a 4-year-old boy. Br J Dermatol 1995;132:978-82.
[Google Scholar]
|
| 5. |
Winkelmann RK, Kossard S, Fraga S. Eruptive histiocytoma of childhood. Arch Dermatol 1980;116:565-7.
[Google Scholar]
|
| 6. |
Wee SH, Kim HS, Chang SN, Kim DK, Park WH. Generalized eruptive histiocytoma: A pediatric case. Pediatr Dermatol 2000;17:453-5.
[Google Scholar]
|
| 7. |
Winkelmann RK, Muller SA. Generalized eruptive histiocytoma: A benign papular histiocytic reticulosis. Arch Dermatol 1963;88:586-96.
[Google Scholar]
|
| 8. |
Tang X, Shen H, Xu A, Sun X, Wang Y, Shi G, et al. Spontaneous regression of generalized eruptive histiocytosis: Possible involvement of apoptosis? Int J Dermatol 2007;46:1073-5.
[Google Scholar]
|
| 9. |
Klemke CD, Dippel E, Geilen CC, Koenigsmann MP, Thiel E, Orfanos CE, et al. Atypical generalized eruptive histiocytosis associated with acute monocytic leukemia. J Am Acad Dermatol 2003;49:S233-6.
[Google Scholar]
|
| 10. |
Rao AG, Lakshmi TS, Vani V. Multicentric reticulohistiocytosis. Indian J Dermatol Venereol Leprol 2003;69:35-6.
[Google Scholar]
|
| 11. |
Taunton OD, Yeshurun D, Jarratt M. Progressive nodular histiocytoma. Arch Dermatol 1978;114:1505-8.
[Google Scholar]
|
| 12. |
Burgdorf WH, Kusch SL, Nix TE Jr, Pitha J. Progressive nodular histiocytoma. Arch Dermatol 1981;117:644-9.
[Google Scholar]
|
| 13. |
Zelger BW, Staudacher C, Orchard G, Jones WE, Burgdorf WH. Solitary and generalized variants of spindle cell xanthogranuloma (progressive nodular histiocytosis). Histopathology 1995;27:11-9.
[Google Scholar]
|
| 14. |
Caputo R, Marzano AV, Passoni E, Berti E. Unusual variants of non-langerhans cell histiocytoses. J Am Acad Dermatol 2007;57:1031-45.
[Google Scholar]
|
| 15. |
Ruíz GA, Ruíz BA, Fraile AH, Martinez PI, Muñoz GM. Progressive nodular histiocytosis accompanied by systemic disorders. Br J Dermatol 2000;143:628-31.
[Google Scholar]
|
| 16. |
Jorge FB, Buján GJ, Losada DP, Rodríguez AR, Fonseca E. A case of generalized eruptive histiocytosis. Acta Derm Venereol 2007;87:533-6.
[Google Scholar]
|
| 17. |
Sidoroff A, Zelger B, Steiner H, Smith N. Indeterminate cell histiocytosis- A clinicopathological entity with features of both X- and non-X histiocytosis. Br J Dermatol 1996;134:525-32.
[Google Scholar]
|
| 18. |
Jang KA, Lee HJ, Choi JH, Sung KJ, Koh JK, Moon KC. Generalized eruptive histiocytoma of childhood. Br J Dermatol 1999;140:174-6.
[Google Scholar]
|
| 19. |
Ma LH, Metze D, Luger TA, Steinhoff M. Successful treatment of generalized eruptive histiocytoma with PUVA. J Dtsch Dermatol Ges 2007;5:131-4.
[Google Scholar]
|
| 20. |
Kwinter J, Koven DJ. Generalized eruptive histiocytoma treated with isotretinoin. J Cutan Med Surg 2009;13:146-50.
[Google Scholar]
|
| 21. |
Torres L, Sánchez JL, Rivera A, González A. Progressive nodular histiocytosis. J Am Acad Dermatol 1993;29:278-80.
[Google Scholar]
|
Fulltext Views
4,798
PDF downloads
2,911





