Translate this page into:
Giant condyloma acuminatum of Buschke and Löwenstein of the vulva: Successful treatment with diphenylcyclopropenone contact sensitization
2 Department of Dermatology, Chang Gung Memorial Hospital, Taoyuan; Drug Hypersensitivity Clinical and Research Center, Immune-Oncology Center of Excellence, Chang Gung Memorial Hospital, Linkou, Taipei; College of Medicine, Chang Gung University, Taoyuan, Taiwan
Correspondence Address:
Jennifer Wu
Department of Dermatology, Chang Gung Memorial Hospital, No. 5, Fuxing St., Guishan Dist., Taoyuan 33305
Taiwan
| How to cite this article: Yen CF, Yang CH, Wu J. Giant condyloma acuminatum of Buschke and Löwenstein of the vulva: Successful treatment with diphenylcyclopropenone contact sensitization. Indian J Dermatol Venereol Leprol 2020;86:592-594 |
Sir,
Giant condyloma acuminatum of Buschke and Löwenstein is a large exophytic, slow-growing benign verrucous lesion of the anogenital region, caused by human papillomavirus. The pathogenesis of giant condyloma acuminatum is not well understood and is often considered an intermediate between condyloma acuminatum and low virulence squamous cell carcinoma.[1] Though it seldom metastasizes, giant condyloma acuminatum is locally destructive and shows an unpredictable response to a variety of therapies in clinical practice. Thus, the management of giant condyloma acuminatum remains challenging given the poor treatment response and high recurrence rates. We herein report a case of giant condyloma acuminatum of Buschke and Löwenstein treated successfully with topical 0.1% diphenylcyclopropenone immunotherapy.
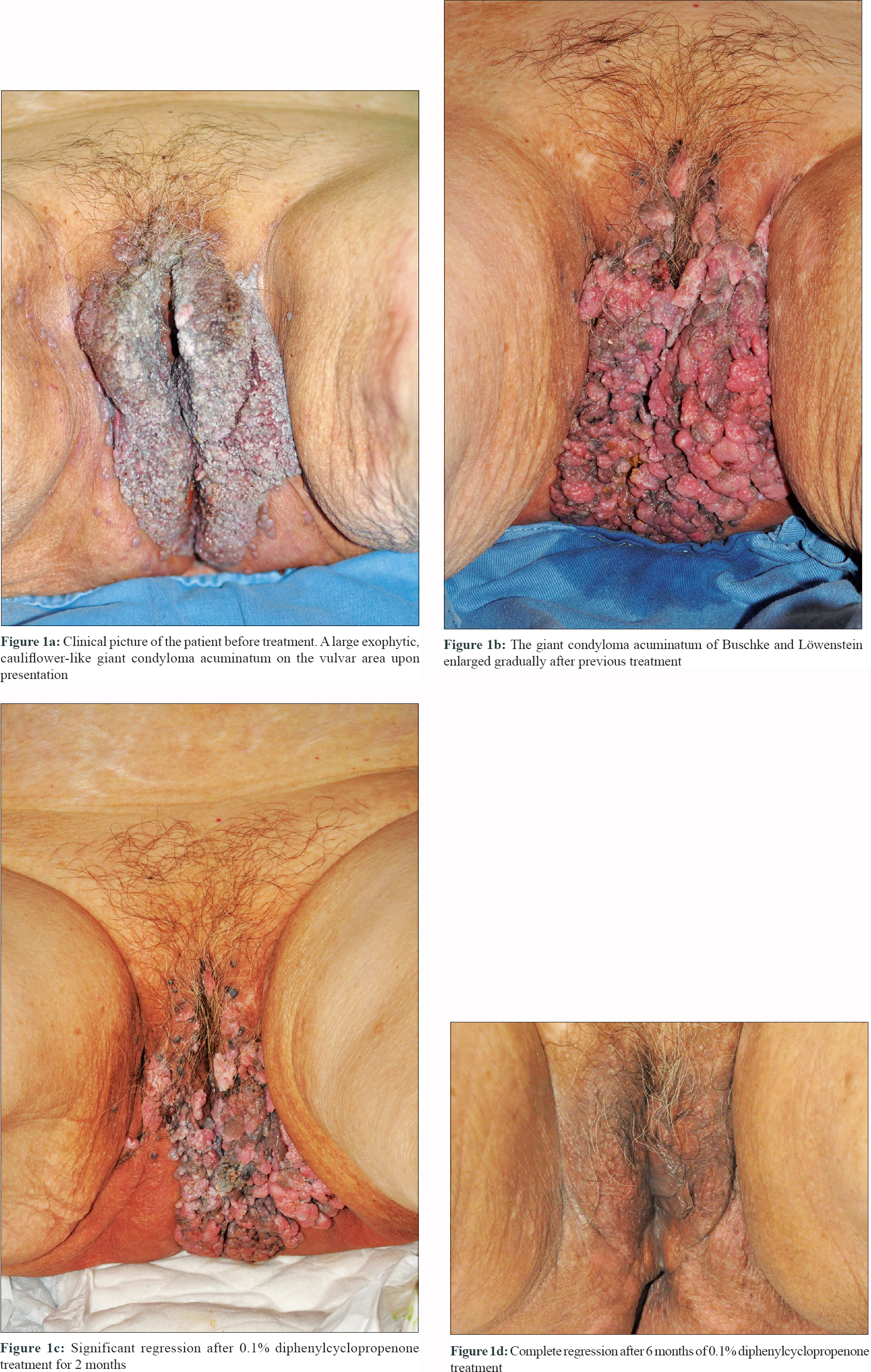
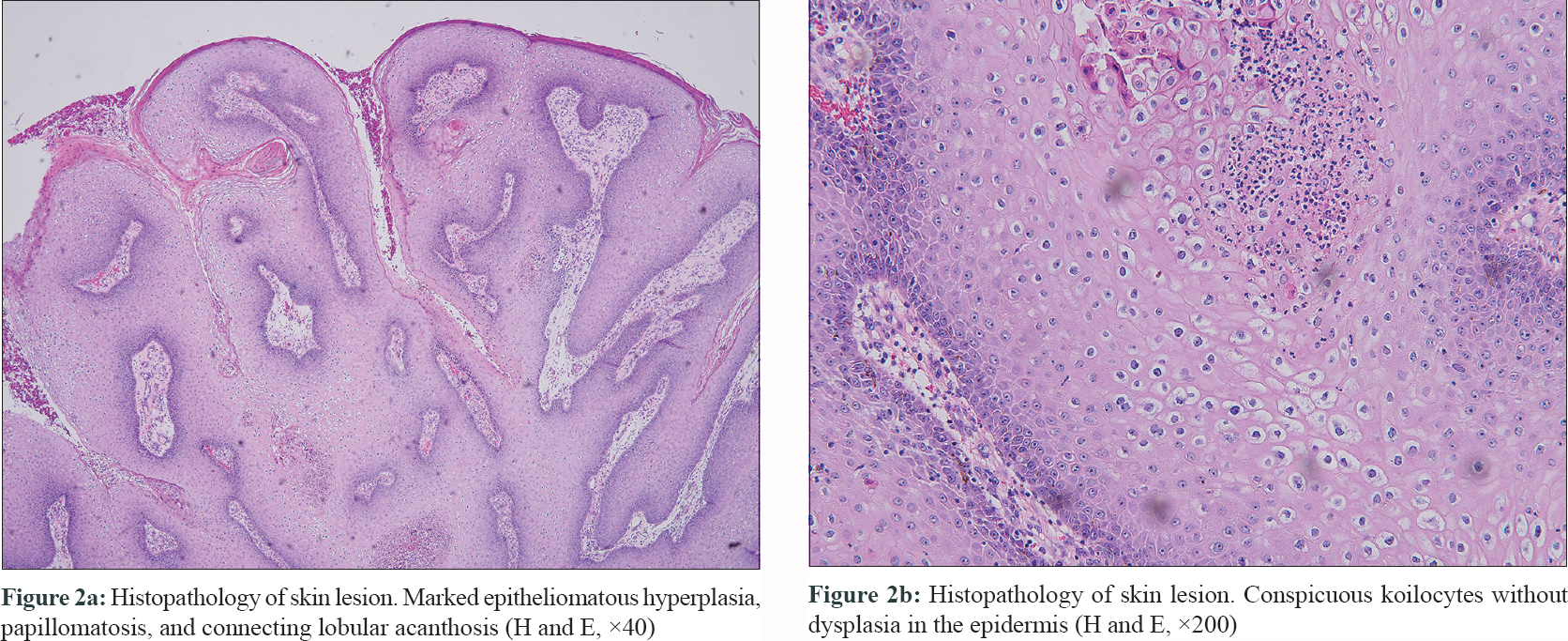
This 88-year-old woman presented with a large multi-lobulated, painless and foul-smelling lesion on the vulvar region since the past 15 years. The patient had no sexual activity for almost three decades. Physical examination showed a 10 × 15 cm flesh-colored, cauliflower-like, verrucous lesion extending from vulva to the anus [Figure - 1]a. There was no associated regional lymphadenopathy and systemic examination was essentially normal. Tests for human immunodeficiency virus (HIV Ag/Ab combination test) and syphilis (Venereal Disease Research Laboratory test) were negative. For treatment, topical podophyllotoxin cream 0.15% applied twice daily for 3 consecutive days per week for 1 month, imiquimod cream 5% three times per week combined with cryotherapy once every 2 weeks for 3 months and oral levamisole 40 mg once daily combined with cimetidine 200 mg twice daily for 2 months were used sequentially. However, the lesion progressed gradually despite these treatment modalities used over a period of 6 months [Figure - 1]b. A biopsy from the lesion showed marked epitheliomatous hyperplasia with connecting lobular acanthosis, plenty of koilocytes and no dysplasia [Figure - 2]a and [Figure - 2]b. The clinical and histopathology features were consistent with giant condyloma acuminatum. The computed tomography of the abdomen and pelvis showed no lymphadenopathy or organ involvement.
 |
 |
As the response to previous treatment was poor and her family members did not consent for surgical excision, local immunotherapy with diphenylcyclopropenone was opted for. To sensitize the patient, 1% diphenylcyclopropenone was applied to the left upper arm within a circle of 2-cm diameter and left for 24 h. One week after sensitisation, the immunotherapy was started by applying 0.1% diphenylcyclopropenone solution locally on the giant condyloma acuminatum of Buschke and Löwenstein once every two weeks for 2 months and the patient was followed up regularly [Figure - 1]c. The treatment was well tolerated except for a self-limiting mild perilesional erythema and pruritus. The lesion disappeared completely after 6 months of treatment with some post-inflammatory hypopigmentation, but without scarring [Figure - 1]d. No relapse was noted during the post-treatment follow-up period of 2 years.
Literature reveals that local ablation by carbon dioxide laser, cryotherapy, podophyllin, imiquimod, or intralesional chemotherapy is considered less efficacious in eradicating giant condyloma acuminatum.[2] The efficacy of immunotherapy with diphenylcyclopropenone has been observed previously to treat common warts and anogenital warts.[3],[4],[5] It was also found to be effective and safe for the treatment of giant condyloma acuminatum of Buschke and Löwenstein in our patient without any recurrence during the 2-year follow-up. Side effects were only limited to the treatment site as local erythema and burning sensation immediately after application that resolved after treatment discontinuation.
The precise mechanism by which diphenylcyclopropenone immunotherapy cleared giant condyloma acuminatum of Buschke and Löwenstein in our case remains speculative. Topical diphenylcyclopropenone is a contact sensitizer mainly used for immunotherapy in alopecia areata and sometimes to treat viral warts.[3] It is said to form a hapten with viral/wart proteins that are recognized by T cells leading to the destruction of human papillomavirus-infected cells via type-IV hypersensitivity immune reaction and/or by activating the function of natural killer cells.[3],[4],[5] However, despite being a significantly destructive procedure with a high rate of recurrence, a wide surgical excision with or without systemic chemotherapy with methotrexate or bleomycin will be needed for extensive or recurrent giant condyloma acuminatum, especially for lesions with histological dysplasia.[2]
Though it is not possible to make any recommendations, immunotherapy with diphenylcyclopropenone appears to be a safe and promising treatment alternative for giant condyloma acuminatum of Buschke and Löwenstein from our experience with this case. It has the added advantage of preserving tissue function and the results are cosmetically elegant when compared with surgical procedures involving the vulva.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal the identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Martin JM, Molina I, Monteagudo C, Marti N, Lopez V, Jorda E. Buschke-Lowenstein tumor. J Dermatol Case Rep 2008;2:60-2.
[Google Scholar]
|
| 2. |
Anissa Z, Houda HG, Wafa K, Olfa M, Rym BM, Achraf D, et al. Successful treatment with topical imiquimod of anal Buschke-Löwenstein tumor in a child. Dermatol Ther 2015;28:363-5.
[Google Scholar]
|
| 3. |
Miyata K, Go U, Fujita M, Mitsuishi T. Successful treatment with topical diphenylcyclopropenone for three cases of anogenital warts in children. Case Rep Dermatol 2019;11:123-9.
[Google Scholar]
|
| 4. |
Buckley DA, Du Vivier AW. The therapeutic use of topical contact sensitizers in benign dermatoses. Br J Dermatol 2001;145:385-405.
[Google Scholar]
|
| 5. |
Suh DW, Lew BL, Sim WY. Investigations of the efficacy of diphenylcyclopropenone immunotherapy for the treatment of warts. Int J Dermatol 2014;53:e567-71.
[Google Scholar]
|
Fulltext Views
3,901
PDF downloads
1,722





