Translate this page into:
Giant warts in a Chinese with epidermodysplasia verruciformis
Correspondence Address:
Hong Fang
No. 79 Qingchun Road, Department of Dermatology, The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou 310003
China
| How to cite this article: Zhu D, Fang H, Qiao J, Liu X, Xu B, Si Z. Giant warts in a Chinese with epidermodysplasia verruciformis. Indian J Dermatol Venereol Leprol 2011;77:730 |
Sir,
Epidermodysplasia verruciformis (EV) is a rare genodermatosis with an increased susceptibility to specific human papillomavirus (HPV) genotypes. EV may be inherited or acquired. The inherited form has a genetically determined defect in cutaneous immunity, resulting in susceptibility to persistent HPV infection. The acquired form has been reported in leukemia patients, transplant recipients, and HIV positive patients. The development of genital warts in patients with EV is rare, with only 3 cases reported throughout the world literature, with none in Asia. [1],[2],[3] We describe here the unusual case of a Chinese EV patient with concomitant giant genital and axillary warts.
A 30-year-old Chinese man presented to our hospital with a 10-year history of numerous papules and macules on his face, upper trunk, and limbs, all of which were asymptomatic. Six months before consultation he noticed multiple itching masses on his scrotum and axilla. Over time, the masses progressively increased in number and size. There was no family history of similar lesions and no history of consanguinity. Physical examination revealed extensive pityriasis, versicolor-like macules on the upper trunk and neck, and several discrete 2-3 mm brown slightly raised plaques similar to seborrheic keratosis on the face and neck. We also observed numerous papule-like flat warts and common warts on his extremities, a 15 cm×12 cm cauliflower-shaped exophytic mass covering his entire scrotal region and portions of his penis, and several similar moist masses on his right axilla [Figure - 1]. Systemic examination showed no abnormalities. Routine laboratory tests including hematological and biochemical analyses of blood and urine were within normal ranges, and he was negative serologically for HIV and syphilis. We observed a slightly lower CD4+ T cell count (20.7% [normal 27-51%]), a higher CD8+ cell count (57.8% [normal 15-44%]), and a reversal of the CD4+/CD8+ ratio (0.35 [normal 0.9-3.2]). A skin biopsy taken from the axilla revealed parakeratosis, papillomatosis, and large vacuolated cells in the spinous layer, all of which were highly indicative of underlying HPV infection [Figure - 2]. Histological examination of a papule on his right forearm showed acanthosis with hyperkeratosis and parakeratosis, an irregular and thickened granular layer and very small nuclei, indicating a diagnosis of EV [Figure - 3]. PCR amplification of genomic DNA extracted from the axillary and genital warts revealed an infection with HPV type 11. Based on the above findings, he was diagnosed with EV with giant axillary and genital warts. The axillary and genital masses were surgically excised, resulting in their complete disappearance [Figure - 4]. He was treated with oral acitretin 20 mg/day for 2 months, but the EV lesions did not show any clinical changes.
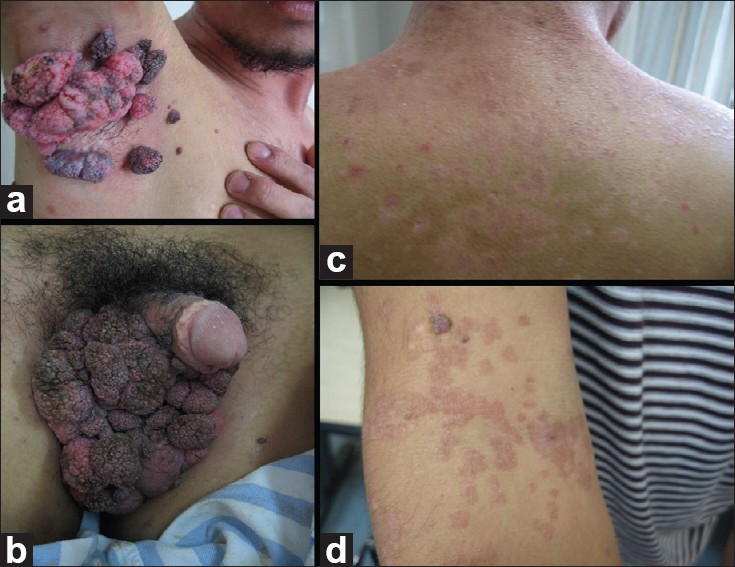 |
| Figure 1: Photographs of this patient, showing multiple cauliflower-shaped exophytic masses on (a) the right axilla and (b) scrotum, (c) pytiriasis versicolor-like lesions on his back, (d) and papule-like flat warts and common warts on his right forearm |
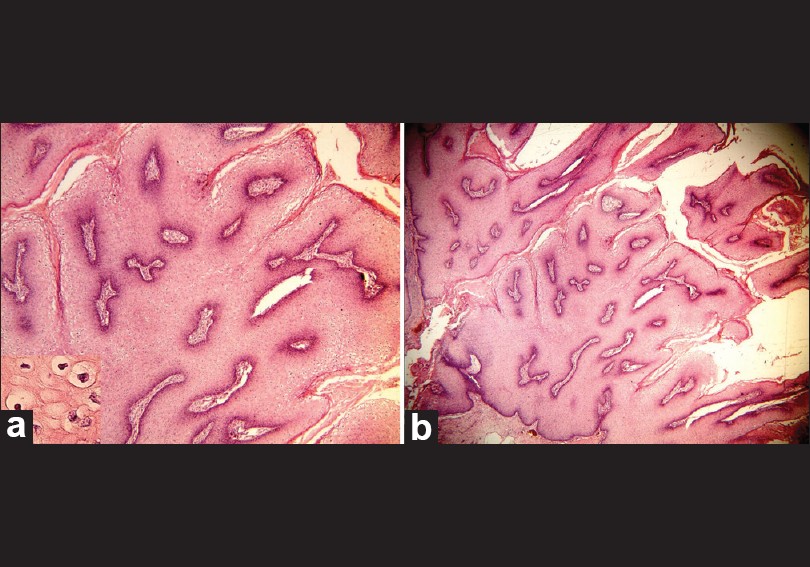 |
| Figure 2: (a, b) Histopathology of his axillar warts, showing parakeratosis and papillomatosis involving the entire epithelial layer (H and E, ×20) |
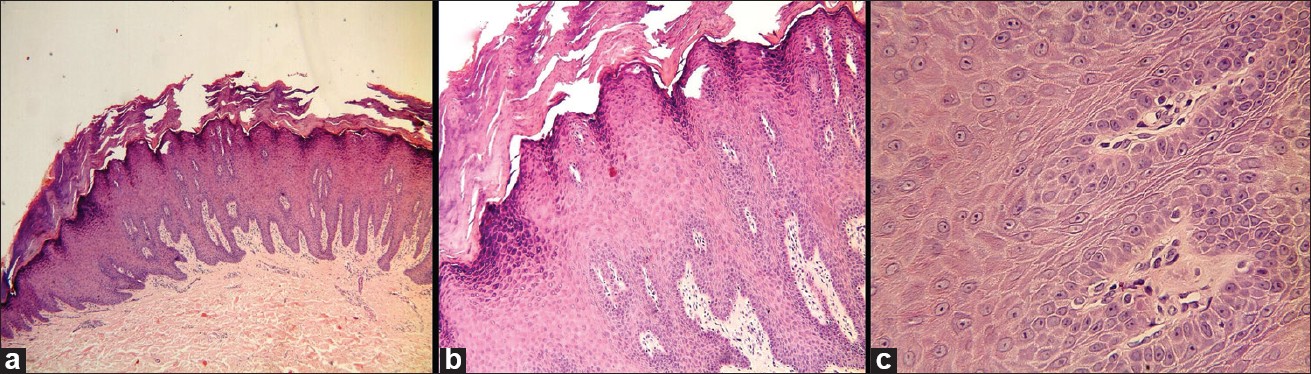 |
| Figure 3: Histopathology of a papule on the right forearm of our patient, showing acanthosis with hyperkeratosis, parakeratosis and thickened granular layers (a. H and E, ×40; b. H and E, ×100; c. H and E, ×400) |
 |
| Figure 4: (a,b) Photographs showing disappearance of the warts after surgical excision |
Epidermodysplasia verruciformis, first described in 1922, is a rare genetic disorder characterized by highly polymorphic cutaneous lesions that can undergo malignant transformation, and an extreme susceptibility to certain human papillomaviruses including HPV types 5, 8, 9, 12, 14, 15, 17, 19, 25, 36, 38, 47, and 50, collectively termed EV-HPV. [4] EV is characterized by a wide spectrum of histological changes. [5],[6] The lesions may resemble verruca plana, tinea versicolr, or seborrheic keratosis rather than being cauliflower-shaped exophytic masses. HPV type 11, which has not been related to EV-HPV, was detected in the axilla and genital samples from our patient. The size, extent, and local aggressiveness of the masses also make them highly unusual compared with traditional warts. The finding of HPV 11 indicates that the lesions of our patient′s genitalia and axillae may not be directly associated with EV. Genital warts developing in EV are very unusual; they may have a malignant transformation in some cases. [1] To our knowledge, this was the first reported case of EV plus concomitant genital HPV 11 infection in Asia. Another prominent finding in our patient was the presence of multiple similar masses on the right axilla, with HPV type 11 detected in these samples, as well as in genital samples. The clinical findings were novel and different from other reports. [1],[2],[3]
Epidermodysplasia verruciformis may be inherited or acquired. The inherited form usually presents in infancy or early childhood, whereas the acquired type may be secondary in immunocompromised individuals, including those with T-cell lymphoma and HIV. In our patient the lesions developed at age 20 years, so it is likely the acquired type. [7] Various abnormalities of nonspecific cell-mediated immunity can be found in most patients with EV, and no correlation has been observed between these abnormalities and the severity of EV. The abnormal condition includes a reversal of the CD4+/CD8+ ratio, a finding observed in our patient. [8] The abnormalities in cell-mediated immunity in our patient may be associated with HPV 11 infection.Treatment of EV is difficult. The genital and axillary warts in our patient were removed surgically, but treatment of the EV lesions with oral acitretin did not result in complete remission. Due to the high incidence of malignant transformation of skin lesions in EV patients, this patient was encouraged to use daily sunscreen and to have regular dermatologic follow-ups.
| 1. |
Kivanc-Altunay I, Erdogan HK, Kayaoglu S. Perianal warts and the development of squamous cell carcinoma in epidermodysplasia verruciformis. Indian J Dermatol Venereol Leprol 2011;77:112.
[Google Scholar]
|
| 2. |
Sanclemente G, García JJ, Gómez LF, Tyring SK, Wolff JC, Correa LA, et al. An unusual presentation of human papillomavirus (HPV) infection in a black epidermodysplasia verruciformis (EV) patient. Int J Dermatol 2007;46:199-201.
[Google Scholar]
|
| 3. |
Rogers HD, Macgregor JL, Nord KM, Tyring S, Rady P, Engler DE, et al. Acquired epidermodysplasia verruciformis. J Am Acad Dermatol 2009;60:315-20.
[Google Scholar]
|
| 4. |
Gewirtzman A, Bartlett B, Tyring S. Epidermodysplasia verruciformis and human papilloma virus. Curr Opin Infect Dis 2008;21:141-6.
[Google Scholar]
|
| 5. |
Nuovo GJ, Ishag M. The histologic spectrum of epidermodysplasia verruciformis. Am J Surg Pathol 2000;24:1400-6.
[Google Scholar]
|
| 6. |
Morrison C, Eliezri Y, Magro C, Nuovo GJ. The histologic spectrum of epidermodysplasia verruciformis in transplant and AIDS patients. J Cutan Pathol 2002;29:480-9.
[Google Scholar]
|
| 7. |
Cutlan JE, Rashid RM, Torres-Cabala C, Tyring SK, Thomas V. Epidermodysplasia verruciformis after cutaneous T-cell lymphoma: Periungual presentation. Dermatol Online J 2010;16:12.
[Google Scholar]
|
| 8. |
Boran P, Tokuc G, Ozberk M, Buyukbabani N, Dogan O. Epidermodysplasia verruciformis associated with natural killer/T cell lymphoma. J Pediatr 2010;156:340.
[Google Scholar]
|
Fulltext Views
29,429
PDF downloads
3,748





