Translate this page into:
Gigantic cutaneous rhinosporidiosis with giant cells bloated with sporangia
Correspondence Address:
Ashok K Ghorpade
BK D-18, Sector 9, Bhilai, Chhattisgarh - 490 006
India
| How to cite this article: Ghorpade AK. Gigantic cutaneous rhinosporidiosis with giant cells bloated with sporangia. Indian J Dermatol Venereol Leprol 2011;77:517-519 |
Sir,
A 21-year-old Indian male presented with multiple, asymptomatic skin lesions on his left leg and foot of 18 months duration. He was operated upon for a nasal growth causing bleeding and some globoid skin lesions on his left calf by a private doctor about 3 months earlier without histopathological examination. There was history of bathing in the common village pond along with buffaloes, since early childhood. There was no family history of skin or nasal lesions. Cutaneous examination showed skin colored, firm globoid skin lesion about 5 × 5 × 5 cm 3 in size on the dorsal aspect of the left foot and left leg, the former with a papular lesion about 3 mm in diameter near its base [Figure - 1]a and similar smaller ones on posterior aspect of the left leg with scars of excised lesions and varicose veins [Figure - 1]b. There were no nasal lesions, organomegaly, or lymphadenopathy at the time of examination. Systemic examination was normal. Routine hematology, blood glucose, liver and kidney function tests, abdominal ultrasound, and X-ray of the limbs were normal and ELISA for HIV 1 and 2 was negative. Histopathology from the globoid skin lesion showed foreign body giant cells bloated with engulfed sporangia and multiple sporangia with endospores in the dermis with a chronic inflammatory infiltrate [Figure - 2]a and b. Crushed tissue smear of the papular lesion also revealed similar sporangia with endospores. The smaller skin lesions were excised followed by electrocoagulation of the base, and he was given tablet dapsone 100 mg once daily without any recurrence during the follow-up of 4 months. He was advised excision for the bigger lesions.
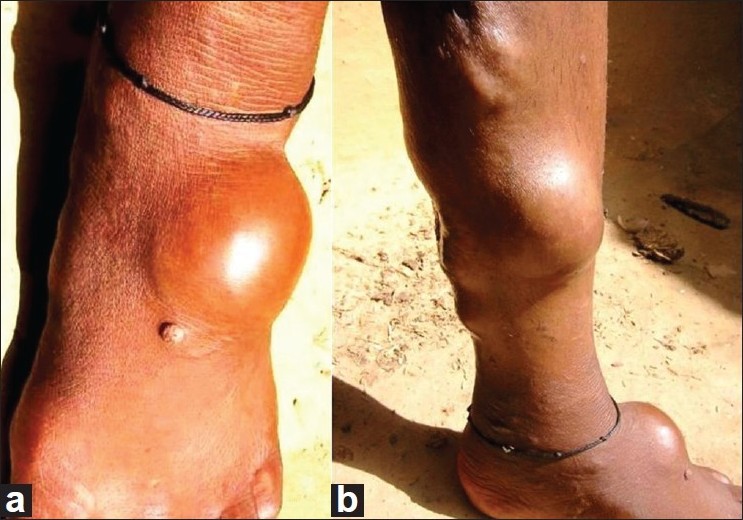 |
| Figure 1: (a) Co-existing big globoid lesion and a papule on the left foot. (b) Multiple, huge, and small globoid skin lesions on the left leg with scars of excised lesions and varicose veins |
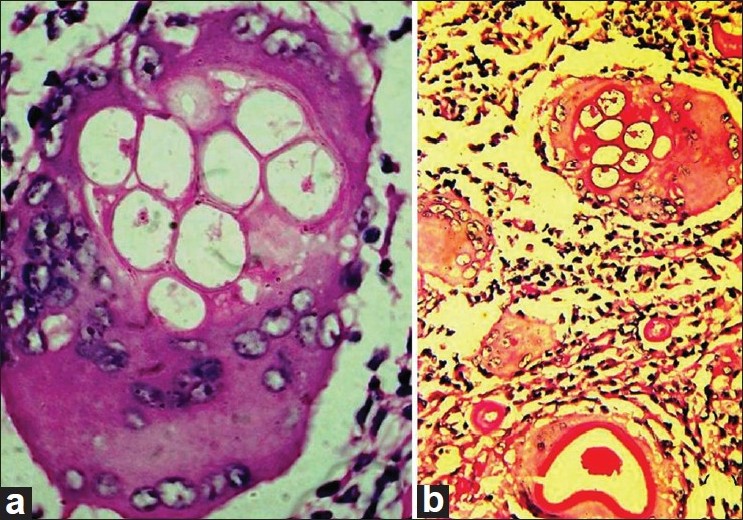 |
| Figure 2: (a) Close-up of a foreign body giant cell seen bloated with sporocysts in the upper half, and the nuclei pushed to edges (hematoxylin and eosin; original magnification, ×1000). (b) Same foreign body giant cell (as in (a)) in the upper part, with another one on the lower end. Thick-walled sporocysts with pinkish nutritional material in the lower and upper edges, two foreign body giant cells in the middle and a dense chronic inflammatory infiltrate (Periodic acid Schiff stain; original magnification, ×400) |
Rhinosporidiosis is endemic in Sri Lanka and parts of India but has been reported from other parts namely Africa, South America, and the United States. In India, Chhattisgarh, Tamil Nadu, Kerala, Karnataka, Pondicherry, and Orissa are endemic for the disease. Several cases of nasal and cutaneous rhinosporidiosis have been described from the Chhattisgarh state. [1],[2],[3],[4] In addition, sporadic cases have been described among migrant population, from other parts as well. Most of the patients are young/middle-aged males, and sharing pond bathing with cattle and repeated trauma seem to be the predisposing factors here. [1],[2],[3],[4] Rhinosporidiosis is caused by Rhinosporidium seeberi, an aquatic protistan parasite of the Mesomycetozoea class along with organisms causing similar infections in amphibians and fish. It is the first known human pathogen from the DRIPs clade. [5] There are no reports of successful in vitro culture and propagation in subculture with various types of culture media. The disease may also affect farm, domestic, and wild animals. It is commoner in males between the second to fourth decades probably due to the increased chances of exposure. The exact mode of transmission is unclear, but it might be acquired through contaminated dust, water, infected clothing, or fingers. There is mucosal involvement of nose, nasopharynx, and soft palate in the form of sessile or pedunculated vascular polyps, studded with minute whitish dots (sporangia containing the spores). Nasal obstruction and bleeding are common. Occasionally, it involves the lips, palate, uvula, maxillary antrum, epiglottis, larynx, trachea, bronchus, ear, scalp, vulva, vagina, penis, rectum, and the skin. Cutaneous rhinosporidiosis may occur from the nasal growths as satellite lesions, or as disseminated lesions with or without nasal involvement, or as primary skin lesions. They begin as papules or nodules and may spread by scratching, inoculating the organism with contaminated fingers from nasal picking, through blood or the lymphatics. [3],[4] They may resemble verruca vulgaris, tuberculosis verrucosa cutis, granuloma pyogenicum, venereal warts, or donovanosis. Cutaneous lesions at sites distant from the nasal mucosa are uncommon.
A clinical diagnosis of gigantic cutaneous rhinosporidiosis with co-existing globoid and papular skin lesions was made. Lipomas, liposarcomas, and subcutaneous aspergillosis were considered in the differential diagnosis, but the history of a nasal growth and bleeding, shared pond bathing with buffaloes, the firm globoid lesions associated with the papular skin lesions, the earlier experience of dealing with such cases suggested and histopathology confirmed the diagnosis. Coccidio idomycosis has a different clinical presentation and a smaller sporangia size. Disseminated polymorphic cutaneous rhinosporidiosis, with verrucoid, furunculoid, and a pseudohorn-like skin lesion was reported by Kumari et al. [6] Nayak et al. [7] described similar but disseminated subcutaneous globoid lesions along with sessile and pedunculated moist, shiny grouped and discrete, highly vascular swellings all over the body and scalp. Although such giant cells bloated with sporangia have been reported once in a patient having a single subcutaneous lesion and nasal rhinosporidiosis, [3] they have not been observed in a patient with polymorphic cutaneous lesions.
Treatment is by excision with electrocoagulation, but recurrences may occur. Oral dapsone might arrest the maturation of the sporangia and cause stromal fibrosis. [8]
| 1. |
Sudarshan V, Goel NK, Gahine R, Krishnani C. Rhinosporidiosis in Raipur, Chhattisgarh: A report of 462 cases. Indian J Pathol Microbiol 2007;50:718-21.
[Google Scholar]
|
| 2. |
Ramanan C, Ghorpade A. Giant cutaneous rhinosporidiosis. Int J Dermatol 1996;35:441-2.
[Google Scholar]
|
| 3. |
Ghorpade A. Rhinosporidiosis: Gigantic cells with engulfed sporangia of Rhinospoirdia seeberi in a case of dermosporidiosis. Int J Dermatol 2008;47:694-5.
[Google Scholar]
|
| 4. |
Acharya PV, Gupta RL, Darbari BS. Cutaneous rhinosporidiosis. Indian J Dermatol Venereol Leprol 1973;39:22-5.
[Google Scholar]
|
| 5. |
Fredricks DN, Jolley JA, Lepp PW, Kosek JC, Relman DA. Rhinosporidium seeberi: A human pathogen from a novel group of aquatic protistan parasites. Emerg Infect Dis 2000;6:273-82.
[Google Scholar]
|
| 6. |
Kumari R, Nath AK, Rajalakshmi R, Adityan B, Thappa DM. Disseminated cutaneous rhinosporidiosis: Varied morphological appearances on the skin. Indian J Dermatol Venereol Leprol 2009;75:68-71.
[Google Scholar]
|
| 7. |
Nayak S, Acharjya B, Devi B, Sahoo A, Singh N. Disseminated cutaneous rhinosporidiosis. Indian J Dermatol Venereol Leprol 2007;73:185-7.
[Google Scholar]
|
| 8. |
Thappa DM, Venkatesan S, Sirka CS, Jaisankar TJ, Gopalkrishnan, Ratnakar C. Disseminated cutaneous rhinosporidiosis. J Dermatol 1998;25:527-32.
[Google Scholar]
|
Fulltext Views
1,727
PDF downloads
1,697





