Translate this page into:
Gottron - like papules induced by hydroxyurea
Correspondence Address:
Prachi G Agrawal
Department of Skin and V.D., Opd No. 117, GSMC and KEM Hospital, Parel, Mumbai, Maharashtra
India
| How to cite this article: Agrawal PG, Mahajan SA, Khopkar US, Kharkar VD. Gottron - like papules induced by hydroxyurea. Indian J Dermatol Venereol Leprol 2012;78:775 |
Sir,
A 45 year old woman presented to us with an eruption on the dorsa of the hands of 2 years′ duration. She had been treated for the past 5 years with oral hydroxyurea (HU) 1.5-2 g/day for chronic myelogenous leukemia. Examination revealed presence of shiny eythematous papules and plaques with mild scaling, on the dorsa of the metacarpophalangeal and proximal interphalangeal joints of bilateral hands [Figure - 1]. She had no other eruptions in photodistributed areas, heliotrope rash, or any evidence of muscle weakness. Laboratory evaluation revealed normal serum chemistries including creatine phosphokinase, negative antinuclear antibody, and rheumatoid factor. Histopathological examination of a skin biopsy taken from one of the erythematous papules revealed the presence of slight epidermal atrophy with orthohyperkeratosis, vacuolar changes in the basal cell layer with colloid bodies, melanophages and a slight perivascular lymphomononuclear infiltrate in the upper dermis [Figure - 2]. Alcian blue stain revealed mucin deposition in the upper dermis [Figure - 3]. Based on clinico-pathologic correlation, a final diagnosis of HU induced dermatomyositis (DM) -like eruption was made. Partial improvement was observed with diligent photoprotection and mild topical corticosteroids. HU was continued considering its importance in CML treatment and mild cutaneous manifestations.
 |
| Figure 1: Shiny erythematous papules and plaques on the dorsa of bilateral hands |
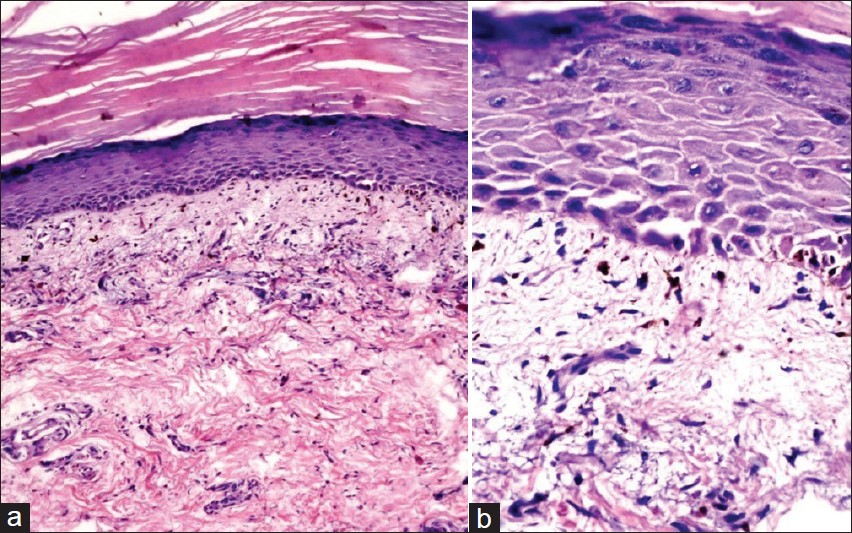 |
| Figure 2: Photomicrograph showing epidermal atrophy, orthohyperkeratosis, vacuolar changes in basal cell layer with colloid bodies, melanophages and slight perivascular lymphomononuclear infiltrate in upper dermis (H and E, ×100 (a) and ×400 (b)) |
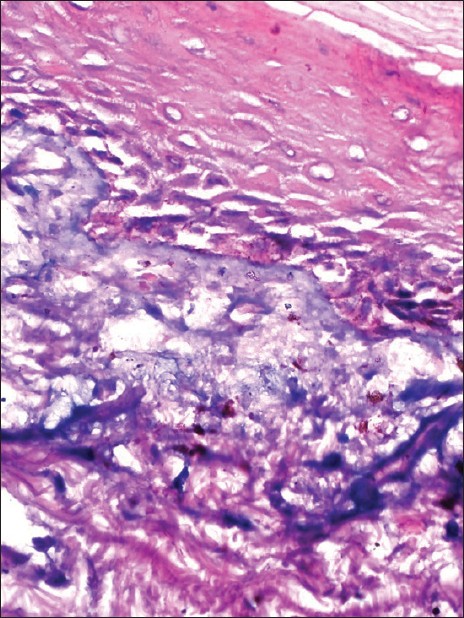 |
| Figure 3: Photomicrograph showing mucin deposition in the upper dermis (Alcian blue, × 400) |
HU is a cytotoxic chemotherapeutic agent mainly used for treatment of myeloproliferative disorders. [1] Cutaneous adverse reactions have been reported in up to 10% to 35% of patients. [2] They include facial erythema, hyperpigmentation, ichthyosis, alopecia, stomatitis, atrophy, acral erythema, palmoplantar keratoderma, leukocytoclastic vasculitis, melanonychia, and leg ulcers. More rarely, a DM-like eruption, aggressive HU-associated nonmelanoma skin cancers, or the recently described HU-associated squamous dysplasia may develop. [3]
In 1975, Kennedy et al. first reported a patient with CML who developed palmoplantar erythema and linear atrophic lesions on the dorsa of the hands, after taking HU for 3 years. [4] In 1995, Senet et al. described a DM-like eruption developing on the dorsa of the hands in six patients on long-term HU therapy. [2] This cutaneous presentation caused by HU has since been reported under different names, such as DM-like lesions, hydroxyurea dermopathy and pseudo-DM. [1] According to Vassallo et al. DM-like change was seen in 7 out of these 21 CML patients receiving HU for 7-120 months. [5]
Although the mechanism of this eruption is unknown, factors such as the latency of onset, slow progression, and subsequent healing after withdrawal of the culprit drug suggest it to be chronic cumulative cytologic damage to the basal layer and epidermis due to inhibition of DNA synthesis and repair. [1]
The reaction has typical cutaneous features of DM (scaly erythema on the dorsa of the hands with atrophic and telangiectatic changes), but without any systemic symptoms. No proximal muscle weakness has been reported and the muscle enzyme level and electromyography are normal. [2] Laboratory evaluation typically reveals negative antinuclear antibody and normal aldolase or creatine kinase. [1] The severity of the rash does not correlate with the evolution of the hematologic malignancy, if present. [2] Histologic analysis, which reveals interface dermatitis with minimal inflammation, vacuolar alteration of the basal keratinocytes with dyskeratotic keratinocytes, incontinence of melanin pigment, and rarely the presence of mucin, does not aid in differentiating DM- like eruption from true DM, for which clinical correlation is required. [1] Symptoms are generally mild, and systemic therapy has never been required to control this entity. [2] DM-like eruption has been reported to resolve within 10 days to 18 months after discontinuation of HU therapy but frequently recurs on rechallenge; however, atrophy if present, tends to persist. [1] Till date, DM-like eruption has been described as benign and does not warrant discontinuation of HU therapy. [3]
Recently it was found that DM-like eruption and HU-associated squamous dysplasia represent similar clinical manifestations of a common underlying chronic phototoxic process involving aberrant keratinocyte p53 expression mediated by HU′s antimetabolite properties and UV radiation exposure. Accordingly, it was suggested that DM-like eruption, previously considered a benign entity, may represent a premalignant precursor of HU associated nonmelanoma skin cancers warranting discontinuation of HU therapy. [3]
In summary, the DM-like eruption is a specific cutaneous adverse effect of HU therapy. To the best of our knowledge, no similar case has been reported in an Indian patient till date. As HU continues to have a prominent role in the treatment of various diseases, clinicians should be aware of this adverse drug reaction to avoid unnecessary investigations, morbidity and therapy.
| 1. |
Dacey MJ, Callen JP. Hydroxyurea-induced dermatomyositis-like eruption. J Am Acad Dermatol 2003;48:439-41.
[Google Scholar]
|
| 2. |
Senet P, Aractingi S, Porneuf M, Perrin P, Duterque M. Hydroxyurea induced dermatomyositis like eruption. Br J Dermatol 1995;133:455-9.
[Google Scholar]
|
| 3. |
Kalajian AH, Cely SJ, Malone JC, Burruss JB, Callen JP. Hydroxyurea-associated dermatomyositis-like eruption demonstrating abnormal epidermal p53 expression: A potential premalignant manifestation of chronic hydroxyurea and UV radiation exposure. Arch Dermatol 2010;146:305-10.
[Google Scholar]
|
| 4. |
Kennedy BJ, Smith LR, Goltz RW. Skin changes secondary to hydroxyurea therapy. Arch Dermatol 1975;111:183-7.
[Google Scholar]
|
| 5. |
Vassallo C, Passamonti F, Merante S, Ardigò M, Nolli G, Mangiacavalli S, et al. Mucocutaneous changes during long-term therapy with hydroxyurea in chronic myeloid leukaemia. Clin Exp Dermatol 2001;26:141-8.
[Google Scholar]
|
Fulltext Views
3,145
PDF downloads
2,993





