Translate this page into:
Graft versus host disease localized to striae distensae: An example of locus minoris resistentiae
Corresponding author: Dr. Keshavamurthy Vinay, Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh - 160 012, India. vinay.keshavmurthy@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bishnoi A, Lad D, Ashraf R, Banerjee N, Saikia UN, Vinay K. Graft versus host disease localized to striae distensae: An example of locus minoris resistentiae. Indian J Dermatol Venereol Leprol 2021;87:555-7.
Sir,
Allogeneic stem cell transplantation is frequently used in the treatment of hematologic malignancies. Graft versus host disease is among the common morbid complications that affect transplant recipients and is caused by the recognition of host antigens as foreign by the transplanted cells.1 Locus minoris resistentiae is a Latin term denoting a skin segment that presents lesser resistance to the development of disease as compared to the rest of the skin.2 This enhanced susceptibility of some cutaneous segments to develop a dermatosis is explained by the interplay of various cutaneous, immunological and neurological factors. Herein, we report a case of chronic graft versus host disease preferentially involving the sites of striae distensae as an example of locus minoris resistentiae.
A 13-year-old girl, with a prior diagnosis of acute myeloid leukemia, presented with itchy, erythematous papules on her back on day 128 of myeloablative, haploidentical hematopoietic cell transplantation. Her past history was significant for the development of acute cutaneous graft versus host disease and steroid-refractory, severe acute liver and gut graft versus host disease 1-month post-transplant, which had responded to antithymocyte globulin.
Examination revealed multiple fragile, erythematous to violaceous, scaly papules and plaques on her back, prominently localized to atrophic striae distensae, conforming precisely to their topography [Figure 1]. Her back also showed diffuse background post-inflammatory hyperpigmentation, reminiscent of acute cutaneous graft versus host disease. Nails and mucosae were normal. The rest of the skin was normal, and there was no obvious poikiloderma or sclerosis elsewhere on the skin. At that point of time, the patient was on tapering doses of prednisolone and mycophenolate mofetil. A diagnosis of late acute graft versus host disease (recurrent type) and chronic lichenoid graft versus host disease was considered, and skin biopsy was obtained from the papulosquamous lesions located on the striae.

- Graft versus host disease localized to striae distensae. Multiple fragile, erythematous to violaceous, scaly papules and plaques are present on the back, prominently localized to atrophic striae distensae. Diffuse background post-inflammatory hyperpigmentation is reminiscent of acute cutaneous graft versus host disease
Histopathology from a skin biopsy obtained from the lesions on the back showed hyperkeratosis, mild hypergranulosis and dense interface dermatitis with multiple apoptotic bodies, foci of satellite cell necrosis, pigment incontinence and fragmented collagen fibers [Figures 2a-c]. A diagnosis of lichenoid chronic graft versus host disease was confirmed. She was advised topical mometasone furoate 0.1% cream and tacrolimus 0.1% ointment for local application. The dose of prednisolone was increased. Sirolimus was added to mycophenolate mofetil and the lesions resolved within a month.
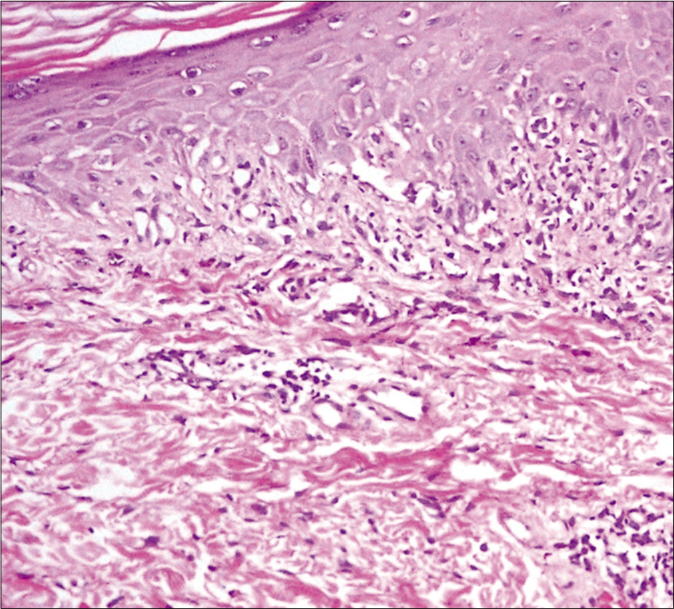
- Histopathological findings of skin biopsy of lesion on the back. The epidermis shows spongiosis with diffuse basal cell vacuolization and perivascular lymphocytic cell infiltration in the superficial dermis (H and E, ×100)
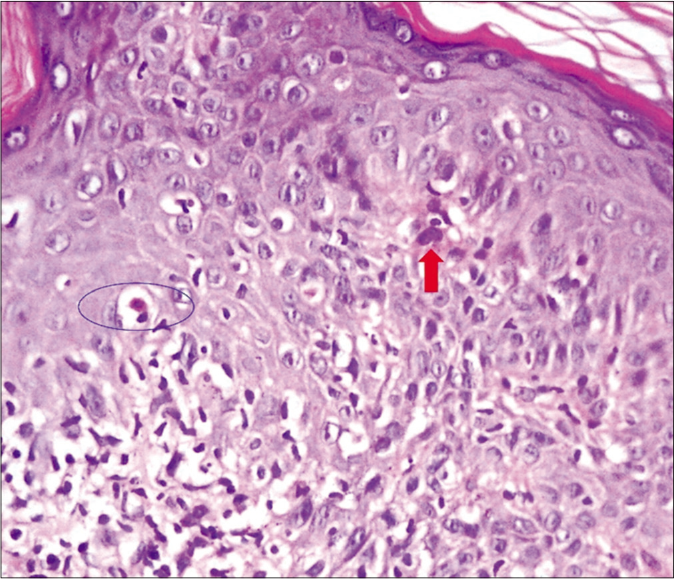
- Histopathological findings of skin biopsy of lesion on the back. The epidermis shows dyskeratotic keratinocyte (red arrow), satellite cell necrosis (blue circle) and lymphocytic exocytosis in the epidermis (H and E, ×200)
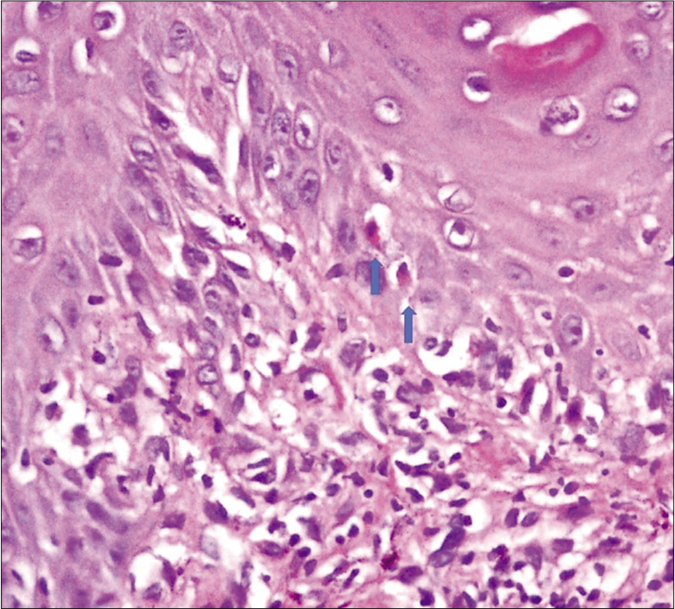
- Histopathological findings of skin biopsy of lesion on the back. Interface changes accompanied by basal cell vacuolization and apoptotic keratinocytes are seen in the epidermis (arrows) (H and E, ×400)
Graft-versus-host disease represents one of the most common complications of allogeneic hematopoietic stem cell transplantation.1 Its classification was previously based on the time point of 100 days (acute 100 days); though this was later revised to include cases of acute graft versus host disease that occurred beyond this time-point (persistent, recurrent and de-novo). Though acute graft-versus-host disease can be usually diagnosed clinically depending upon skin, liver and gastrointestinal manifestations, the same is not true for chronic graft versus host disease, where diagnosis relies on the presence of either diagnostic manifestations (classical lichen planus, poikiloderma or sclerosis), or distinctive manifestations that are subsequently proven to be chronic graft versus host disease on histopathology (lichenoid or sclerotic features in the skin).3 For our patient, since she presented on day 128 post-transplant, and the lesions were not very suggestive of classic lichen planus; both diagnoses were considered; that is, late acute (recurrent) or chronic lichenoid graft versus host disease, and histopathology established the diagnosis to be chronic lichenoid graft versus host disease.
The index patient had also developed classic acute graft versus host disease (affecting skin, liver and gut) initially (after 1 month of transplant); following which she gradually developed extensive striae distensae probably because of the concomitant pubertal growth spurt and intake of systemic corticosteroids. Striae distensae represent traumatized dermal collagen zones, and their selective affliction by chronic lichenoid graft versus host disease in the index patient aptly demonstrates the phenomenon of locus minoris resistentiae. An easy transit and access of lymphocytes to cutaneous antigens through the damaged dermal matrix in the striae might be a plausible explanation for this occurrence. Chemotherapy-induced skin eruptions localized to radiotherapy site4 and melanoma metastasis;5 as well as infective conditions like verruca6 and tinea barbae7 localized to verrucous epidermal nevus and scar tissue, respectively, are other examples of locus minoris resistentiae. Fixed drug reaction secondary to minocycline localizing to areas of herpes zoster and burn scars has also been described.8 Vitiligo,9 psoriasis,10 plane xanthomas,11 drug-induced exanthems12 leukemia cutis13 and lichen sclerosus14 are some of the other dermatosis that have been reported to localize to striae distensae.
Though graft versus host disease is a systemic affliction, the skin is affected preferentially; in both acute and chronic forms. Atypical cutaneous variants have been previously described [Table 1]15-18 highlighting the effect of the microenvironmental and constitutional factors on the final presentation of the disease. Blaschkoid (both acute and chronic)19 and chronic sclerotic graft versus host disease conforming to the sites of the waistband, radiotherapy, needle sticks and healed herpes zoster has been previously reported.20 Lichenoid graft versus host disease localizing to striae has been sparingly reported before.21 All these cases highlight previously described Wolf’s isotopic or Koebner’s isomorphic response; both of which can now be clubbed into the unifying concept of an immunocompromised cutaneous district or the locus minoris resistantiae,22 which the index case aptly represents, though for a rarer disease.
| Acute graft-versus-host disease | Chronic graft-versus-host disease |
|---|---|
| Psoriasiform | Psoriasiform |
| Follicular erythema/lichenoid | Follicular erythema/lichenoid |
| Contact dermatitis | Acral keratosis |
| Type-II pityriasis rubra pilaris-like | Pityriasis rosea-like |
| Hand-foot-mouth disease-like | Annular scleroderma-like plaques |
| Localized to tattoo skin | Eczematoid |
| Atopic dermatitis-like | |
| Exfoliative dermatitis | |
| Dermatomyositis-like | |
| Lupus erythematosus-like | |
| Hypertrophic lupus erythematosus-like | |
| Erythema multiforme-like | |
| Total body leukoderma | |
| Koebner isomorphic pattern | |
| Blaschko-linear | |
| Black hairy tongue | |
| Nodular/keloidal scleroderma-like |
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Graft-versus-host disease: Part I. Pathogenesis and clinical manifestations of graft-versus-host disease. J Am Acad Dermatol. 2012;66:515.e1-18.
- [CrossRef] [PubMed] [Google Scholar]
- The immunocompromised district: A unifying concept for lymphoedematous, herpes-infected and otherwise damaged sites. J Eur Acad Dermatol Venereol. 2009;23:1364-73.
- [CrossRef] [PubMed] [Google Scholar]
- Classification systems for chronic graft-versus-host disease. Blood. 2017;129:30-7.
- [CrossRef] [PubMed] [Google Scholar]
- An acneiform eruption exhibiting locus minoris resistentiae after whole-brain radiation and vemurafenib therapy. J Eur Acad Dermatol Venereol. 2017;31:e209-10.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous eruption secondary to immunotherapy for metastatic melanoma limited to sites of locoregional melanoma metastases: A possible variant of locus minoris resistentiae. JAMA Dermatol. 2018;154:846-7.
- [CrossRef] [PubMed] [Google Scholar]
- Appearance of verruca over linear verrucous epidermal nevus-An example of locus minoris resistentiae: A report of three cases. Indian Dermatol Online J. 2018;9:334-7.
- [Google Scholar]
- Tinea barbae spreading to locus minoris resistentiae. Eur J Dermatol. 2009;19:173-4.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple fixed drug eruption to minocycline at sites of healed burn and zoster: An interesting case of locus minoris resistentiae. JAAD Case Rep. 2017;3:392-4.
- [CrossRef] [PubMed] [Google Scholar]
- Köebner phenomenon induced by striae distensae in a vitiligo patient. Ann Dermatol. 2017;29:633-4.
- [CrossRef] [PubMed] [Google Scholar]
- Pustular psoriasis occurring on the striae distensae: Isotopic phenomenon/Koebner's phenomenon. Indian J Dermatol. 2016;61:239.
- [CrossRef] [PubMed] [Google Scholar]
- Diffuse normolipemic plane xanthoma on striae. J Eur Acad Dermatol Venereol. 2017;31:e452-3.
- [CrossRef] [PubMed] [Google Scholar]
- Clindamycin-induced maculopapular exanthema with preferential involvement of striae distensae: A Koebner phenomenon? Acta Dermatovenerol Croat. 2018;26:61-3.
- [Google Scholar]
- Striae gravidarum leukaemia cutis: A rare manifestation of acute myeloid leukaemia. BMJ Case Rep. 2017;2017:bcr2016218428.
- [CrossRef] [PubMed] [Google Scholar]
- Lichen sclerosus on the sites of striae distensae and a surgical scar in a patient with coexistent morphea. Acta Dermatovenerol Croat. 2019;27:44-6.
- [Google Scholar]
- Atypical manifestations of graft-versus-host disease. J Am Acad Dermatol. 2015;72:690-5.
- [CrossRef] [PubMed] [Google Scholar]
- Late-onset acute graft-versus-host disease mimicking hand, foot, and mouth disease. Indian Dermatol Online J. 2016;7:509-11.
- [CrossRef] [PubMed] [Google Scholar]
- Acute graft-versus-host disease arising within tattooed skin. JAAD Case Rep. 2015;1:114-6.
- [CrossRef] [PubMed] [Google Scholar]
- Nodular sclerodermatous chronic cutaneous graft-versus-host disease (GvHD): A new clinicopathological variant of cutaneous sclerodermatous GvHD resembling nodular/Keloidal scleroderma. Am J Dermatopathol. 2017;39:910-3.
- [CrossRef] [PubMed] [Google Scholar]
- Blaschkoid acute graft-vs-host disease. JAMA Dermatol. 2018;154:494-5.
- [CrossRef] [PubMed] [Google Scholar]
- Localization of sclerotic-type chronic graft-vs-host disease to sites of skin injury: Potential insight into the mechanism of isomorphic and isotopic responses. Arch Dermatol. 2011;147:1081-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous acute graft-versus-host disease with isomorphic disposition over striae distensae in a 12-year-old girl. Int J Dermatol. 2017;56:e37-8.
- [CrossRef] [PubMed] [Google Scholar]
- Locus minoris resistentiae: An old but still valid way of thinking in medicine. Clin Dermatol. 2014;32:553-6.
- [CrossRef] [PubMed] [Google Scholar]





