Translate this page into:
Granulomatous and eccrinotropic lymphomatoid papulosis
Correspondence Address:
Uday Khopkar
Department of Dermatology, Seth GS Medical College and KEM Hospital, Parel, Mumbai - 400 012
India
| How to cite this article: Jain N, Gutte R, Jadhav P, Khopkar U. Granulomatous and eccrinotropic lymphomatoid papulosis. Indian J Dermatol Venereol Leprol 2012;78:82-84 |
Abstract
Lymphomatoid papulosis has been classically described as a chronic, recurrent and self-healing papulonecrotic or papulonodular skin eruption, which is clinically benign and histopathologically malignant. The histologic characteristics of lymphomatoid papulosis are suggestive of a cluster of differentiation 30+ (CD30+) malignant lymphoma, and it is best regarded as a low grade cutaneous T cell lymphoma (CTCL). We hereby report a case of granulomatous and eccrinotropic lymphomatoid papulosis in a 40- year-old male. There was no systemic involvement. The patient was treated with low dose oral methotrexate with good response.Introduction
The term lymphomatoid papulosis (LyP) was coined by Macaulay in 1968 to describe a condition characterized by spontaneously appearing, asymptomatic to mildly itchy, red to brown papulonodular lesions over the trunk and extremities. [1],[2] The lesions typically undergo central necrosis and crusting, and later heal spontaneously within 6 to 8 weeks leaving transient hyperpigmentation or varioliform scars. Co-existence of lesions in various stages of evolution is characteristic. The lesions, though self healing, are usually recurrent with a waxing and waning course, that extends from months to years. In most cases, the disorder apparently follows a benign course with an overall good prognosis, though paradoxically, histopathology shows features of malignancy with large hyperchromatic cells that in many instances, tend to invade and erode the epidermis. [1] These large atypical cells are cluster of differentiation 30+ (CD30+) lymphocytes suggestive of a low grade malignant cutaneous T cell lymphoma (CTCL), accounting for 15% of all CTCL. [3]
Though three distinct histologic subtypes (type A, B and C) have been described, a predominant granulomatous and eccrinotropic variant as in this case, is a rarity. [1],[2]
Case Report
A 40 year old male, presented to us with multiple, itchy, erythematous papulo-nodular skin lesions with central necrosis, occurring in crops initially over the trunk, and later over the extremities since last 12 years. The lesions were self healing, but recurrent. Individual lesion started as a nodule, underwent central necrosis and healed spontaneously within a week with residual hyperpigmentation. There was no history of insect bite or unexplained fever and weight loss. Examination revealed multiple hyperpigmented papules and nodules with central crusting over the upper extremities [Figure - 1], thighs and the abdomen, healing with hyperpigmentation and mild atrophy and not associated with nodal enlargement. Systemic examination revealed no abnormality.
 |
| Figure 1: Multiple crusted papulo-nodules over arm in different stages of evolution |
The patient was further investigated considering a clinical differential diagnosis of lymphomatoid papulosis and pityriasis lichenoides et varioliformis acuta (PLEVA). Skin biopsy done from a papule revealed a dense infiltrate in the dermis composed of multiple large atypical lymphocytes with large hyperchromatic nuclei, and increased nucleo-cytoplasmic ratio, admixed with eosinophils [Figure - 2], in a diffuse and nodular distribution without epidermotropism. There were also plenty of histiocytes′ forming small granulomas at places and nodular aggregates in an eccrinotropic pattern [Figure - 3]a and b. On immunohistochemistry, the atypical cells stained positively for leukocyte common antigen (LCA) and CD30 [Figure - 4]a and b, but were negative for CD 3 and 5. Based on clinico-pathologic correlation, a final diagnosis of granulomatous and eccrinotropic lymphomatoid papulosis was made. The patient was subsequently evaluated for oral methotrexate therapy and a complete hemogram, chest radiograph and ultra-sound of the abdomen were done which revealed no abnormality. A weekly dose of oral 15 mg methotrexate (MTX) was started after the test dose which was subsequently tapered to 12.5 mg after 4 weeks as all the lesions healed and there were no new lesions. Presently the patient is on a weekly dose of 7.5 mg with no new lesions in the last 5 months.
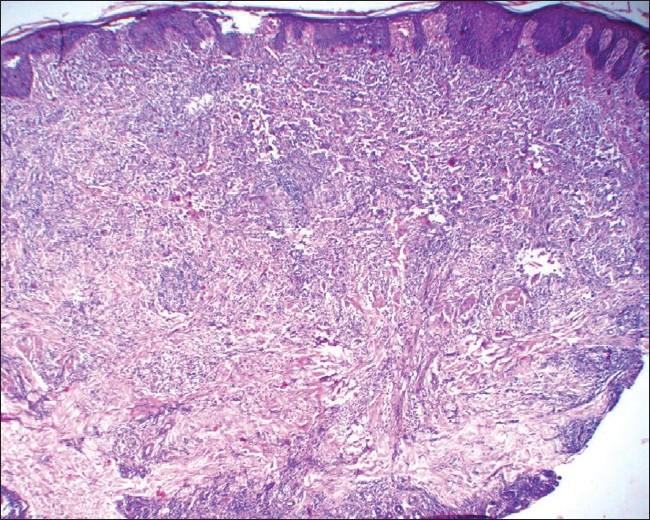 |
| Figure 2: Diffuse dermal mixed infiltrate with predominance of non-epidermotropic large atypical lymphocytes having hyperchromatic nuclei (H and E, ×25) |
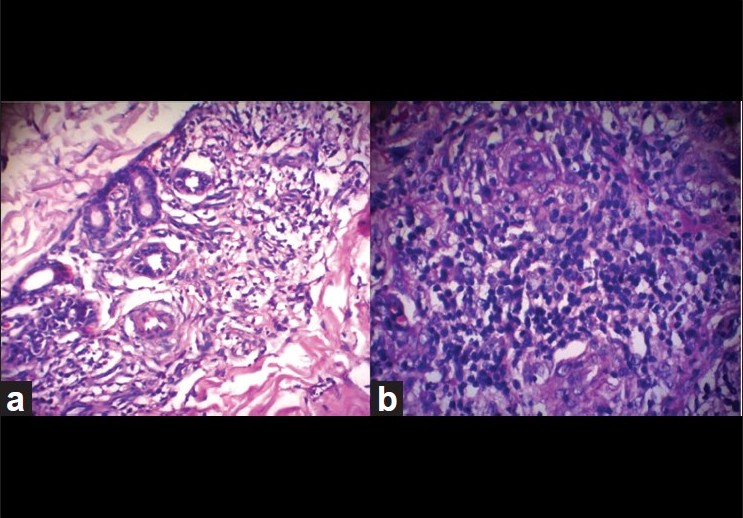 |
| Figure 3: Atypical lymphocytes around eccrine coils (a) and with multiple histiocytes respectively (b) (H and E, ×100) |
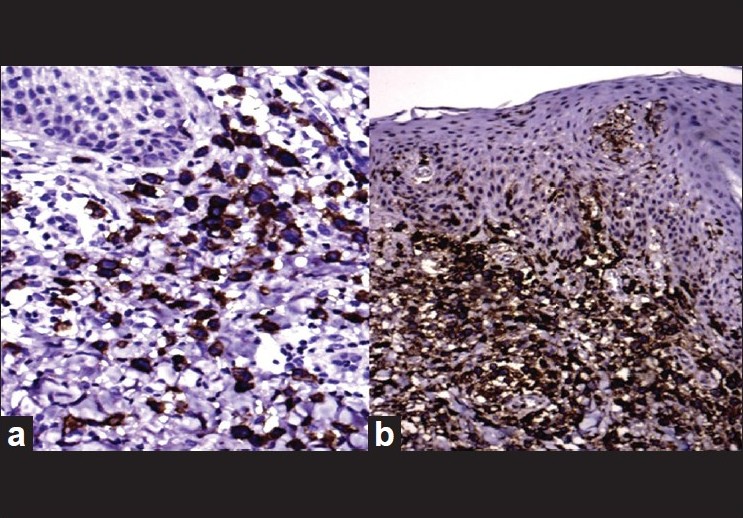 |
| Figure 4: Immunohistochemistry showing CD30 positive (a) and Leukocyte common antigen positive infiltrate (b) (H and E, ×100) |
Discussion
Lymphomatoid papulosis is characterized clinically by papular or papulo-necrotic eruptions with a waxing and waning course. Lesions in different stages of evolution and regression may be seen. Individual lesions usually last for 4-6 weeks, but the eruption persists indefinitely and a long duration of upto 20 years is not uncommon. [1]
Three histopathological variants of LyP namely, type A, B and C have been described though they do not differ clinically. Type A lesions are characterized by wedge shaped, initially nonepidermotropic infiltrate with scattered or small clusters of large atypical cells and have many features similar to cutaneous Hodgkin′s disease. Type B lesions have perivascular or band like infiltrate of lymphocytes with epidermotropism, and may simulate mycosis fungoides. Type C lesions show monotonous population or large clusters of CD30 positive T cells with few inflammatory cells, and resemble primary cutaneous CD30 positive anaplastic large cell lymphoma (ALCL). The standard histologic description of LyP emphasize wedge shaped dermal infiltrates with angiocentricity, a polymorphous inflammatory background containing eosinophils and plasma cells, variable epithelial and vessel wall necrosis, and lymphocytic migration into the epidermis. [1],[2],[3] The granulomatous and eccrinotropic LyP is a rare histologic variant. Crowson et al. described 9 cases of granulomatous and eccrinotropic LyP, 5 being men and 4 women. Most of the patients were elderly with a mean age at diagnosis 40.6 years and the average duration of disease was 3.7 years. [2] Our patient was a 40 year old male and duration of disease was 12 years.
Wantzin et al.[3] found a good clinical response to oral methotrexate in all their three cases. Also Yip et al.[4] have reported MTX to be a safe and effective treatment for LyP in children. In a series of nine cases of granulomatous and eccrinotropic LyP by Crowson et al. three patients received MTX: first patient showed complete resolution of lesions without recurrence; no response was seen in second patient; and, third patient was just started on MTX with no resolution of lesions yet. [2] In our case, excellent response was seen to oral 15 mg weekly methotrexate. Various other treatment modalities including topical, systemic and intra-lesional corticosteroids, systemic antibiotics, natural sunlight, psoralen and ultraviolet A (PUVA) therapy and narrowband ultraviolet B therapy have been described but with varying success. The decision to actively treat childhood LyP is controversial, since this disease is self-resolving, but as mentioned above methotrexate is effective and safe. In adult-onset LyP, low-dose MTX between 10-25 mg weekly is recommended as the treatment of choice for aggressive or refractory disease. [3],[4]
The overall prognosis for LyP is good and the disease follows a benign course, though clonal T cell gene rearrangements can be demonstrated in 70% cases. LyP may be preceded by, associated with, or followed by another cutaneous lymphoma like Hodgkin′s disease, cutaneous T cell lymphoma or anaplastic large cell lymphoma (ALCL). Some cases may resolve spontaneously. However, some cases may have an aggressive course, and transformation to true lymphoma can occur variably with increasing duration of disease, and long term follow-up is warranted. [5]
| 1. |
Macaulay WL. Lymphomatoid papulosis. Int J Dermatol 1978;17:204-12.
[Google Scholar]
|
| 2. |
Crowson AN, Baschinsky DY, Kovatich AL, Magro C. Granulomatous eccrinotropic lymphomatoid papulosis. Am J Clin Pathol 2003;119:731-9.
[Google Scholar]
|
| 3. |
Wantzin GL, Thomsen K. Methotrexate in lymphomatoid papulosis. Br J Dermatol 1984;111:93-5.
[Google Scholar]
|
| 4. |
Yip L, Darling S, Orchard D. Lymphomatoid papulosis in children: Experience of five cases and the treatment efficacy of methotrexate. Australas J Dermatol 2011;52:1-5.
[Google Scholar]
|
| 5. |
Jerajani HR, Ambade G. Lymphoproliferative disorders. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. 3 rd ed. India: Bhalani Publisher; 2008.
[Google Scholar]
|
Fulltext Views
3,380
PDF downloads
2,437





