Translate this page into:
Granulomatous rosacea mimicking eyelid dermatitis
2 Departments of Histopathology, PGIMER, Chandigarh, India
Correspondence Address:
Sanjeev Handa
Department of Dermatology, Venereology and Leprology, PGIMER, Chandigarh-160 012
India
| How to cite this article: Ajith C, Dogra S, Radotra B D, Handa S. Granulomatous rosacea mimicking eyelid dermatitis. Indian J Dermatol Venereol Leprol 2005;71:366-365 |
 |
 |
 |
 |
 |
 |
Sir,
Allergic contact dermatitis (ACD) due to topical medications for the eyes accounts for about 80% of cases of eyelid dermatitis.[1],[2] Sometimes, other periorbital dermatoses may be mistakenly labelled as ACD due to topical ophthalmic medications. Here, we report a patient of granulomatous rosacea with predominant periocular involvement, who was initially diagnosed as contact dermatitis secondary to topical eye medications.
A 60-year-old man presented with complaints of itchy eruptions around his eyes for the past 20 days. He correlated the onset of symptoms with the use of topical medications in his eyes prescribed by ophthalmologists for allergic conjunctivitis. His medications included sodium carboxymethyl cellulose, stabilized oxychlorocomplex, ketorolac tromethamine, benzalkonium chloride and polyvinyl alcohol.
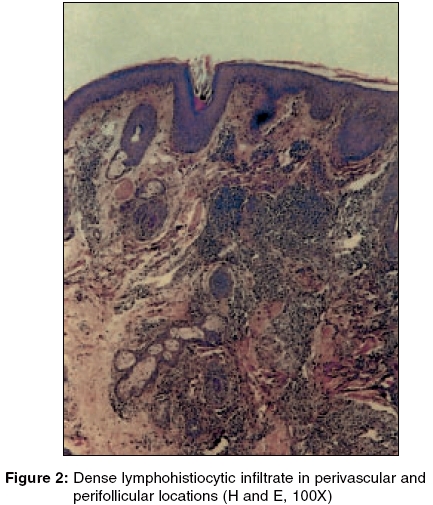
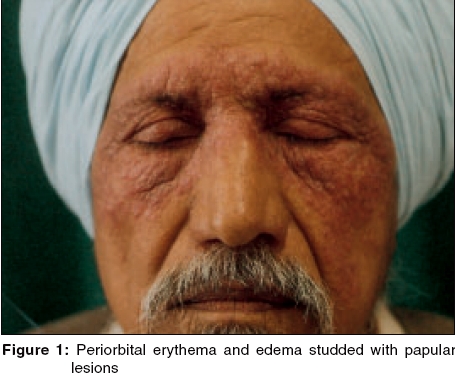
On examination, both periorbital regions and the root of the nose were diffusely erythematous, edematous, studded with multiple erythematous papular lesions, and minimally scaly [Figure - 1]. The lesions extended on to the cheeks and up to the mid-forehead. A provisional diagnosis of ACD due to ophthalmic medications was made. Patch testing with the Indian standard series and his topical medications as antigens was negative. He was prescribed topical fluticasone dipropionate cream and was advised to avoid the ocular medications he was using. At follow-up after 2 weeks, the response was not satisfactory. Hence, a biopsy was done from the skin lesions. A H and E stained histopathological section showed a normal epidermis and dense collections of predominantly lymphocytic infiltrates surrounding the dilated blood vessels and hair follicles; features consistent with granulomatous rosacea [Figure - 2]. A final diagnosis of granulomatous rosacea was made. Topical fluticasone dipropionate was withheld and he was prescribed doxycycline 100 mg bid PO and topical metronidazole gel (0.75%) for local application twice daily. At follow-up after 8 weeks, there was almost complete clearance of the skin lesions [Figure - 3] and improvement of his eye symptoms. Subsequently, the initial diagnosis of allergic conjunctivitis was revised by the ophthalmologists to ocular rosacea.
Granulomatous rosacea is a dermatosis characterized by small, discrete, yellowish brown papules and pustules distributed across the center of the face and eyelids. The eyelids, lower part of the forehead, nasolabial folds, cheeks and perioral areas are frequent sites of involvement. [3] Histopathological examination reveals perivascular and perifollicular noncaseating epithelioid granulomas. The prevalence of ocular involvement in rosacea varies between 3% to 58% in different reports.[3],[4] Various ophthalmological manifestations that can occur in rosacea include blepharitis, conjunctivitis, iritis, iridocyclitis, hypopyoniritis, and keratitis. Other unusual presentations of rosacea include rosacea fulminans, persistent edema of rosacea and rosacea conglobata. Rosacea fulminans is considered an extreme form of the disease. There may be a rapid onset without any prior history of rosacea. In persistent edema of rosacea, a hard, non-pitting edema is found on the forehead, glabella, upper eyelids, nose or cheeks. Rosacea conglobata is characterized by a chronic, progressive course with haemorrhagic nodular abscesses and indurated plaques.[5]
The temporal correlation between the application of the ophthalmic topical medications and appearance of symptoms led to an initial misdiagnosis of ACD in our patient. Absence of prior symptoms suggestive of rosacea also contributed to this.
This report highlights the importance of considering rosacea as a diagnostic possibility in cases of eyelid dermatitis.
| 1. |
Guin JD. Eyelid dermatitis: A report of 215 patients. Contact Dermatitis 2004;50:87-90.
[Google Scholar]
|
| 2. |
Guin J. Eyelid dermatitis: a report of 203 cases. J Am Acad Dermatol 2002;47:755-65.
[Google Scholar]
|
| 3. |
Patrinely JR, Font RL, Anderson RL. Granulomatous acne rosacea of the eyelids. Arch ophthalmol 1990;108:561-3.
[Google Scholar]
|
| 4. |
Michel JL, Cabibel F. Frequency, severity and treatment of ocular rosacea during cutaneous rosacea. Ann Dermatol Venereol 2003;130:20-4.
[Google Scholar]
|
| 5. |
Beuchner SA. Rosacea: An update. Dermatology 2005;210:100-8.
[Google Scholar]
|
Fulltext Views
2,496
PDF downloads
1,196





