Translate this page into:
Herpes zoster motor neuropathy: A clinical and electrophysiological study
2 Department of Neuromedicine, Andhra Medical College, King George Hospital, Visakhapatnam, Andhra Pradesh, India, India
Correspondence Address:
G Raghurama Rao
Gopal Sadan, D. No.: 15-1-2C, Naoroji Road, Maharanipeta, Visakhapatnam - 530 002
India
| How to cite this article: Gopal K, Sarvani D, Krishnam Raju P V, Rao G R, Venkateswarlu K. Herpes zoster motor neuropathy: A clinical and electrophysiological study. Indian J Dermatol Venereol Leprol 2010;76:569-571 |
Sir,
Neurological complications of herpes zoster include post-herpetic neuralgia, meningoencephalitis, transverse myelitis, Gullian-Barre syndrome, peripheral nerve palsy, cranial nerve palsies and deafness. [1] Among these complications of herpes zoster, involvement of motor neurons is uncommon and segmental motor paralysis of the limbs is seen in only 5% of these cases. [2] We observed three cases of limb paralysis following herpes zoster out of 100 cases of herpes zoster in a 6-month period from May 2004 to October 2004.
Our first case was a 49-year-old male who presented with weakness in the left lower limb and foot drop of 10 days duration. On enquiry, the patient gave a history of painful vesicular eruption over the left lower leg 3 weeks ago and, on examination, discrete hyperpigmented macules were seen in the L5-S1 dermatome on the medial aspect of the left lower limb and foot, suggestive of healed lesions of herpes zoster. The second case was a 65-year-old male diabetic who presented with right wrist drop of 3 days duration. Three weeks ago, he had painful grouped vesicular lesions over the medial side of the right arm. There were grouped hypopigmented macules over the medial aspect of the right arm, extending from the axilla to the elbow joint (C8-T1 dermatome), suggestive of healed herpes zoster. The third case was a 49-year-old male who presented with inability to completely abduct the right shoulder and flattening of the deltoid contour on the right arm since 5 days. Two weeks ago, the patient had painful vesicular rash over the posterolateral aspects of the right shoulder and there were grouped hypopigmented and hyperpigmented macules over the lateral and posterior aspects of the right shoulder, suggestive of healed lesions of herpes zoster (C5-C6 dermatome). In all the three cases, there was no history of prior trauma. In all the three cases, motor neuropathy developed 2-3 weeks after the onset of skin lesions of zoster and the patients did not take specific treatment with acyclovir for herpes zoster.
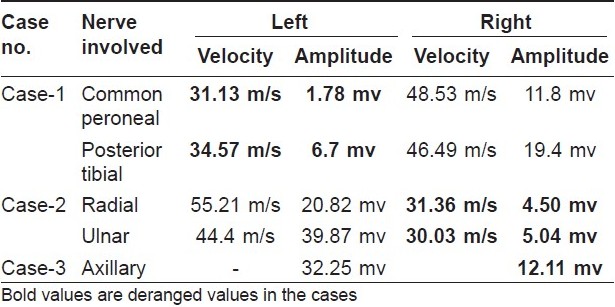
In all the three cases, power of the involved group of muscles was markedly decreased compared to other groups of muscles. Complete neurological examination revealed no other abnormality. In all the cases, there were no hypopigmented anesthetic patches, all the peripheral nerves were normal in consistency, were not thickened and there was no clinical evidence of Hansen′s disease. Hence, skin smear and skin biopsy were not performed. Routine hematological and biochemical tests were within normal limits and serological tests for syphilis and human immunodeficiency virus screening tests were negative in all the three cases. Varicella zoster virus (VZV)-IgG antibody titers were markedly raised in all the three cases - 440 U/ml, 97.41U/ml and 156.64 U/ml in the first, second and third cases, respectively (normal range: <9 U/ml, negative; >11U/ml, positive). In all the cases, magnetic resonance imaging of the spine revealed early degenerative changes with no evidence of nerve root compression. Nerve conduction studies were carried out in all these cases, which showed involvement of the left common peroneal and posterior tibial nerves in the first case, right radial and ulnar nerves in the second case and right axillary nerve in the third case [Table - 1]. All these cases were managed with physiotherapy and complete recovery was observed after 6-12 weeks.
Pathogenesis of motor paralysis following herpes zoster may involve viral invasion and inflammation of the motor neurons of the anterior horn cells by the VZV at the same time and site as the cutaneous eruption. [3] Nerve conduction studies in all our three cases showed decreased nerve conduction velocity and decreased amplitude of action potential of involved nerves, suggestive of significant axonal involvement. Similar findings in electrophysiological studies conducted in herpes zoster limb paralysis were reported in previous studies. [4] The latency period between the onset of vesicular eruption and the development of limb weakness may vary from 1 day to 4 months. [2] In all our three cases, limb paralysis developed 2-3 weeks after the onset of skin lesions of zoster. The prognosis for zoster segmental weakness is generally good, with complete recovery in 55-75% of the cases in <1 year. [2] Previous literature suggests that systemic steroids along with acyclovir are beneficial in cases of Ramsay Hunt Syndrome for recovery of facial nerve paralysis but are not indicated in limb paralysis. Recovery from paralysis was uniformly good in all our three cases within 6-12 weeks with physiotherapy.
Limb paralysis following herpes zoster has been reported infrequently in India [5] and in other parts of the world. [2],[3],[4] In endemic areas, leprosy is the most common cause for all peripheral limb paralysis, like foot drop and wrist drop, but VZV can also rarely produce limb paralysis. In view of the high prevalence of herpes zoster in recent times, this uncommon complication of herpes zoster should also be considered in all peripheral limb paralysis cases. The purpose of this report is to create awareness about this uncommon complication of herpes zoster among dermatologists, physicians and general practitioners.
| 1. |
Straus SE, Oxman MN, Schmader KE. Varicella and herpes zoster. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's Dermatology in General Medicine. 7 th ed. New York: Mc Graw Hill; 2008. p. 1885-98.
th ed. New York: Mc Graw Hill; 2008. p. 1885-98.'>[Google Scholar]
|
| 2. |
Cockerell OC, Ormerod IE. Focal weakness following herpes zoster. Neurol Neurosurg Psychiatry 1993;56:1001-3.
[Google Scholar]
|
| 3. |
Grant BD, Rowe CR. Motor paralysis of the extremities in herpes zoster. J Bone Joint Surg 1961;43:885-96.
[Google Scholar]
|
| 4. |
Cruz-Velarde JA, Muρoz-Blanco JL, Traba A, Nevado C, Ezpeleta D. Segmental motor paralysis caused by the varicella zoster virus. Clinical study and functional prognosis. Rev Neurol 2001;32:15-8.
[Google Scholar]
|
| 5. |
Nigam P, Dayal SG. Paralysis of the limb complicating herpes zoster. Indian J Dermatol Venereol Leprol 1978;44:293-4.
[Google Scholar]
|
Fulltext Views
6,224
PDF downloads
1,603





