Translate this page into:
Hidradenitis suppurativa involving the preauricular region : An unusual location
Correspondence Address:
Shalu Jain
Department of Dermatology, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi - 110 002
India
| How to cite this article: Jain S, Sardana K, Garg VK, Sinha S. Hidradenitis suppurativa involving the preauricular region : An unusual location. Indian J Dermatol Venereol Leprol 2012;78:229 |
Sir,
Hidradenitis suppurativa (HS) is a chronically relapsing disfiguring skin disease primarily affecting the axillae, groin and inframammary regions, although, occasionally, it can be seen in the atypical sites. Here, we report a case of unusual location of HS involving the bilateral preauricular region. To the best of our knowledge, the preauricular region has not been reported previously as a site of HS.
A 30-year-old male presented with recurrent episodes of multiple, painful swellings with foul-smelling pus discharge over the bilateral preauricular region for the past 2 years. The lesions began as firm, reddish, raised lentil-sized lesions that gradually enlarged, softened and ultimately ruptured, discharging yellow-colored foul-smelling pus and, eventually, over a period of few weeks to months, the lesions healed with scarring but only to recur again. He took multiple courses of antibiotics without much relief. There was no history of diarrhea, prolonged fever, chronic cough or weight loss. Cutaneous examination revealed a single, well-defined, firm, indurated, erythematous plaque of size 1 cm × 1 cm over the right preauricular region with few comedones in the surrounding skin [Figure - 1], while the left preauricular region showed a single well- to ill- defined erythematous, nonindurated, tender plaque of size 3 cm × 2 cm with overlying papules and a single sinus at the lower end, discharging thick, foul-smelling pus [Figure - 2]. Other areas including the axilla, groin, buttocks and anogenital region were normal. Regional lymphadenopathy was characteristically absent. With these clinical findings, we kept the differential diagnosis of HS, scrofuloderma and recurrent furunculosis.
 |
| Figure 1: Single, well-defined, firm, indurated erythematous plaques over the right preauricular region |
 |
| Figure 2: Left preauricular region showing an erythematous plaque with overlying papules and a single discharging sinus at the lower end |
Investigations were carried out to look for any evidence of tuberculosis, human immunodeficiency virus (HIV) infection and diabetes mellitus. Complete blood count was normal, except for neutrophilia (82%). ESR was 70 mm fall/h by the Westergren method. X-ray chest and mandible, Mantoux, blood sugar and HIV antibodies by enzyme-linked immunosorbent assay (ELISA) were normal. Pus culture from the lesions showed no growth. Tissue culture did not reveal acid fast bacilli. A 4-mm punch biopsy from the left preauricular lesion revealed an ulcerated epidermis lined by inflammatory granulation tissue with foreign body giant cells scattered on the surface as well as deeper in the dermis and focally entrapping the keratin [Figure - 3]. The upper and deep dermis showed diffuse mixed inflammatory infiltrate comprising of lymphocytes, plasma cells, histiocytes and few neutrophils, especially around the hair follicles and blood vessels. No definite granuloma was identified [Figure - 4]. Stain for the acid fast bacilli was negative. These findings were suggestive of hidradenitis suppurativa. Considering the mild disease, we prescribed a short course of oral doxycycline with topical retinoids and clindamycin gel following which lesions healed with deep cord-like scarring [Figure - 5], but new lesions continued to develop which also responded to the same treatment.
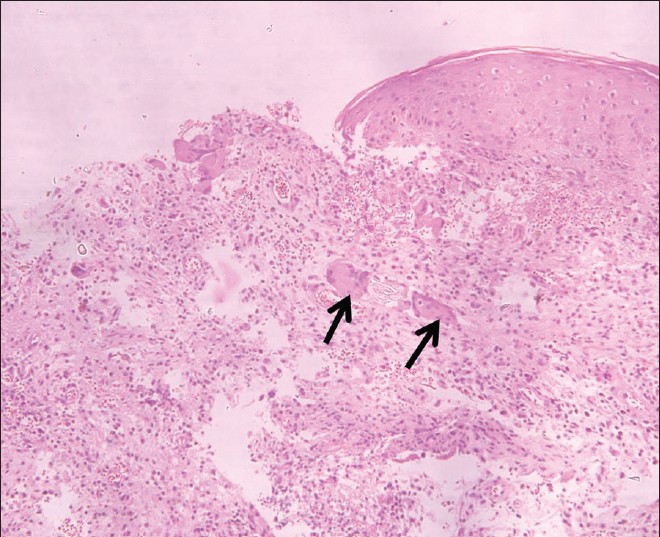 |
| Figure 3: Histopathology showing an ulcerated epidermis lined by inflammatory granulation tissue with foreign body giant cells scattered on the surface as well as deeper in the dermis and focally entrapping the keratin (arrows) (H and E, × 250) |
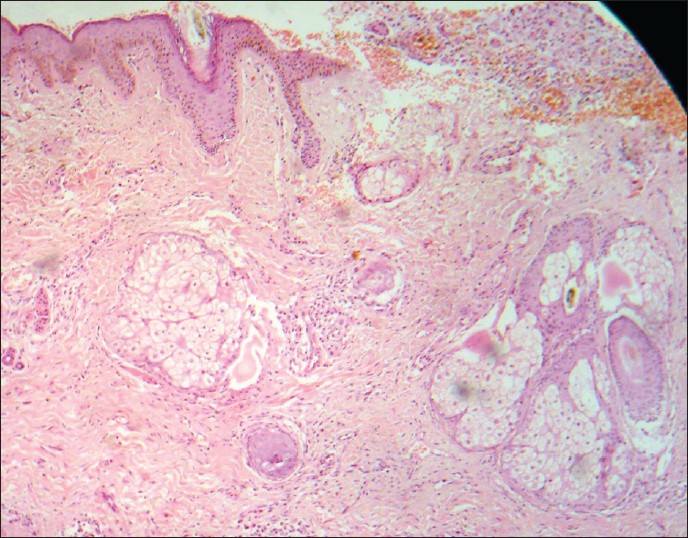 |
| Figure 4: The upper and deep dermis showed diffuse mixed inflammatory infiltrate comprising of lymphocytes, plasma cells, histiocytes and few neutrophils, especially around hair follicles and blood vessel (H and E, × 100) |
 |
| Figure 5: Deep cord-like scarring at the site of healed lesions. Comedones (white arrows) and terminal hairs (black arrow) are also seen in the surrounding skin |
HS is characterized by recurrent, painful, deep-seated nodules and abscesses, draining sinuses, fibrosis and scarring, involving predominantly the axilla and groin, sites that carry terminal hairs and apocrine glands. [1] Other areas are occasionally affected. These atypical sites include buttocks, [2] areola, infra- mammary and inter-mammary fold, [3] abdomen, chest, [4] scalp, [5] zygomatic and temporal areas of face and periorbital region, [6] eyelids, [7] external auditory meatus, ear lobes, retroauricular fold [8] and the posterior thighs. [9] However, preauricular involvement by HS has not been reported earlier in the literature. In a large series reported by Poitrine et al., [4] HS in atypical locations was found to be significantly more common in men (47.1%) than in women (14.8%). Involvement of unusual sites by HS is more frequent in HIV/AIDS patients, which could be due to HIV-induced immunosuppresion and immunological changes that significantly alter the clinical course of the chronic disease. [9]
Earlier, HS was thought to be a disorder of apocrine origin. But, in recent years, various histopathological studies have shown that the origin of HS lesions is in the hair follicle. [10] Thus, HS is now considered to be caused by follicular obstruction, a primary event with secondary involvement of apocrine glands. Thus, the atypical sites for HS are even those rich in terminal hair follicles. The presence of terminal hairs in preauricular region in our patient explains the occurrence of HS at this unusual site. Management should be appropriately tailored according to the severity and distribution of HS as well as the extent of impairment of quality of life of the patient. Treatment options include topical and systemic antibiotics, retinoids, anti-androgens, estrogens, oral steroids, anti-TNFα agents and, more recently, Nd: YAG and carbon dioxide laser. The most effective treatment of HS is excision of the affected area followed by split-skin grafting or leaving to heal by secondary intension.
Because the diagnosis of HS is primarily clinical, hence, if present at atypical sites, may go unrecognized and may be misdiagnosed as scrofuloderma and recurrent furunculosis. We hereby strive to bring to the notice of others the occurrence of HS at preauricular sites. In addition to the typically involved sites, HS can occur at any site that carries terminal hairs and/or apocrine glands.
| 1. |
Jansen T, Plewig G. Acne inversa. Int J Dermatol 1998;37:96-100.
[Google Scholar]
|
| 2. |
Liron R, Torralba JA, Pellicer E, Morales G, Martin JG, Miguel J, et al. Treatment of long-standing extensive perianal hidradenitis suppurativa using double rotation plasty, V-Y plasty and free grafts. Int J Colorectal Dis 2004;19:73-8.
[Google Scholar]
|
| 3. |
Li EN, Mofid MM, Goldberg NH, Silverman RP. Surgical management of hidradenitis suppurativa of the nipple-areolar complex. Ann Plast Surg 2004;52:220-3.
[Google Scholar]
|
| 4. |
Poitrine FC, Revuz JE, Wolkenstein P, Viallette C, Gabison G, Pouget F, et al. Clinical characteristics of a series of 302 French patients with hidradenitis suppurativa, with an analysis of factors associated with disease severity. J Am Acad Dermatol 2009;61:51-7.
[Google Scholar]
|
| 5. |
Mengesha YM, Holcombe TC, Hansen RC. Prepubertal hidradenitis suppurativa: Two case reports and review of the literature. Pediatr Dermatol 1999;16:292-6.
[Google Scholar]
|
| 6. |
Greer KE, Charlottesville VA. Facial involvement with hidradenitis suppurativa. Arch Dermatol 1974;109:408.
[Google Scholar]
|
| 7. |
Sachs DD, Gordon AT. Hidradenitis suppurativa of glands of Moll. Arch Opthalmol 1967;77:635-6.
[Google Scholar]
|
| 8. |
Moul DK, Korman NJ. The cutting edge. Severe hidradenitis suppurativa treated with adalimumab. Arch Dermatol 2006;142:1110-2.
[Google Scholar]
|
| 9. |
Khambhati R, Singhal P, Marfatia YS. Hidradenitis suppurativa in AIDS. Indian J Sex Transm Dis 2010;31:45-6.
[Google Scholar]
|
| 10. |
Yu CC, Cook MG. Hidradenitis suppurativa: A disease of follicular epithelium, rather than apocrine glands. Br J Dermatol 1990;122:763-9.
[Google Scholar]
|
Fulltext Views
7,003
PDF downloads
3,735





