Translate this page into:
Hidradenitis suppurativa treated with carbon dioxide laser followed by split skin thickness graft
2 Department of Plastic Surgery, PSG IMSR, Coimbatore, Tamil Nadu, India
3 Department of General Surgery, PSG IMSR, Coimbatore, Tamil Nadu, India
Correspondence Address:
Karthika Natarajan
Department of Dermatology, PSG IMSR, Coimbatore - 641 004, Tamil Nadu
India
| How to cite this article: Natarajan K, Srinivas C R, Thomas M, Aruchamy M, Kumar S R. Hidradenitis suppurativa treated with carbon dioxide laser followed by split skin thickness graft. Indian J Dermatol Venereol Leprol 2014;80:376-378 |
Sir,
A 34-year-old woman presented with multiple, infected nodules with interconnecting sinuses over the axillae, groin and perianal areas of 6 months duration. The lesions first developed over the left axilla [Figure - 1] and gradually spread to the right axilla followed by groin and perianal areas. They were accompanied by pain and purulent discharge. The patient also complained of difficulty in walking and lifting her hands.
 |
| Figure 1: Pre-operative image showing nodules, pustules and sinus tracts |
On examination, multiple discharging sinuses with surrounding induration were present in the axilla, groin and perianal areas. Complete blood picture revealed low hemoglobin (8 g/dl) and raised erythrocyte sedimentation rate. Peripheral smear was suggestive of normocytic, normochromic anemia with relative neutrophilia. Human immunodeficiency virus and hepatitis B surface antigen assays were negative. An ultrasound examination was done as marsupialization of the sinus tracts was being considered as a possible treatment modality. It showed ill-defined hypoechoic lesions in bilateral axillae, groin, perineal region and mons pubis in the subcutaneous soft tissue planes.
Histopathological examination of a punch biopsy specimen from the left axilla revealed a mixed dermal inflammatory infiltrate of neutrophils, lymphocytes and plasma cells. A sinus tract lined with granulation tissue was noted along with a perifollicular mixed inflammatory infiltrate. Dilated infundibulum filled with keratin and periadnexal inflammation was observed. These findings were consistent with hidradenitis suppurativa.
Pus culture showed a heavy growth of Streptococcus pyogenes. The patient did not respond to multiple courses of oral antibiotics including amoxicillin-clavulanic acid, clindamycin, cefixime and cotrimoxazole. A course of isotretinoin 20-30 mg daily was given for a period of 12 weeks with only slight improvement. Since the patient did not show a significant response to medical management, surgical intervention was planned. A wide excision of the diseased area over the left axilla was performed under general anesthesia using a carbon dioxide laser [Figure - 2] and [Figure - 3]. Laser ablation was performed in the continuous mode and the energy used varied from 10 to 15 W. Blood vessels were coagulated using the defocused mode. However, as the carbon dioxide laser was not effective in achieving complete hemostasis, diathermy was used to achieve control of bleeding [Figure - 4]. Since, the patient was anemic with a pre-operative hemoglobin of 9.6 g/dl, 1 unit of whole blood was transfused in the post-operative period. A split skin thickness graft was performed 10 days following the excision to ensure formation of adequate granulation tissue and successful graft uptake. The patient was treated with hematinics, antibiotics and regular dressing change. One year after surgery, the patient presented with persistent lesions over the right axilla, groin and perianal area but the grafted area in the left axilla was quiescent and showed no new lesions [Figure - 5].
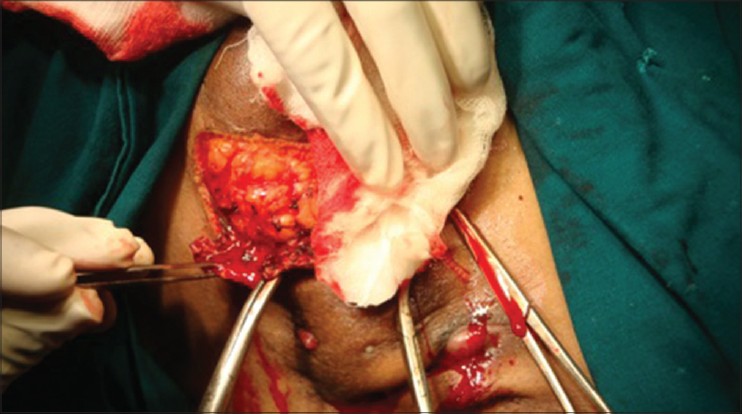 |
| Figure 2: Excision of diseased tissue using carbon dioxide laser |
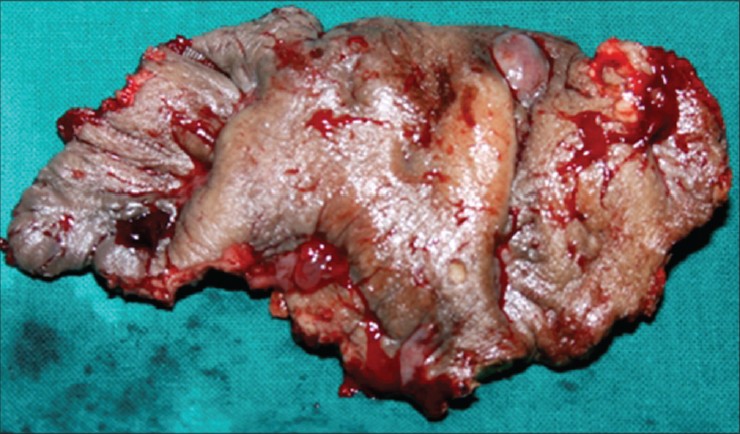 |
| Figure 3: Excised tissue |
 |
| Figure 4: Immediate post-operative appearance of left axilla |
 |
| Figure 5: Left axilla, 12 months following surgery and grafting |
Numerous therapeutic modalities include antibiotics, systemic or intralesional steroids, oral retinoids, cyclosporine, colchicine and dapsone have been used in the treatment of hidradenitis suppurativa. [1]
Surgical removal has been recommended for persistent lesions. Surgical options include radical excision with use of grafts or flaps and exteriorization and deroofing of sinus tracts. Surgical excision using the carbon dioxide laser (10,600 nm) and healing by secondary intention is associated with good results and minimal complications. [2] The advantages of this method are prevention of recurrences, achievement of adequate hemostasis and avoidance of multiple treatment sessions.
No post-operative complications such as scar contracture, graft failure or relapse of disease were encountered. With regard to hemostasis, high flow vessels greater than 500 μm are likely to bleed after carbon dioxide laser whereas without blood flow, vessels up to 2 mm have been coagulated. [3] An additional advantage of using carbon dioxide laser in defocused mode may be the destruction of residual lesions by the heat generated during the procedure.
| 1. |
Hazen PG, Hazen BP. Hidradenitis suppurativa: Successful treatment using carbon dioxide laser excision and marsupialization. Dermatol Surg 2010;36:208-13.
[Google Scholar]
|
| 2. |
Madan V, Hindle E, Hussain W, August PJ. Outcomes of treatment of nine cases of recalcitrant severe hidradenitis suppurativa with carbon dioxide laser. Br J Dermatol 2008;159:1309-14.
[Google Scholar]
|
| 3. |
Kauvar AN, George JH. Principles and Practices in Cutaneous Laser Surgery. Boca Raton: Taylor and Francis; 2005.
[Google Scholar]
|
Fulltext Views
5,596
PDF downloads
1,820





