Translate this page into:
Histiocytoid sweet syndrome related to bortezomib: A mimicker of cutaneous infiltration by myeloma
2 Department of Pathology, Hospital Universitario De La Princesa, Madrid, Spain
Correspondence Address:
Mar Llamas-Velasco
C/Diego de León 62, CP28006, Madrid
Spain
| How to cite this article: Llamas-Velasco M, Concha-Garz�n MJ, Fraga J, Arag��s M. Histiocytoid sweet syndrome related to bortezomib: A mimicker of cutaneous infiltration by myeloma. Indian J Dermatol Venereol Leprol 2015;81:305-306 |
Sir,
Histiocytoid Sweet syndrome presents with lesions mimicking classical Sweet syndrome but histopathologically is characterized by an inflammatory infiltrate composed of monocytoid or histiocytoid cells positively stained with CD15, CD43, CD45, CD68, MAC-386, HAM56, myeloperoxidase, and lysozyme, which correspond with immature neutrophils. [1] This pattern is independent of the length of time the lesion has been present and can be demonstrated in lesions of less than 24 h duration. [1]
Several skin lesions associated with bortezomib have been described as skin rash which show histopathological findings of lymphocytic infiltrates, interphase dermatitis, [2] vasculitis, [3] and different neutrophilic diseases. [4],[5],[6],[7],[8],[9],[10],[11]
A 66-year-old male with an IgG lambda myeloma that progressed despite autologous peripheral blood stem cell transplantation was being treated with bortezomib (1.3 mg/m 2 ) and melphalan (9 mg/m 2 ) according to VISTA protocol (Velcade as Initial Standard Therapy in Multiple Myeloma). On the 8 th day of the second chemotherapy cycle, he presented with asymptomatic lesions on the trunk that had appeared 5 days earlier on his chest and remained stable. No fever, malaise, or systemic symptoms were present. On physical examination, he had 15-20 well-demarcated erythematous, slightly infiltrated, edematous plaques [Figure - 1]. Blood analysis showed neutropenia (2860/mm 3 with 39.2% neutrophils). Erythrocyte sedimentation rate was 54 mm.
 |
| Figure 1: (a) Nonconfluent, erythematous, and edematous well-demarcated plaques, slightly infiltrated and without epidermal involvement. (b) Closer view of the lesions |
Skin biopsy revealed a perivascular, polymorphous, inflammatory infiltrate composed of lymphocytes and histiocyte-like cells [Figure - 2]. Histiocyte-like cells were positive for myeloperoxidase and lysozyme. Karyorrhexis was observed although vasculitis was not seen. Skin biopsy culture was negative. He did not receive treatment with granulocyte-macrophage-colony stimulating factor or other drugs known to be associated with Sweet′s syndrome. We made a diagnosis of histiocytoid Sweet′s syndrome related to bortezomib.
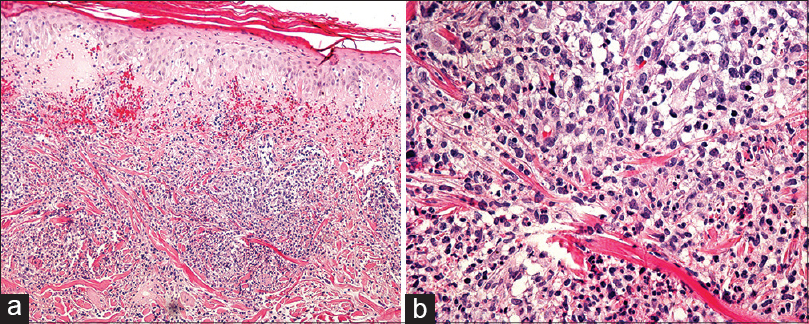 |
| Figure 2: (a) Edema in papillary dermis. Polymorphous nodular infiltrates in reticular dermis and extravasation of erythrocytes (H and E, ×100). (b) Lymphocytes without atypical nuclei, scattered mature neutrophils and many histiocyte-like cells (H and E, ×200) |
With intramuscular corticosteroid injection, the lesions disappeared but reappeared on the second day of the second part of the cycle. After this recurrence, he was treated with 20 mg prednisone for 4 days after every bortezomib treatment and did not develop any further recurrences.
Sweet′s syndrome related to multiple myeloma is infrequent, [9] but bortezomib-related neutrophilic diseases have been previously described with typical lesions that usually appear between the first and the third cycle. [4],[5],[6],[7],[8],[9],[10],[11] The presence of leucocytosis or fever may favor the diagnosis of myeloma associated-Sweet′s syndrome, but both findings were not present in our case unlike some other cases. [11] We were able to find only 2 previous cases of histiocytoid Sweet′s syndrome related to bortezomib. [4],[12] The main differential diagnoses of histiocytoid Sweet′s syndrome include interstitial granuloma annulare and interstitial granulomatous dermatitis, both showing a denser, "bottom-heavy," inflammatory infiltrate of histiocytes with large, pleomorphic nuclei that in some small foci are arranged in palisades surrounding degenerated basophilic collagen; [1] methotrexate-induced rheumatoid papules, which appears only in methotrexate-treated patients; and leukemia cutis that shows nodular dermal infiltrates of medium-sized, round to oval mononuclear cells that express lysozyme, myeloperoxidase, CD43, CD45, and CD68. Specific myeloma infiltration should be ruled out when evaluating presumed lesions of histiocytoid Sweet′s syndrome. A cytologic examination of peripheral blood should be performed and fluorescence in situ hybridization may be useful to detect underlying cytogenetic abnormalities in histiocytoid Sweet′s syndrome when there is an identifiable chromosomal abnormality. [13]
| 1. |
Requena L, Kutzner H, Palmedo G, Pascual M, Fernandez-Herrera J, Fraga J, et al. Histiocytoid Sweet syndrome: A dermal infiltration of immature neutrophilic granulocytes. Arch Dermatol 2005;141:834-42.
[Google Scholar]
|
| 2. |
Garcia-Navarro X, Puig L, Fernandez-Figueras MT, Dalmau J, Roe E, Alomar A. Bortezomib-associated cutaneous vasculitis. Br J Dermatol 2007;157:799-801.
[Google Scholar]
|
| 3. |
Agterof MJ, Biesma DH. Images in clinical Medicine. Bortezomib-induced skin lesions. N Engl J Med 2005;352:2534.
[Google Scholar]
|
| 4. |
Murase JE, Wu JJ, Theate I, Cole GW, Barr RJ, Dyson SW. Bortezomib-induced histiocytoid Sweet syndrome. J Am Acad Dermatol 2009;60:496-7.
[Google Scholar]
|
| 5. |
Van Regenmortel N, Van de Voorde K, De Raeve H, Rombouts S, Van de Velde A, Lambert J, et al. Bortezomib-induced Sweet's syndrome. Haematologica 2005;90:43.
[Google Scholar]
|
| 6. |
Liu CI, Hsiao CH, Wu JT, Tsai TF. Sweet syndrome with histiocytoid infiltrate and neutropenia: A rare combination. J Am Acad Dermatol 2009;61:882-4.
[Google Scholar]
|
| 7. |
Knoops L, Jacquemain A, Tennstedt D, Theate I, Ferrant A, Van den Neste E. Bortezomib-induced Sweet syndrome. Br J Haematol 2005;131:142.
[Google Scholar]
|
| 8. |
Paiva CM, Kurtis B, Mekki M, Newman MA, Singhal S, Lacouture ME. Neutrophilic dermatitis associated with bortezomib in a patient with multiple myeloma. Ann Oncol 2007;18:1744-5.
[Google Scholar]
|
| 9. |
Tanguy-Schmidt A, Avenel-Audran M, Croue A, Lissandre S, Dib M, Zidane-Marinnes M, et al. Bortezomib-induced acute neutrophilic dermatosis. Ann Dermatol Venereol 2009;136:443-6.
[Google Scholar]
|
| 10. |
Thomas M, Cavelier Balloy B, Andreoli A, Briere J, Petit A. Bortezomib-induced neutrophilic dermatosis with CD30+lymphocytic infiltration. Ann Dermatol Venereol 2009;136:438-42.
[Google Scholar]
|
| 11. |
Thuillier D, Lenglet A, Chaby G, Royer R, Vaida I, Viseux V, et al. Bortezomib-induced eruption: Sweet syndrome? Two case reports. Ann Dermatol Venereol 2009;136:427-30.
[Google Scholar]
|
| 12. |
Kim JS, Roh HS, Lee JW, Lee MW, Yu HJ. Distinct variant of Sweet's syndrome: Bortezomib-induced histiocytoid Sweet's syndrome in a patient with multiple myeloma. Int J Dermatol 2012;51:1491-3.
[Google Scholar]
|
| 13. |
Chavan RN, Cappel MA, Ketterling RP, Wada DA, Rochet NM, Knudson R, et al. Histiocytoid Sweet syndrome may indicate leukemia cutis: A novel application of fluorescence in situ hybridization. J Am Acad Dermatol 2014;70:1021-7.
[Google Scholar]
|
Fulltext Views
3,969
PDF downloads
1,612





