Translate this page into:
Histopathological comparison of lesional and perilesional skin in melasma: A cross-sectional analysis
2 Consultant Dermatologist and Epidemiologist, Mumbai, Maharashtra, India
Correspondence Address:
Manjyot Gautam
Department of Dermatology, Dr. D Y Patil Medical College, Navi Mumbai, Maharashtra
India
| How to cite this article: Gautam M, Patil S, Nadkarni N, Sandhu M, Godse K, Setia M. Histopathological comparison of lesional and perilesional skin in melasma: A cross-sectional analysis. Indian J Dermatol Venereol Leprol 2019;85:367-373 |
Abstract
Background: Melasma is a common acquired hyperpigmentary disorder of the sun exposed skin, especially the face. The pathogenesis is unclear but interplay between genetic factors, hormones and ultraviolet radiation is important. We have evaluated the histological characteristics of melasma and compared the findings with adjacent normal skin.
Methods: Skin biopsies were taken from both melasma and the surrounding perilesional normal skin in 50 Indian women. The sections were stained with hematoxylin and eosin, Fontana–Masson and Verhoeff–Van Gieson stains.
Results: Biopsy from melasma showed significant epidermal atrophy, basal cell hyperpigmentation and solar elastosis when compared with the perilesional skin. We found that the proportion of pendulous melanocytes was significantly higher in the lesional biopsy compared with the perilesional biopsy (76% vs 42%, P < 0.001). Similarly, pigmentary incontinence and features of solar elastosis were significantly higher in the lesional skin compared with the perilesional skin.
Conclusion: The characteristic histopathological features such as epidermal atrophy, basal cell hyperpigmentation and solar elastosis suggest the role of chronic sun exposure in the pathogenesis of melasma. Presence of pendulous melanocytes is a characteristic feature of melasma. The presence of pendulous melanocytes may have prognostic implications in melasma.
Introduction
Melasma is a common acquired hyperpigmentary disorder affecting the sun exposed areas of the face of young and middle-aged women with Fitzpatrick skin types III, IV and V.[1] It is common in Asians and Hispanics,[2] and has a significant impact on the quality of life of the affected individuals.[3] Genetic background, female hormones, ultraviolet radiation, pregnancy, cosmetics and certain drugs, including oral contraceptive pills and antiepileptic agents, are some of the predisposing factors for melasma.[1],[4],[5],[6] However, the exact pathogenesis of melasma is still notclear. The histopathology changes seen in melasma may provide the discerning dermatologist valuable pointers towards understanding its pathogenesis. There is paucity of literature on this subject.
Hence, we conducted the present study to evaluate the histological characteristics of melasma in the Indian population. Further, we also assessed the frequency of pendulous melanocytes on histopathological examination of melasma in Indian population. We compared the findings between lesional and perilesional skin in these individuals.
Methods
The present study is a cross-sectional analysis involving 50 individuals with melasma from January 2014 to August 2015.
Study site and population
The study was conducted in the Department of Dermatology of a tertiary care center and teaching hospital. The hospital caters to patients from all sections of the society; however, a large proportion of them belong to middle and lower-middle class. All female patients with a history of melasma were eligible for the study. A total of 50 consecutive consenting women were included in the study. The inclusion criteria were females; age ≥18 years; history of melasma for at least one year; and treatment naïve individuals (specifically taken for melasma lesions). We excluded pregnant and lactating women from the present study.
Data collection
After obtaining a written informed consent, we collected the following information: demographic data; history about the condition (duration of the disease, treatment taken – to ensure eligibility of individuals); history of sun exposure and products for prevention of sun exposure; use of oral contraceptive pills; history of any chronic or systemic illness and treatment taken for the same; history of any other procedures. Following this, we recorded findings from the systemic examination as well as local cutaneous examination. We recorded the site and features of melasma. We also calculated the Melasma Area Severity Index for each individual. A single dermatologist confirmed the clinical diagnosis of melasma and only facial melasma was included in the study. After the initial clinical examination, we used Wood's lamp examination to classify the facial melasma lesions.[7] If there was accentuation of pigmentation, we classified melasma as epidermal; if there was no accentuation, we classified it as dermal; if there was accentuation in some areas and no accentuation in other areas, we classified it as mixed.[7] Though in some individuals with very dark skin, melasma can be classified as indeterminate, we could not classify our cases as indeterminate. A single dermatologist classified the melasma based on Wood's lamp examination. However, if required (whenever there was doubt in the classification), we sought the opinion of a senior dermatologist. We used 2-mm punches for the biopsy. One biopsy was done at the site of melasma (lesional biopsy) and one in the adjacent skin without any lesion (perilesional biopsy). The perilesional biopsy was done at a distance of 0.5 cm from the edge of the lesion. Both these biopsies were divided into three sections. The sections were stained as follows: Hematoxylin and eosin stain; Fontana–Masson stain (for highlighting melanocytes); and Verhoeff–Van Geison stain (for elastic fibers). Some of the features we noted in all the biopsies studied were presence of pendulous melanocytes; pigment in basal layer and pigmentary incontinence; epidermal atrophy; basal cell degeneration; vascular changes and solar elastosis. These features were recorded in the lesional and perilesional biopsy.
Statistical analysis
We estimated the means and standard deviations (SD), or medians and interquartile ranges (IQR) for linear variables. We calculated the proportions for categorical variables. The linear variables were compared using the t-test for parametric data and Mann–Whitney test for nonparametric data for two groups. We used analysis of variance test for parametric data and Kruskal–Wallis test for nonparametric data for more than two groups. The proportions were compared using the Chi-square test or Fisher's exact test for low expected cell counts. A P value of <0.05 was considered statistically significant. The study was approved by the Institutional Ethics Committee.
Results
We evaluated 50 female patients with melasma for the present study. The mean age of the patients was 36.9 years ranging from 24 to 50 years. Majority of the women (n = 39) were housewives. The duration of melasma ranged from 1 to 20 years. Twenty-nine patients (66%) had history of sun exposure during the peak hours of the day, and seven patients had history of using cosmetics. Thirty patients (60%) gave a history of using sun protection measures. Only four out of 50 patients had history of consuming oral contraceptive pills. The median Melasma Area Severity score was 9.2 (4.8–15). The most common pattern observed under Wood's lamp examination in our study was epidermal (n = 35, 70%) followed by dermal (n = 9, 18%) and mixed (n = 6, 6%).
Hematoxylin and eosin staining of the specimens showed epidermal atrophy in 90% of lesional skin [Figure - 1]a, [Figure - 1]b, [Figure - 1]c and only 28% of perilesional skin [Figure - 1]d, [Figure - 1]e, [Figure - 1]f and [Table - 1]. This difference was statistically significant (P < 0.001). Examination of the dermis showed moderate-to-severe solar elastosis in 88% of lesional skin and only 14% of perilesional skin, which was statistically significant (P < 0.001). Fontana–Masson stain was done for better visualization of pigmentary changes [Figure - 1]b and [Figure - 1]e. Approximately 60% of the patients showed moderate-to-severe degree of hyperpigmentation in the basal layer in the lesional skin while the corresponding figure in the perilesional skin was only 22%, which was statistically significant (P < 0.001). Pendulous melanocytes were noted in the lesional skin of 76% of the patients compared to only 42% in the perilesional skin, which was statistically significant (P < 0.001). Pigmentary incontinence and dermal melanophages were noted in 80% of lesional skin and 48% of perilesional skin (P = 0.001). Pendulous melanocytes were seen in 76% of the lesional sites but only 42% of the perilesional sites. This result was also statistically significant (P < 0.001). We used Verhoeff–Van Geison stain for elastic fibers [Figure - 1]c and [Figure - 1]f. The amount of elastotic material was significantly higher in melasma skin (98%) compared to perilesional normal skin (8%) (P < 0.001). Though we did not find any basal layer degeneration in the lesional or perilesional skin, we did observe increased vascularity in the lesional skin compared with perilesional skin (30% vs. 0%; P < 0.001). Approximately 10% of the patients also had extravasation?? in the lesional biopsy.
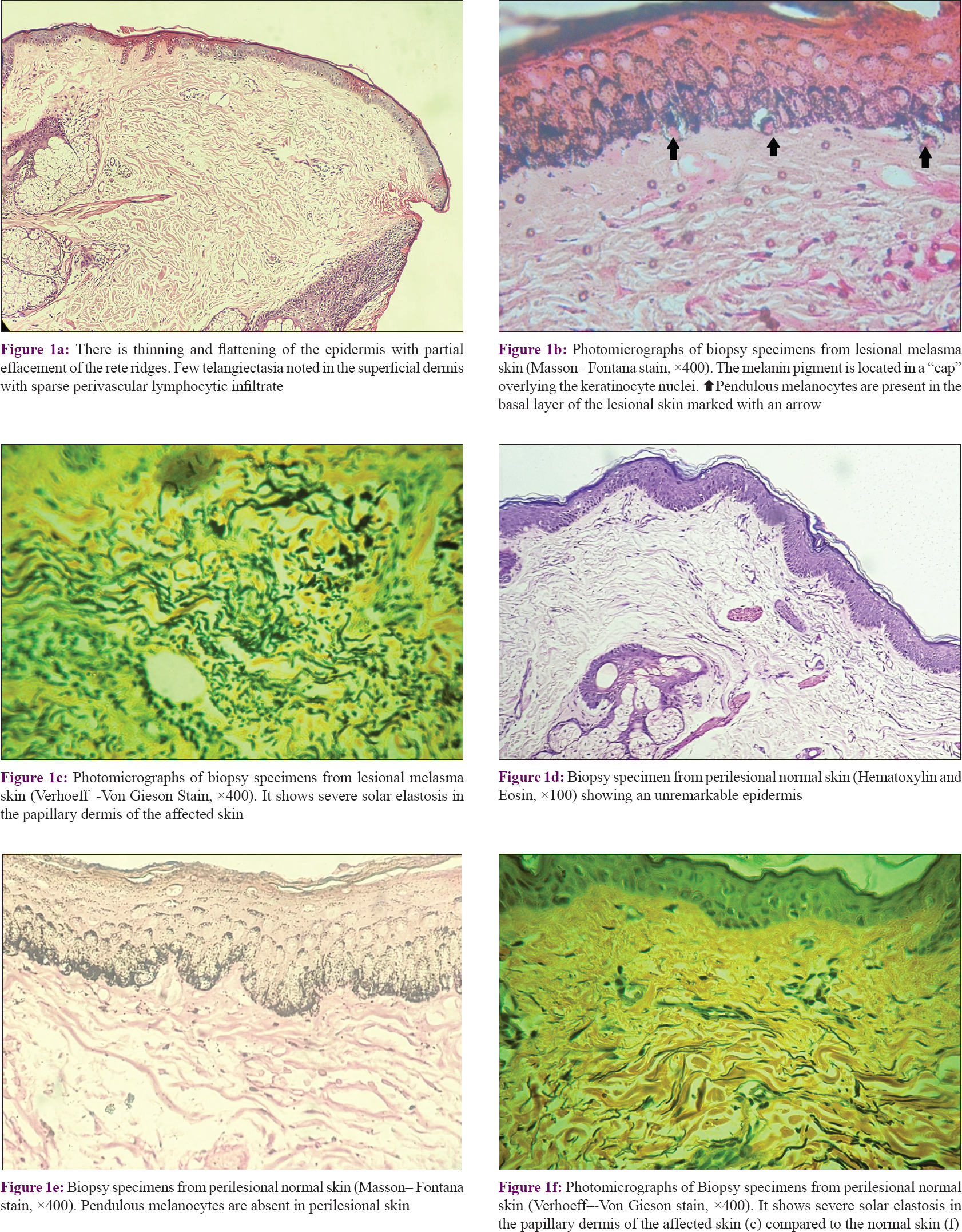 |
| Figure 1: |

We compared sun exposure and melasma features in these individuals. The mean (standard deviation) Melasma Area Severity Index scores for sun exposure of less than 2 h, 2–5 h and more than 5 h was 12.2 (6.1), 10.7 (6.8) and 8.0 (4.4), respectively; this difference was not statistically significant (P = 0.32). Most individuals with dermal melasma reported sun exposure for less than 2 h (63%), whereas most individuals with epidermal melasma reported exposure for 2–5 h, whereas all individuals with mixed melasma reported sun exposure more than 2 h. In the hematoxylin and eosin-stained lesion, the median number (interquartile range) of pendulous melanocytes in lesional skin was the highest in those exposed to sun for more than 5 h [13 (10, 16)], followed by those exposed for 2–5 h [11 (3, 16)] and the least in those exposed for less than 2 h [7 (3, 15)]; P = 0.34. Severe pigment in the basal layer in lesional skin was highest in those exposed for more than 5 h (13%) compared with 2–5 h (4%) or less than 2 h (0%); P = 0.59.
We also classified the patients according to the type of melasma as epidermal, dermal or mixed variants and analyzed the histopathologic findings separately [Table - 2] and [Table - 3]. All the nine patients (100%) with dermal melasma showed pigmentary incontinence and dermal melanophages in the lesional skin compared to 80% of patients with epidermal melasma and 83% of patients with mixed melasma. Six patients (67%) with dermal melasma showed pigmentary incontinence and dermal melanophages in peri-lesional skin as against 60% of patients with epidermal melasma and 17% of patients with mixed melasma. Patients with epidermal melasma showed more solar elastosis than patients with dermal or mixed melasma. However these differences were not statistically significant.


We did not find any significant associations between Melasma Area Severity Index score and histopathological features. There were no significant differences in the Melasma Area Severity Index score in individuals who had pigmentary incontinence compared with those who did not show any features of incontinence [Mean (standard deviation): 10.4 (6.5) vs 11.2 (6.1); P = 0.73]. Similarly, the correlation between the number of melanocytes and Melasma Area Severity Index score was not statistically significant (r = 0.22, P = 0.13). There were no significant differences in the Melasma Area Severity Index score between individuals who had a higher grade of pigment in the basal layer (2+/3+) compared with a lower grade (1+) [Mean (standard deviation): 10.9 (6.7) vs 10.2 (6.3); P = 0.67].
Discussion
Melasma is a chronic, acquired hypermelanosis commonly affecting the sun exposed areas of the face and sometimes the neck, and is characterized by irregular gray-brown macules and patches. It is more common in females than males. The exact pathogenesis of melasma is unclear. We believe that a better understanding of the histopathology of melasma will be of great help in improving our understanding of the disease process and its pathogenesis. There are very few studies in the literature evaluating the histopathological features of melasma. Our study compares the histopathologic characteristics of melasma with the adjacent normal facial skin.
The mean age of our patients was 36.9 years (standard deviation, 7.5), while Achar and Raithi reported the mean age of 33.4 years and Goh reported the mean age of 42.3 years in their patients.[8],[9]
The mean duration of melasma was 3 years in our study compared to 3.5 years in the study conducted by Achar and Rathi.[8] Sixty-six percent of our patients gave a history of sun exposure during the peak hours of the day, which was quite high in comparison to other studies (28% reported by Kavya[10] and 55.2% reported by Achar and Rathi).[8] Approximately 15% of our patients used cosmetics regularly compared to 22% reported by Kavya.[10] Only 8% of our patients had a history of consuming oral contraceptive pills while Kavya reported 11.11% of the patients who consumed these pills.[10] The most common pattern under Wood's lamp examination observed in our study was epidermal (70%), which was in accordance to the study by Kavya (55%).[10] However, this was in contrast to the study by Achar and Rathi where the dermal variant was the most common.[8]
On histopathological examination of hematoxylin and eosin-stained sections, epidermal atrophy was noted in the lesional melasma skin of 90% of the cases. In contrast, only 28% of the cases demonstrated epidermal atrophy within the peri-lesional skin. Vermani et al. reported these changes in 28% of their patients in the affected skin.[11] Kang et al., however, reported epidermal atrophy in both lesional and perilesional skin.[12] This epidermal atrophy in melasma is attributed to chronic solar damage.[12],[13]
Solar elastosis was significantly increased in the lesional skin (88%) compared to the perilesional skin (14%) (P < 0.001). These findings were in accordance to those reported by Kang et al. and Torres-Álvarez et al.[12],[14] The latter study reported that melasma skin showed a significantly higher degree of solar elastosis (83%) than perilesional normal skin (29%).[14] Furthermore, on verhoeff-van geison (VVG)-stained sections, the amount of elastotic material was significantly higher in melasma skin (98%) than that in normal skin (8%) (P < 0.001). This was similar to the findings reported by Kang et al.[12] and Hernández-Barrera et al.[15] Increased solar elastosis in the lesional skin suggests the role of chronic sun exposure in the development of melasma. Ultraviolet radiation of keratinocytes results in the production of cytokines such as α-melanocyte-stimulating hormone and adrenocorticotropic hormone derived from proopimelanocortin which stimulate melanocyte activity and proliferation.[16],[17] Persistent overexpression of α-melanocyte-stimulating hormone has been reported by Im et al.[18] Moreover, solar elastosis in the dermis induces secretion of stem cell factor by fibroblasts which stimulate melanogenesis in the overlying epidermis.[16],[19],[20] It is difficult to study melanocytes on routine hematoxylin and eosin staining. Fontana–Masson staining gives more definite identification of melanin.[12] Sixty percent of our patients showed moderate-to-severe increase in pigmentation in the basal layer of lesional skin while the corresponding figure in perilesional skin was only 22%. Kang et al.[12] reported an increase in the pigmentation in all the layers of the epidermis in lesional skin, whereas in the normal skin, the melanin pigment was mostly confined to the basal layer. This difference in melanin pigment in the lesional versus the perilesional skin suggests an increased activity of melanocytes in the lesional skin compared to the perilesional skin.
Pigment incontinence and dermal melanophages were noted in 80% of lesional skin compared to 48% of perilesional skin. Kang et al. reported these findings in 36% of their patients in both lesional and perilesional skin.[12] Though previous studies have also highlighted differences in dermal melanin in lesion and perilesional skin, Kang has suggested that more studies are needed to study the association between the presence of dermal melanin and outcome.[12],[21],[22] Recently, the concept of pendulous melanocytes has evolved in melasma. These melanocytes show features of protruding into the dermis. Kang et al. have demonstrated that these cells correspond to activated dendritic melanocytes in in-vivo confocal microscopy examination. They also suggested that pendulous melanocytes occur in epidermal hypermelanosis related to the hyperactivity of melanocytes.[23]
In our study, pendulous melanocytes were detected in 76% of lesional sites but only 42% of perilesional sites. Lee et al. observed pendulous melanocytes in 45% of lesional skin and 9% of perilesional skin.[24] These findings suggest that pendulous melanocytes are a characteristic feature of melasma. Lee et al. postulated the mechanism of pendulous cells in melasma. Chronic sun exposure may increase matrix metalloproteinase 2 expression which loosens the basement membrane in melasma, which is then responsible for the pendulous change of melanocytes in melasma.[24] The clinical significance of pendulous melanocytes is unclear at present. They may be of prognostic importance where presence of these cells in the affected melasma skin may increase the risk of developing postinflammatory hyperpigmentation following invasive procedures such as lasers. Thus, potentially, a biopsy may be useful to decide treatment protocols in these patients. Our study was not without limitations. We did not perform dermoscopy and immunostaining due to lack of facilities. Furthermore, as the individual examining the slides was not blinded, it is likely that presence of certain features may be over-reported in the lesional skin compared with perilesional skin. We tried to address this by using multiple sections with special stains, nonetheless, this may be a potential limitation of the study.
Melasma is a medical mystery as far as the etiology is concerned. Not many studies have been done to elucidate the histopathology. Our own study showed diverse histopathological findings such as epidermal atrophy, basal cell hyperpigmentation and solar elastosis when compared to findings in normal (perilesional) skin. However, the most significant finding in our study is the prominence of pendulous melanocytes in 76% lesional skin compared to only 42% in normal skin, a highly significant difference. We feel further investigations into the morphological abnormalities of melanocytes are required. This will probably help us to unravel the “enigma wrapped in a mystery” that is melasma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that names and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study was financially supported by the IADVL-L' Oreal Hair and Skin Research India Grant - 2014.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Handel AC, Miot LD, Miot HA. Melasma: A clinical and epidemiological review. An Bras Dermatol 2014;89:771-82.
[Google Scholar]
|
| 2. |
Sheth VM, Pandya AG. Melasma: A comprehensive update: Part I. J Am Acad Dermatol 2011;65:689-97.
[Google Scholar]
|
| 3. |
Freitag FM, Cestari TF, Leopoldo LR, Paludo P, Boza JC. Effect of melasma on quality of life in a sample of women living in Southern Brazil. J Eur Acad Dermatol Venereol 2008;22:655-62.
[Google Scholar]
|
| 4. |
Grimes PE. Melasma. Etiologic and therapeutic considerations. Arch Dermatol 1995;131:1453-7.
[Google Scholar]
|
| 5. |
Ortonne JP, Arellano I, Berneburg M, Cestari T, Chan H, Grimes P, et al. Aglobal survey of the role of ultraviolet radiation and hormonal influences in the development of melasma. J Eur Acad Dermatol Venereol 2009;23:1254-62.
[Google Scholar]
|
| 6. |
Sanchez NP, Pathak MA, Sato S, Fitzpatrick TB, Sanchez JL, Mihm MC Jr., et al. Melasma: A clinical, light microscopic, ultrastructural, and immunofluorescence study. J Am Acad Dermatol 1981;4:698-710.
[Google Scholar]
|
| 7. |
Bandyopadhyay D. Topical treatment of melasma. Indian J Dermatol 2009;54:303-9.
[Google Scholar]
|
| 8. |
Achar A, Rathi SK. Melasma: A clinico-epidemiological study of 312 cases. Indian J Dermatol 2011;56:380-2.
[Google Scholar]
|
| 9. |
Goh CL, Dlova CN. A retrospective study on the clinical presentation and treatment outcome of melasma in a tertiary dermatological referral centre in Singapore. Singapore Med J 1999;40:455-8.
[Google Scholar]
|
| 10. |
Kavya M. Melasma: A clinico-epidemioological study. Int J Basic Appl Med Sci 2014;4:388-91.
[Google Scholar]
|
| 11. |
Sarvjot V, Sharma S, Mishra S, Singh A. Melasma: A clinicopathological study of 43 cases. Indian J Pathol Microbiol 2009;52:357-9.
[Google Scholar]
|
| 12. |
Kang WH, Yoon KH, Lee ES, Kim J, Lee KB, Yim H, et al. Melasma: Histopathological characteristics in 56 Korean patients. Br J Dermatol 2002;146:228-37.
[Google Scholar]
|
| 13. |
Toyoda M, Morohashi M. Morphological alterations of epidermal melanocytes in photoageing: An ultrastructural and cytomorphometric study. Br J Dermatol 1998;139:444-52.
[Google Scholar]
|
| 14. |
Torres-Álvarez B, Mesa-Garza IG, Castanedo-Cázares JP, Fuentes-Ahumada C, Oros-Ovalle C, Navarrete-Solis J, et al. Histochemical and immunohistochemical study in melasma: Evidence of damage in the basal membrane. Am J Dermatopathol 2011;33:291-5.
[Google Scholar]
|
| 15. |
Hernández-Barrera R, Torres-Alvarez B, Castanedo-Cazares JP, Oros-Ovalle C, Moncada B. Solar elastosis and presence of mast cells as key features in the pathogenesis of melasma. Clin Exp Dermatol 2008;33:305-8.
[Google Scholar]
|
| 16. |
Kwon SH, Park KC. Clues to the pathogenesis of melasma from its histologic findings. J Pigment Disord 2014;1:141.
[Google Scholar]
|
| 17. |
Suzuki I, Kato T, Motokawa T, Tomita Y, Nakamura E, Katagiri T, et al. Increase of pro-opiomelanocortin mRNA prior to tyrosinase, tyrosinase-related protein 1, dopachrome tautomerase, pmel-17/gp100, and P-protein mRNA in human skin after ultraviolet B irradiation. J Invest Dermatol 2002;118:73-8.
[Google Scholar]
|
| 18. |
Im S, Kim J, On WY, Kang WH. Increased expression of alpha-melanocyte-stimulating hormone in the lesional skin of melasma. Br J Dermatol 2002;146:165-7.
[Google Scholar]
|
| 19. |
Imokawa G. Autocrine and paracrine regulation of melanocytes in human skin and in pigmentary disorders. Pigment Cell Res 2004;17:96-110.
[Google Scholar]
|
| 20. |
Kang HY, Hwang JS, Lee JY, Ahn JH, Kim JY, Lee ES, et al. The dermal stem cell factor and c-kit are overexpressed in melasma. Br J Dermatol 2006;154:1094-9.
[Google Scholar]
|
| 21. |
Grimes PE, Yamada N, Bhawan J. Light microscopic, immunohistochemical, and ultrastructural alterations in patients with melasma. Am J Dermatopathol 2005;27:96-101.
[Google Scholar]
|
| 22. |
Kang HY, Ortonne JP. What should be considered in treatment of melasma. Ann Dermatol 2010;22:373-8.
[Google Scholar]
|
| 23. |
Kang HY, Bahadoran P, Suzuki I, Zugaj D, Khemis A, Passeron T, et al. In vivo reflectance confocal microscopy detects pigmentary changes in melasma at a cellular level resolution. Exp Dermatol 2010;19:e228-33.
[Google Scholar]
|
| 24. |
Lee DJ, Park KC, Ortonne JP, Kang HY. Pendulous melanocytes: A characteristic feature of melasma and how it may occur. Br J Dermatol 2012;166:684-6.
[Google Scholar]
|
Fulltext Views
7,501
PDF downloads
3,037





