Translate this page into:
Ichthyosiform mycosis fungoides with alopecia and atypical membranous nephropathy
Correspondence Address:
Hao Cheng
Department of Dermatology, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, 3 Qingchun Road East, 310016 Hangzhou
China
| How to cite this article: Zhou Q, Zhu K, Yu H, Cheng H. Ichthyosiform mycosis fungoides with alopecia and atypical membranous nephropathy. Indian J Dermatol Venereol Leprol 2011;77:180-183 |
Abstract
We describe here a rare case of variant of mycosis fungoides (MF): ichthyosiform MF with alopecia and atypical membranous nephropathy. The diagnosis was made based on the following findings: generalized ichthyosis-like eruption, alopecia, enlarged superficial lymph nodes, proteinuria, and hematuria, the histological features of the skin biopsy from both ichthyotic and alopecic lesions with immunohistochemical staining, and the renal biopsy examination with immunofluorescence. The histological examination of ichthyotic and alopecic lesions displayed a predominant infiltration of atypical lymphocytes in the upper dermis with the characteristics of epidermotropism and folliculotropism. Immunohistochemical studies demonstrated that most infiltrated atypical lymphocytes were CD3, CD4, and CD45RO positive, whereas negative for CD5, CD7, CD20, CD30, and CD56. A renal biopsy examination revealed atypical membranous nephropathy with deposition of immunoglobulin G (IgG), IgM, IgA, C1q, and C3. In this case atypical membranous nephropathy was involved, which is very uncommon and has never been presented in the literature to date. Although ichthyosiform MF usually features a relatively favorable course, diffuse alopecia and the renal involvement in this case might indicate aggressive disease and poor prognosis.Introduction
Mycosis fungoides (MF) is an epidermotropic cutaneous T-cell lymphoma (CTCL) that can manifest with various clinical presentations including the typical patch, plaque and nodular lesions, and less common hypopigmented, bullous, hyperkeratotic, or ichthyosis-like lesions. Ichthyosiform MF is recognized recently as a clinical variant of MF with indolent course. We describe here a rare case of ichthyosiform MF in a 23-year-old man who developed a widespread ichthyosis-like appearance coexisting with diffuse alopecia, enlarged lymph nodes, hematuria, and proteinuria.
Case Report
The patient presented with a 1-year history of lumbar pain and frequency of micturition, in combination with recently observed microscopic hematuria and proteinuria. During his hospitalization in department of nephrology, the patient was referred to dermatologist for ill-defined ichthyosis-like skin lesion of 10 years duration. Slight itching and crusted excoriations were presented on his limbs and trunk. In addition, the patient has suffered from alopecia for about 5 years. The patient had no relevant medical or family history.
A physical examination revealed diffuse flush and ichthyosis-like lesions on whole body [Figure - 1]. Patchy alopecic scalp and sparse body hair including eyebrows, axillary, and pubic hair were also exhibited. Enlarged lymph nodes were palpable in the cervical, bilateral inguinal, and axillary regions. Differential blood count, liver function, renal function, and other biochemical analyses were normal. No atypical circulating cells were found. Bone marrow smear disclosed active proliferation of non-malignant cells. Computed tomography and B-ultrasound scan showed hepatosplenomegaly and multiple enlarged lymph nodes in porta hepatis, retroperitoneal, and bilateral axillary regions. A urinalysis discovered protein 2+ and occult blood 2+, and the 24-h urine protein quantification was 2 g. A renal biopsy demonstrated thickening of the glomerular basement membrane with slight mesangial expansion and proliferation. The immunofluorescence of a renal biopsy showed positive staining of IgG, IgM, IgA, C1q, and C3 along the glomerular basement membrane and mesangium, consistent with the diagnosis of atypical membranous nephropathy. Histopathological examination of a lymph node revealed a dermatopathic lymphadenitis.
 |
| Figure 1: (a-d) Ichthyosis-like scaly and dry lesions on whole body. Alopecia is also exhibited |
The biopsy specimen obtained from scaly trunk lesion disclosed focal parakeratosis, slight hyperkeratosis, acanthosis, and thinned granular layer of the epidermis. There was a band-like infiltrate of atypical cerebriform lymphocytes in the upper dermis. The infiltration was also presented around the hair follicles, sweat glands, and sebaceous glands [Figure - 2].
 |
| Figure 2: Skin biopsy specimens showing: (a) band-like infiltrate of atypical cerebriform lymphocytes in the upper dermis (H and E, ×40), (b) atypical lymphocytes exocytosis in the epidermis with formation of epidermal lymphocytic micro-abscesses (H and E, �400), (c-d) atypical lymphocytes infiltration surrounding and invading sweat glands and hair follicles (H and E, ×100) |
The specimen from alopecic scalp displayed similar picture but with significantly diminished hair follicles and infiltrated lymphocytes in damaged follicular structures. Immunohistochemical studies showed that the majority of atypical lymphocytes had positive staining for CD3, CD4, and CD45RO, weak positive for CD8, whereas negative for CD5, CD7, CD20, CD30, and CD56 [Figure - 3]. Some scattered monocytes had positive staining for CD68.
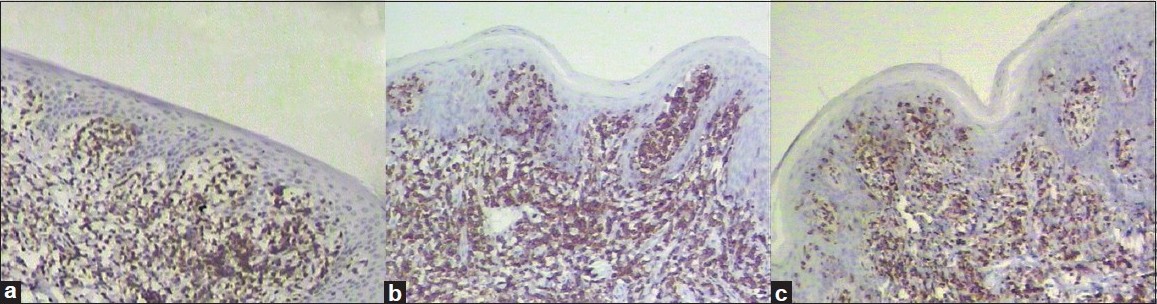 |
| Figure 3: Immunohistochemical studies demonstrate that the infiltrating atypical lymphocytes were positive for CD3 (a), CD4 (b), and CD45RO (c) (H and E, �100), whereas negative for CD5, CD7, CD20, CD30, and CD56 (picture not shown) |
Based on the clinical features and laboratory findings, the diagnosis of a stage IIA MF was established. The patient was treated with psoralen plus ultraviolet A (UVA), etretinate (30 mg/day) and prednisone (30 mg/day) for 5 months. Partial improvement of the ichthyosis-like lesion and alopecia was been noted. However, after the discontinuation of prednisone and etretinate, the ichthyosis-like lesion and alopecia worsened. The second biopsy specimen obtained from scaly trunk lesion displayed more severe infiltrate of atypical lymphocytes in the epidermis. A systemic chemotherapy regimen is now under discussion.
Discussion
When acquired ichthyoses are related to neoplasms, mostly lymphomas, they can behave as paraneoplastic syndrome or as certain clinical variant of the lymphoma. Ichthyosiform MF has recently been reported to be a variant of MF within its wide clinicopathological spectrum such as classical, follicular, syringotropic, palmoplantar, bullous/vesicular, hyper/hypopigmented, and granulomatous MF. [1],[2],[3] First described in 1996, there have been less than 20 cases of ichthyosiform MF. [1],[2],[4] Ichthyosiform MF was characterized as the feature of a favorable course and the tendency to be pathologically associated with folliculotropic MF. [1] Among 18 reported cases of CTCL presenting an ichthyosis-like eruption, 10 cases had a cutaneous manifestation including alopecia, comedo-like lesions, and follicular papules. [4] In our case, histological examination of the biopsy specimen from both ichthyotic and alopecic lesions displayed a predominant infiltration of atypical lymphocytes in the upper dermis with the features of epidermotropism and folliculotropism. More importantly, the specimen from alopecic scalp revealed significantly diminished hair follicles and damage of the follicular structures with infiltrated lymphocytes. Unfortunately, T-cell receptor gene rearrangement analysis, a test for early diagnosis of CTCL, was not done due to the limitation of our hospital lab. According to the characteristic clinical and histological manifestations, the diagnosis of ichthyosiform MF with alopecia can be made.
According to the ISCL/EORTC revision to the staging of MF, [5] a stage II MF was considered for our case. Corticosteroids, psoralen plus UVA, etretinate and radiotherapy are utilized to treat classic MF. [6],[7] However, ichthyosiform MF with alopecia may be more resistant to skin-directed therapies such as topical treatments and UVB. [8] This is probably because of the deeper location of infiltrating atypical lymphocytes in the follicles. Paradoxically, the above hypothesis could not explain why the treatment in our case with psoralen plus UVA, etretinate, and prednisone seemed to be unsuccessful.
Kidney involvement related to MF has rarely been described. [4],[9] It has been reported that CTCL is associated with glomerular disease, especially with IgA nephropathy [4],[10] and segmental glomerular sclerosis. [9] Among eight reported cases of CTCL associated with kidney disease, all except one were late-stage CTCL, and three patients died of progressive disease. [10] However, it is unclear whether this association is pathophysiological and the mechanism of renal disease in lymphoma is unknown. Cather et al,[9] speculated that interleukin-2 is involved in glomerular dysfunction. Additionally, Sato et al,[4] reported that a case of ichthyosiform MF with nephropathy demonstrated increased serum soluble interleukin-2 receptor.
Ryan et al,[7] recently reported a very young patient diagnosed as folliculotropic and ichthyosiform MF. However, our patient is to our knowledge the first case of ichthyosiform MF associated with diffuse alopecia and atypical membranous nephropathy. Though ichthyosiform MF usually features an indolent and favorable course, our case was characterized by widespread ichthyosis-like lesion with diffuse body hair loss and atypical membranous nephropathy which might be associated with aggressive disease and poor prognosis.
| 1. |
Marzano AV, Borghi A, Facchetti M, Alessi E. Ichthyosiform mycosis fungoides. Dermatology 2002;204:124-9.
[Google Scholar]
|
| 2. |
Bianchi L, Papoutsaki M, Orlandi A, Citarella L, Chimenti S. Ichthyosiform mycosis fungoides: A neoplastic acquired ichthyosis. Acta Derm Venereol 2007;87:82-3.
[Google Scholar]
|
| 3. |
Kazakov DV, Burg G, Kempf W. Clinicopathological spectrum of mycosis fungoides. J Eur Acad Dermatol Venereol 2004;18:397-415.
[Google Scholar]
|
| 4. |
Sato M, Sohara M, Kitamura Y, Hatamochi A, Yamazaki S. Ichthyosiform mycosis fungoides: Report of a case associated with IgA nephropathy. Dermatology 2005;210:324-8.
[Google Scholar]
|
| 5. |
Olsen E, Vonderheid E, Pimpinelli N, Willemze R, Kim Y, Knobler R, et al. Revisions to the staging and classification of mycosis fungoides and sezary syndrome: A proposal of the international society for cutaneous lymphomas (ISCL) and the cutaneous lymphoma task force of the european organization of research and treatment of cancer (EORTC). Blood 2007;110:1713-22.
[Google Scholar]
|
| 6. |
Keehn CA, Belongie IP, Shistik G, Fenske NA, Glass LF. The diagnosis, staging, and treatment options for mycosis fungoides. Cancer Control 2007;14:102-11.
[Google Scholar]
|
| 7. |
Ryan C, Whittaker S, D'Arcy C, O'Regan GM, Rogers S. Juvenile folliculotropic and ichthyosiform mycosis fungoides. Clin Exp Dermatol 2009;34:e160-2.
[Google Scholar]
|
| 8. |
Ramsay DL, Lish KM, Yalowitz CB, Soter NA. Ultraviolet-b phototherapy for early-stage cutaneous T-cell lymphoma. Arch Dermatol 1992;128:931-3.
[Google Scholar]
|
| 9. |
Cather JC, Jackow C, Yegge J, Hagemeister F, Duvic M. Mycosis fungoides with focal segmental glomerular sclerosis and nephrotic syndrome. J Am Acad Dermatol 1998;38:301-5.
[Google Scholar]
|
| 10. |
Moe SM, Baron JM, Coventry S, Dolan C, Umans JG. Glomerular disease and urinary sezary cells in cutaneous t-cell lymphomas. Am J Kidney Dis 1993;21:545-7.
[Google Scholar]
|
Fulltext Views
3,353
PDF downloads
2,242





