Translate this page into:
Ichthyosiform sarcoidosis revisited
2 Department of Dermatology, Venereology, and Leprosy, R. G. Kar Medical College, Khudiram Bose Sarani, Kolkata, West Bengal, India
Correspondence Address:
Sudip Kumar Ghosh
Department of Dermatology, Venereology, and Leprosy, R. G. Kar Medical College, 1, Khudiram Bose Sarani, Kolkata - 700 004, West Bengal
India
| How to cite this article: Ghosh UC, Ghosh SK, Hazra K, Mondal A. Ichthyosiform sarcoidosis revisited. Indian J Dermatol Venereol Leprol 2013;79:795-798 |
Abstract
Cutaneous manifestations of sarcoidosis are present in approximately one-third of the cases. Ichthyosiform lesion is one of the extremely rare cutaneous manifestations of sarcoidosis. It is a uncommon, but specific cutaneous manifestation of sarcoidosis that may precede or appear simultaneously with the diagnosis of systemic sarcoidosis. Approximately 20 cases of ichthyosiform sarcoidosis have been reported in the PubMed database. We report here a case of sarcoidosis with ichthyosiform skin lesions along with central nervous system (CNS) and pulmonary involvement for its rarity and interesting clinical presentation.Introduction
Sarcoidosis is a multisystem granulomatous disorder of an unknown etiology. [1] Cutaneous manifestations of sarcoidosis are present in approximately 25% to 35% of the cases. [2],[3] Since the early description of the disease, many reports have documented the protean clinical manifestations of the disorder. Ichthyosiform lesion is one of the extremely rare cutaneous manifestations of sarcoidosis. [3],[4] We report herein a case of ichthyosiform sarcoidosis for its rarity, unusual associations, and interesting clinical presentations.
Case Report
A 35-year-old Indian woman presented with a history of gradual onset of pain and swelling of both ankle joints and dryness and scaling of the skin of the lower limbs for the past 6 months. She was suffering from headache for the last one and half months. In addition, she had double vision, deviation of angle of mouth toward the right side, and loss of sensation of the left half of her face for the last 2 weeks. Her ankle pain was progressive in nature and persisted throughout the day. Other joints were not involved, and there was no early morning stiffness. There was no history of any preceding drug intake or any family history of ichthyosiform disorder. The headache was gradually progressive, persistent, throbbing in character, and associated with photophobia and nausea. Diplopia was more in the left lateral gaze. There was no loss of smell or taste sensations, hearing loss, tinnitus, difficulty in swallowing, altered sensorium, convulsion, fever, weight loss, or cough. There was no significant past history of medical illness. Her menstrual history, bladder and bowel functions, sleep, and appetite were normal.
Cutaneous examination showed xerosis with fine hyperpigmented, adherent, and rhomboidal scales on both legs [Figure - 1]. There was no lesional anesthesia nor any thickening of peripheral nerves. No other mucocutaneous lesion was noted elsewhere in the body. Hair and nails were normal. Systemic examination revealed sensory loss in the distribution of the left V th cranial nerve, left VI th cranial nerve palsy, and lower motor neuron type of palsy of the left VII th cranial nerve [Figure - 2]. Cranium and spine were normal, and there was no sign of meningeal irritation. Ankle joints were swollen and tender.
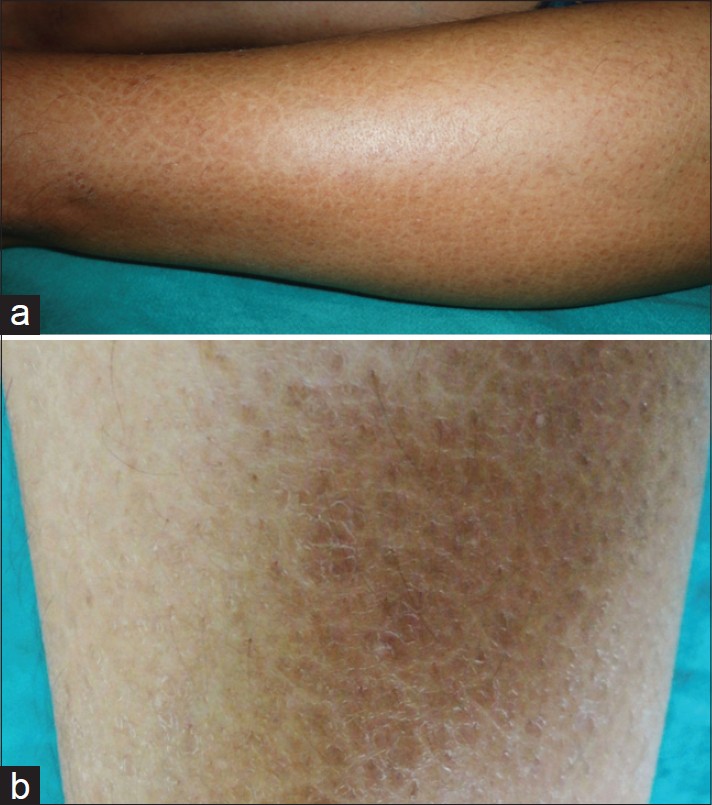 |
| Figure 1: (a) Ichthyosiform eruption on leg (b) Close-up showing fine hyperpigmented rhomboidal scales and xerosis |
 |
| Figure 2: Deviation of the angle of mouth toward the right side (due to left-sided facial palsy) and medial convergence of the left eye ball (due to left sixth cranial nerve palsy) |
There were no palpable lymph nodes and systemic examination was otherwise normal. Ophthalmological evaluation did not reveal any abnormality. Computed tomography (CT) scan of brain showed normal brain parenchyma. Magnetic resonance imaging (MRI) of brain revealed enhanced and thickened extra-axial tissue symmetrically distributed in the region of both cavernous sinuses [Figure - 3]. The right-sided lesion measured about 20 Χ 10 Χ 13 mm and that of the left side measured about 21 Χ 08 Χ 12 mm. Chest X-ray (CXR) showed upper mediastinal widening. CT scan of thorax showed enlarged and discrete mediastinal lymph nodes in the right para-tracheal and pre-tracheal regions along with a few small enlarged lymph nodes in the left para-tracheal region. Mild degree of reticulation due to thickening of intra-lobular septa was seen in the right middle lobe and also in the peripheral aspect of the left lower lobe. Some scattered streaky nodules were also noted in the middle lobe [Figure - 4]. Sputum for acid-fast bacilli (AFB) was negative. Mantoux test (5 Tuberculin Units) showed no induration. Ultrasonography of the abdomen was normal.
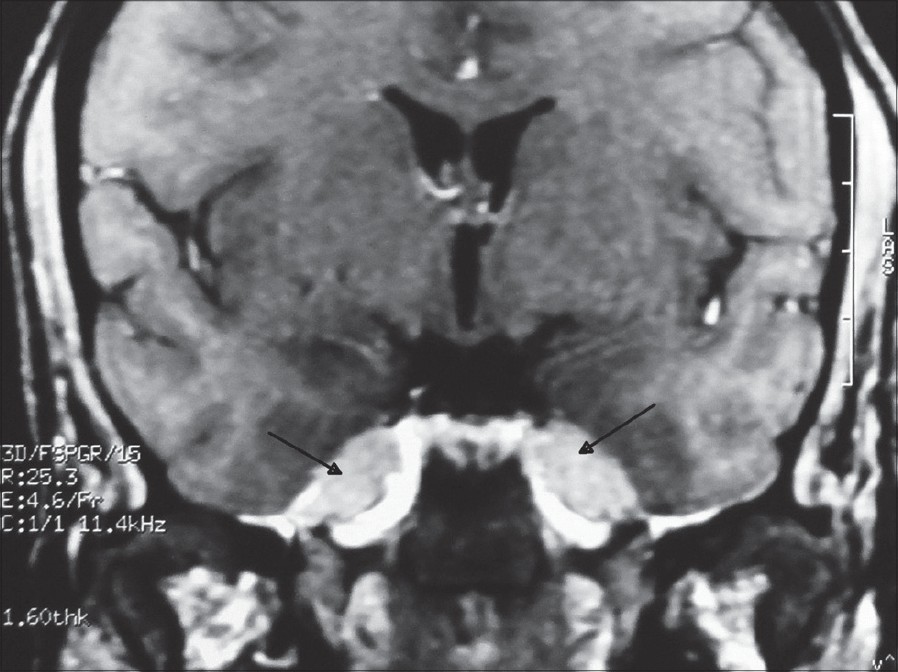 |
| Figure 3: MRI scan suggestive of neuro-sarcoid (marked by the black arrows) around cavernous sinus |
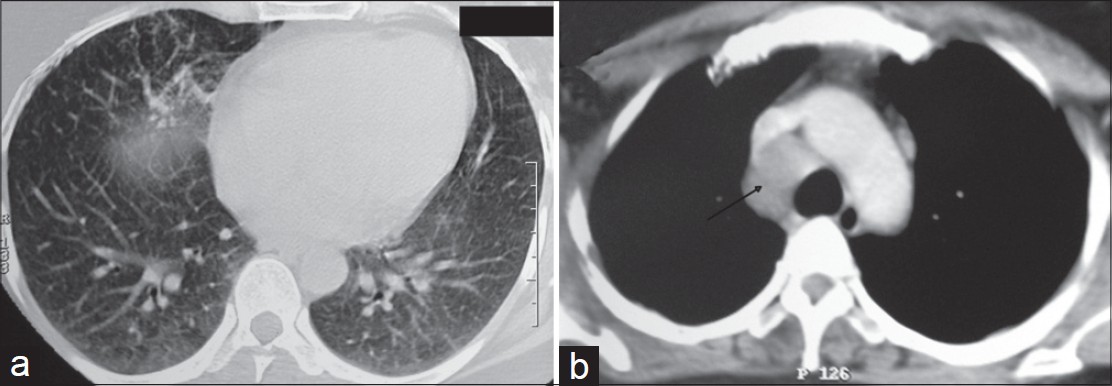 |
| Figure 4: CT scan thorax shows (a) Reticulonodular pattern, (b) Paratracheal lymphadenopathy (marked by the black arrow) |
We did a 4-mm lesional punch biopsy of skin from the ichthyotic lesions on the left leg. Histopathology [Figure - 5] revealed mild hyperkeratosis, thinning of granular layer, focal acanthosis, and multiple non-caseating well-formed epithelioid granulomas in the dermis without any infiltration of cutaneous appendages or nerves. Modified Fite staining and periodic acid-Schiff stain (PAS) were non-contributory.
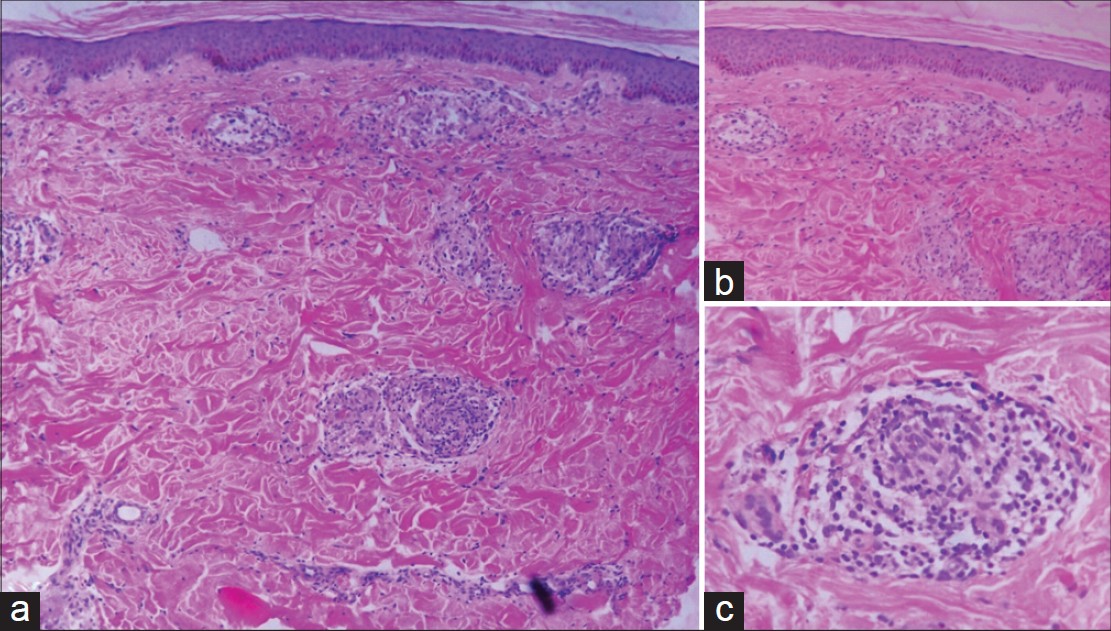 |
| Figure 5: (a) Non-caseating epithelioid granulomas in dermis (H and E stain, ×100), (b) Hyperkeratosis, thinning of granular layer, and a few epithelioid granulomas (H and E stain, ×100), (c) Noncaseating epitheliod granuloma in dermis (H and E stain, ×400) |
A biopsy specimen of apparently normal-appearing skin showed no histological abnormality. In the background of the clinical presentation (including the ichthyosiform skin lesions) and suggestive histopathology, a presumptive diagnosis of sarcoidosis was made. We did serum angiotensin converting enzyme (ACE) estimation that was markedly elevated. Subsequently cerebrospinal fluid (CSF) ACE level also showed gross elevation.
Serum calcium level was normal (8.4 mg/dl). Other laboratory investigations including biochemical panels were non-contributory except mild elevation of transaminase levels.
Based on the clinical and laboratory findings, histopathology, and imaging, a diagnosis of ichthyosiform sarcoidosis along with central nervous system (CNS) and pulmonary involvement was made. Oral prednisolone (60 mg/day) was started. Within a couple of weeks, the patient showed significant clinical and radiological improvement.
Discussion
The diagnosis of sarcoidosis is made based on the compatible clinical, laboratory, or radiological features along with histopathological evidence of non-caseating granuloma and when other potential causes, such as infections and foreign objects are excluded. [5] Sarcoidosis can virtually affect any organ system of our body. It mainly involve the lungs, mediastinal, and peripheral lymph nodes, skin, liver, spleen, eyes, and parotid glands. Less commonly, central nervous system, heart, upper respiratory tract, and bones are involved. As cutaneous lesions can exhibit a wide gamut of different morphologies, cutaneous sarcoidosis is known as one of the great masquerader in dermatology. [6] Skin manifestations of sarcoidosis are classified as "specific" or "nonspecific" depending on the presence or absence of noncaseating granuloma. [2] The common specific lesions include lupus pernio, infiltrated plaques, macular and papular lesions, and subcutaneous nodules. Hypopigmented patches, ulcers, alopecia, verrucous lesions, and ichthyosiform lesions are relatively less common specific manifestations. On the other hand, the commonest nonspecific lesion of sarcoidosis is erythema nodosum. [1]
Acquired ichthyosis has been reported to occur in association with a wide gamut of systemic illnesses. It is known to occur with Hodgkin′s disease, leprosy, drugs, hypothyroidism, lymphosarcoma, multiple myeloma, carcinomatosis, and chronic malnutrition among others. [1],[2],[7] In these instances, only ichthyosiform change is present histopathologically; microscopic alterations suggestive of or diagnostic of the generalized disease process with which they were related are not present. [2] Ichthyosis-like eruption may develop several months before the diagnosis of generalized sarcoidosis as in the present case.
Biopsy specimens frequently show not only non-caseating granuloma but also epidermal changes, which are consistent with ichthyosis vulgaris and which comprise of ortho-hyperkeratosis and a decreased or absent granular layer. [1]
The diagnosis of sarcoidosis in the present case was supported by the demonstration of well-formed epitheliod granuloma along with ichthyosiform changes in the skin biopsy specimen, negative Mantoux test, markedly raised ACE, hilar adenopathy in CXR, features of lung parenchymal involvement in the CT scan, and features suggestive of neurosarcoid in the MRI brain along with raised ACE level in CSF.
We searched the PubMed and Medline databases with the terms "ichyosiform sarcoidosis." Less than 20 reports of ichthyosiform sarcoidosis were found. It has been virtually always seen among non-white persons. Out of these, only a few cases have been reported in Indian patient. [8],[9] One case of ichthyosiform sarcoidosis without any systemic feature has been reported in a 25-year-old Indian woman. [8]
Another case of ichthyosiform sarcoidosis after chemotherapy for Hodgkin′s disease has been reported in a 36-year-old Indian man. [9] Ichthyosiform sarcoidosis typically presents as asymptomatic, adherent, and polygonal hyperpigmented scales on the lower extremities. [1] The presence of these ichthyosiform lesions correlates well with the presence of systemic disease. Ninety-five percent of all reported cases of ichthyosiform sarcoidosis have systemic involvement at the time of diagnosis or develop systemic involvement within several months. [1],[4] Treatment of sarcoidosis should be tailored to the patient and depends on the organ involvement and stage of the disease. Systemic corticosteroids are the most widely used drug for the treatment of systemic involvement in sarcoidosis. Other treatment options available are hydroxychloroquine, methotrexate, azathioprine, pentoxifylline, thalidomide, cyclophosphamide, cyclosporine, and infliximab among others. Topical steroids maybe considered for the treatment of anterior uveitis and skin lesions. [10] The ichthyosiform lesions have been reported to improve to both topical and systemic glucocorticoids. [1]
Association of multiple cranial nerve palsy as a manifestation of neuro-sarcoid along with ichthyosiform skin lesions was an unusual combination of features in our patient. We seek to emphasize the importance of excluding sarcoidosis in any patient with acquired ichthyosis. Furthermore, this case also highlight the importance of skin biopsy in the evaluation of acquired ichthyosis.
| 1. |
Rosenberg B. Ichthyosiform sarcoisis. Dermatol Online J 2005;11:15.
[Google Scholar]
|
| 2. |
Kauh YC, Goody HE, Luscombe HA. Ichthyosiform sarcoidosis. Arch Dermatol 1978;114:100-1.
[Google Scholar]
|
| 3. |
Feind-Koopmans AG, Lucker GP, van de Kerkhof PC. Acquired ichthyosiform erythroderma and sarcoidosis. J Am Acad Dermatol 1996;35:826-8.
[Google Scholar]
|
| 4. |
Haimovic A, Sanchez M, Judson MA, Prystowsky S. Sarcoidosis: A comprehensive review and update for the dermatologist: Part I. Cutaneous disease. J Am Acad Dermatol 2012;66:699.
[Google Scholar]
|
| 5. |
Zhang H, Ma HJ, Liu W, Yuan XY. Sarcoidosis characterized as acquired ichthyosiform erythroderma. Eur J Dermatol 2009;19:516-7.
[Google Scholar]
|
| 6. |
Yanardag H, Tetikkurt C, Bilir M, Demirci S, Iscimen A. Diagnosis of cutaneous sarcoidosis; clinical and the prognostic significanceof skin lesions. Multidiscip Respir Med 2013;8:26.
[Google Scholar]
|
| 7. |
Patel N, Spencer LA, English JC 3 rd , Zirwas MJ. Acquired ichthyosis. J Am Acad Dermatol 2006;55:647-56.
[Google Scholar]
|
| 8. |
Gangopadhyay AK. Ichthyosiform sarcoidosis. Indian J Dermatol Venereol Leprol 2001;67:91-2.
[Google Scholar]
|
| 9. |
Sawhney M, Sharma YK, Gera V, Jetley S. Ichthyosiform sarcoidosis following chemotherapy of Hodgkin's disease. Indian J Dermatol Venereol Leprol 2003;69:220-2.
[Google Scholar]
|
| 10. |
Wu JJ, Schiff KR. Sarcoidosis. Am Fam Physician 2004;70:312-22.
[Google Scholar]
|
Fulltext Views
4,882
PDF downloads
2,572





