Translate this page into:
Ichthyosis follicularis with alopecia and photophobia (IFAP) syndrome
Correspondence Address:
Vandana Mehta Rai
Department of Skin and STD, Kasturba Medical College, Manipal, Karnataka
India
| How to cite this article: Rai VM, Shenoi S D. Ichthyosis follicularis with alopecia and photophobia (IFAP) syndrome. Indian J Dermatol Venereol Leprol 2006;72:136-138 |
Abstract
A 12-year-old boy born of a nonconsanguineous marriage presented with dry rough skin and photophobia since birth. His growth and developmental milestones were normal and there was no history of any neurological problem, hearing deficit or scarring around the hair follicles. Cutaneous examination revealed diffuse thinning of scalp hair with loss of eyebrows and eyelashes and a sandpapery texture of the skin all over the body, suggestive of ichthyosis follicularis with alopecia and photophobia syndrome.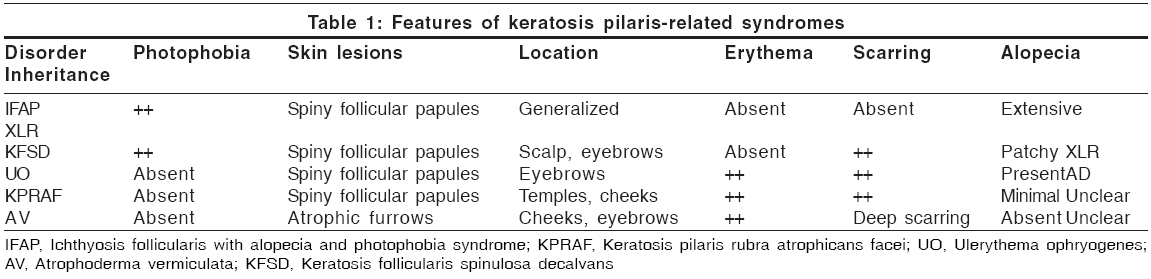
 |
 |
 |
 |
 |
 |
 |
 |
Introduction
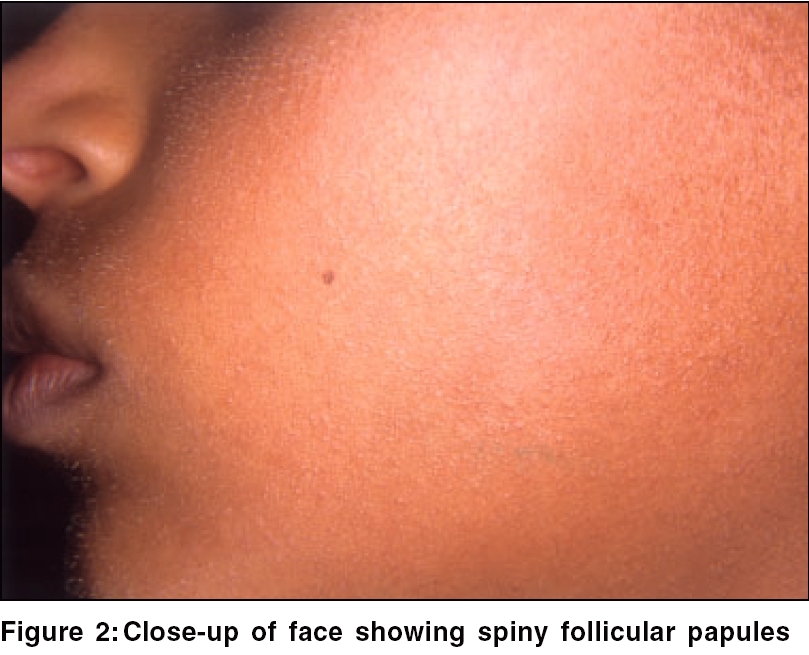
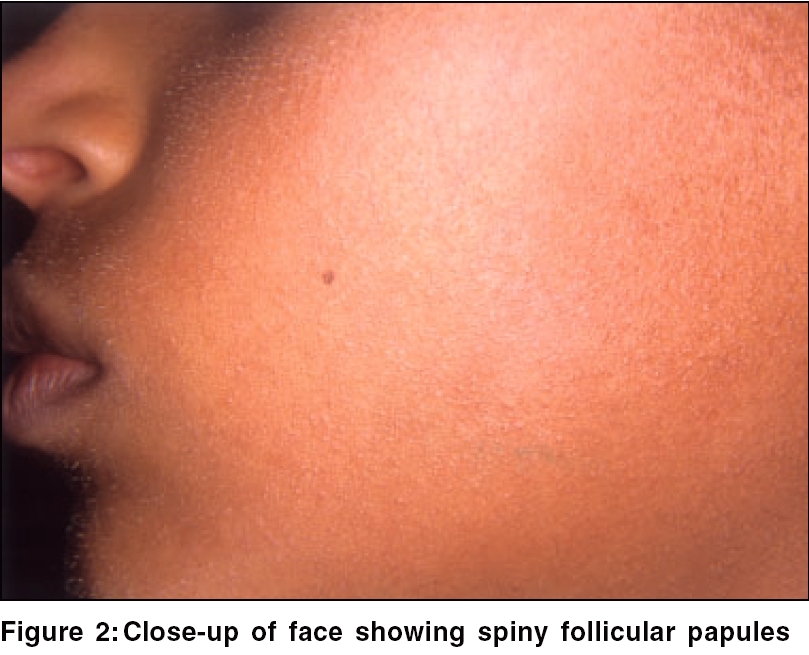
Ichthyosis refers to a relatively uncommon group of skin disorders characterized by the presence of excessive amounts of dry surface scales. It is regarded as a disorder of keratinization or cornification and it is due to abnormal epidermal differentiation or metabolism. Ichthyosis follicularis is a keratinization disorder characterized by spiny follicular papules all over the body since birth. It can occur as a part of IFAP (ichthyosis follicularis, atrichia, photophobia) syndrome.
Case Report
A 12-year-old boy presented with complaints of dry rough skin and photophobia since birth. He also had diffuse hair loss of 3 months′ duration. He was born of a nonconsanguineous marriage and had normal growth and developmental milestones. However, he was devoid of eyebrows and eyelashes since birth. There was no history of any neurological or hearing deficit, sweating defect, collodion membrane, ectropion, eclabium, redness around the hair follicles, or scarring. There was a history of photophobia since birth with redness and watering of eyes while going out in sunlight. Similar complaints were absent in other family members; however, his mother and grandmother gave a history of dry skin since birth.
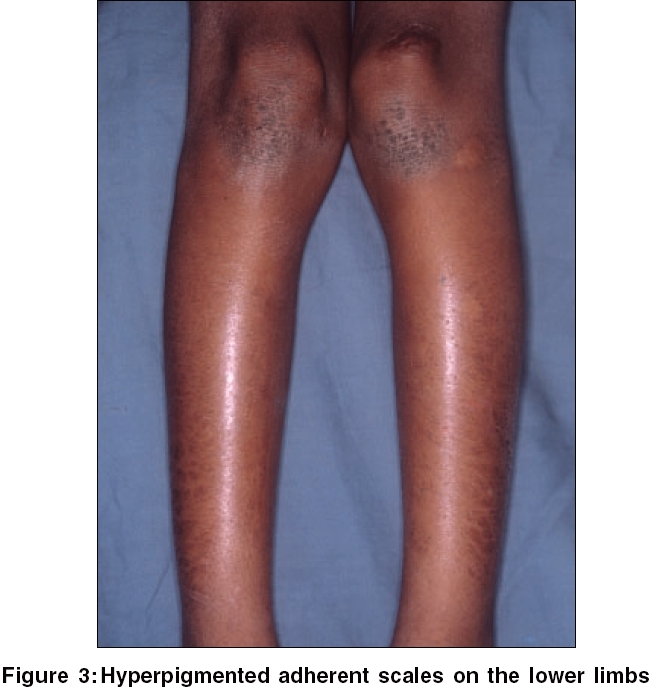
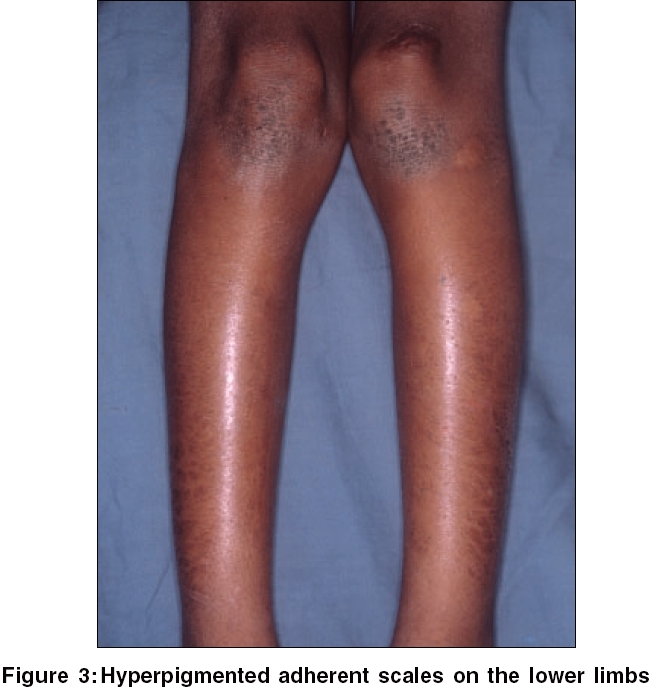
On examination, there was diffuse thinning of scalp hair. His skin was of a sand paper texture with spiny follicular papules over the face [Figure - 1], arms, back and limbs. There were hyperpigmented scaly hyperkeratotic plaques on the elbows and knees and hyperpigmented adherent scales on the lower limbs [Figure - 2]. His eyebrows and eyelashes were partially lost [Figure - 3].
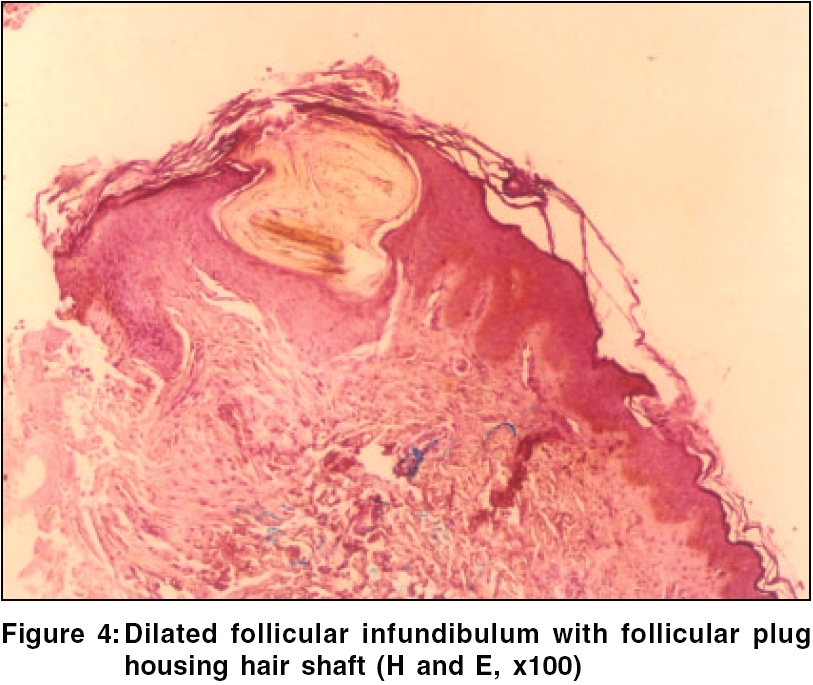
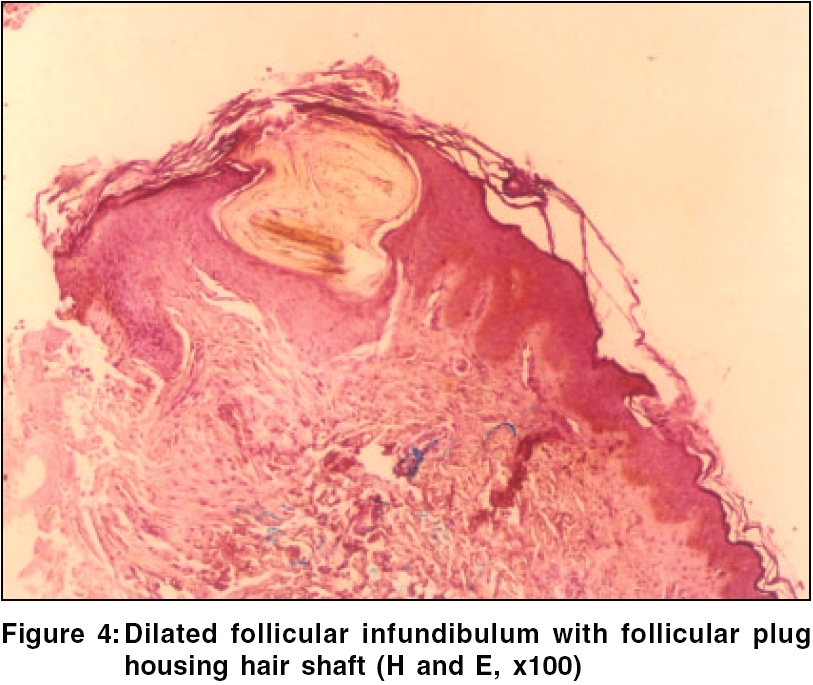
All routine hematological and biochemical investigations were normal. A skin biopsy from a spiny follicular papule revealed a hyperkeratotic epidermis with an orthokeratotic plug within a dilated follicular ostium containing an entrapped hair shaft with perivascular lymphohistiocytic infiltrate in the dermis [Figure - 4]. Hair shaft examination was normal. Based on the history and clinical examination, a provisional diagnosis of generalized keratosis pilaris with photophobia and diffuse hair loss was considered. However, the unusual association of photophobia and hair loss prompted us to reconsider our diagnosis to ichthyosis follicularis with alopecia and photophobia (IFAP) syndrome.
Discussion
Ichthyosis follicularis (IF) was characterized as a distinct entity by Macleod in 1909, although Lesser first used the term IF in 1885 to describe a 6-year-old boy with congenital alopecia of the scalp and eyebrows and keratotic follicular papules on the body. He believed that the hyperkeratotic follicular papules were a manifestation of a localized form of ichthyosis.[1]
Patients with IFAP share a unique appearance because of striking alopecia, severe photophobia and generalized cutaneous ′thorn-like′ projections. The spines impart a peculiar sensation on palpation that has been described as resembling a ′nutmeg grater′ or ′the prickly surface of a rose leaf.′ The teeth and nails are normal and no abnormalities of sweat production have been noted. Hyperkeratosis is sometimes present over the elbows and knees, but there is no palmoplantar keratoderma.
Males with IFAP syndrome have an inexorable progression of corneal vascularization and loss of vision. Retinal vascular tortuosity may be a clinical sign of carrier status in females.[2] IFAP syndrome has been reported with mental retardation, seizures, cutaneous infections and inguinal hernia.[3]
The histopathological findings are rather nonspecific and include dilated follicles filled with keratin plugs that extend above the level of the skin, forming acuminate papules; absence of sebaceous glands; and normal sweat glands.[4]
IFAP syndrome results from congenital absence of or marked defect in the pilosebaceous apparatus. The follicular hyperkeratosis is believed to be secondary to the obstruction of sebum. A limited number of patients with this disorder have been described and X-linked recessive inheritance has been proposed.[5] This disorder has been reported occurring simultaneously in a mother and daughter.[6]
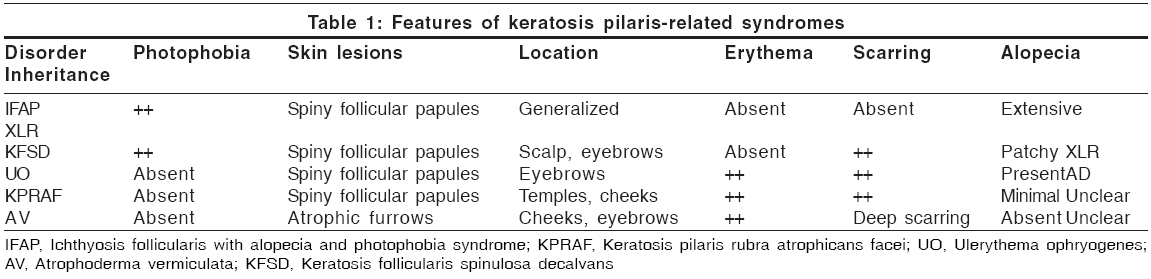
IFAP syndrome must be differentiated from other keratosis pilaris variants such as ulerythema ophryogenes, keratosis pilaris rubra atrophicans faciei, atrophoderma vermiculata and keratosis follicularis spinulosa decalvans [Table - 1].[2]
Keratosis follicularis spinulosa decalvans (KFSD) is a rare X- linked recessive disorder characterised by spiny follicular papules that may disappear, leaving behind follicular scars. There may be scarring alopecia along with punctate defects of cornea and photophobia. Palmoplantar keratoderma may be associated; however, the nails and teeth are normal. Even though there is a great similarity between keratosis follicularis spinulosa decalvans and IFAP syndrome, our patient had IFAP syndrome since he had no scarring.
The prognosis of IFAP syndrome is variable. The cutaneous lesions improve with keratolytics, emollients and urea preparations. Oral retinoids also have been tried in its management; however, topical retinoids are not suitable because of their irritation potential. This case is being reported for its presentation similar to the keratosis pilaris variants, which should be considered in its differential diagnosis.
| 1. |
Macleod JMH. Three cases of 'ichthyosis follicularis' associated with baldness. Br J Dermatol 1909;21:165-89.
[Google Scholar]
|
| 2. |
Traboulsi E, Aaked N, Megarbane H, Megarbane A. Ocular findings in Ichthyosis follicularis, alopecia, photophobia (IFAP) syndrome. Ophthalmic Genet 2004;25:153-6.
[Google Scholar]
|
| 3. |
Boente MC, Bibas-Bonet H, Coronel AM, Asial RA. Atrichia, ichthyosis, follicular hyperkeratosis, chronic candidiasis, keratitis, seizures, mental retardation and inguinal hernia: a severe manifestation of IFAP syndrome. Eur J Dermatol 2000;10:98-102.
[Google Scholar]
|
| 4. |
Eramo LR, Esterly NB, Zieserl EJ, Stock EL, Herrmann J. Ichthyosis follicularis with alopecia and photophobia. Arch Dermatol 1985;121:1167-74.
[Google Scholar]
|
| 5. |
Cambiagi S, Barbareschi M, Tadini G. Ichthyosis follicularis with atrichia and photophobia (IFAP) syndrome in two unrelated female patients. J Am Acad Dermatol 2002;46:156-8.
[Google Scholar]
|
| 6. |
Sato-Matsumura KC, Matsumura T, Kumakiri M, Hosokawa K, Nakamura H, Kobayashi H, et al. Ichthyosis follicularis with alopecia and photophobia in a mother and daughter. Br J Dermatol 2000;142:157-62.
[Google Scholar]
|
Fulltext Views
3,716
PDF downloads
2,236





