Translate this page into:
Idiopathic bullous eosinophilic cellulitis (Wells syndrome) responsive to topical tacrolimus and antihistamine combination
2 Department of Pathology, University College of Medical Sciences (University of Delhi) and Guru Teg Bahadur Hospital, Delhi University, Delhi, India
Correspondence Address:
Prashant Verma
Department of Dermatology and STD, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi University, Delhi
India
| How to cite this article: Verma P, Singal A, Sharma S. Idiopathic bullous eosinophilic cellulitis (Wells syndrome) responsive to topical tacrolimus and antihistamine combination. Indian J Dermatol Venereol Leprol 2012;78:378-380 |
Sir,
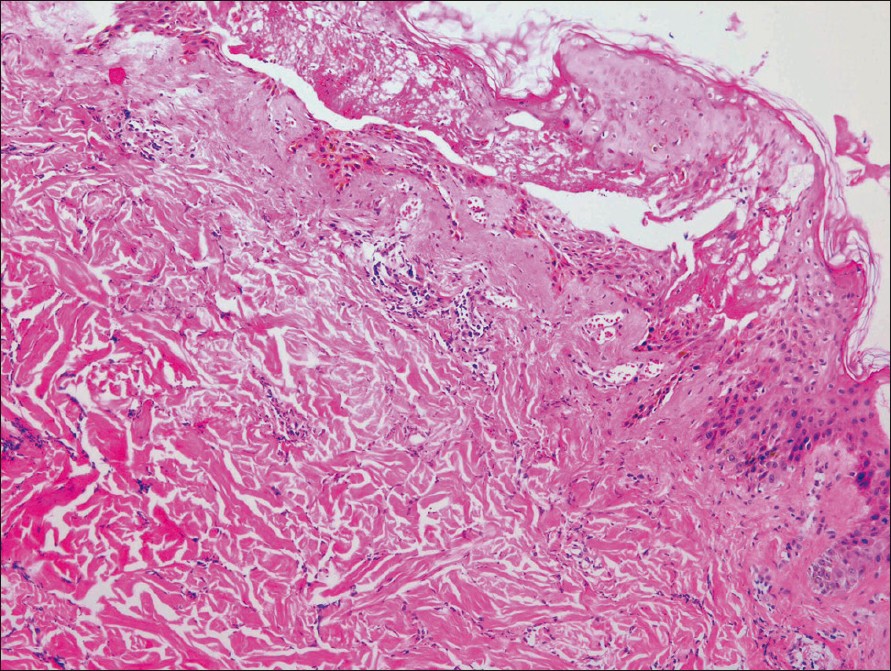
A 40-years-old man presented with recurrent, slightly itchy, red-colored eruptions over trunk for 2 months. He had received multiple antibiotics for the eruptions without any improvement. He denied history of Raynaud′s phenomenon, dysphagia, fever, joint pains, malaise, photosensitivity, oral ulcerations, weight loss and anorexia. He also denied any drug intake, vaccinations, and arthropod bites. Physical examination revealed multiple erythematous-tumid, non-tender, non-calor plaques over abdomen, back and proximal arms. The surface of the lesions depicted vesicles and bullae [Figure - 1]. Nikolsky sign and bulla spread sign were negative. Rest of the mucocutaneous and systemic examination was unremarkable. Histopathological examination of the section from a representative lesion revealed epidermal spongiosis and spongiotic vesicles, superficial and deep interstitial lymphocytic and eosinophilic infiltrate [Figure - 2]. Flame figures, eosinophilic debris hugging the collagen fibers, were prominent [Figure - 3]. Periodic-acid-Schiff stain showed neither fungal elements nor mucin. Tissue culture on Sabouraud′s agar failed to isolate any fungus. Other instrumental tests including complete blood counts, peripheral smear, absolute eosinophil count, serum IgE levels, liver and renal functions, blood sugar, ELISA for HIV, and microscopic urine analysis were normal. Serum levels of antinuclear antibody (ANA) estimated by indirect immunoflouresence on Hep-2 cell line, and antineutrophilic cytoplasmic antibody (ANCA) were also normal. Imaging studies including a chest X-ray and an ultrasound of the abdomen were normal. A diagnosis of Wells syndrome was made and the patient was started on cetrizine tablets, 10 mg twice a day. The lesions regressed completely after 2 weeks leaving behind some induration. Cetirizine was continued at a dose of 10 mg once daily for further 4 weeks and was finally stopped. Nine weeks later, the patient had a recurrence of similar lesions. He was started on cetrizine 10 mg twice a day. This time, the lesions showed a minimal response even after 4 weeks of treatment. Topical 0.1% tacrolimus ointment was added to the treatment regimen. The lesions resolved completely after 2 weeks of treatment leaving hypopigmentation [Figure - 4] and some induration. Ever since the patient has been on follow-up for the last 6 months with no recurrence. Wells′ syndrome, or eosinophilic cellulitis, is a recurrent, hypersensitivity reaction to an arthropod bite, drug, infections, Churg-Strauss syndrome, or an overlap with hypereosinophilic syndrome. [1] Aberrant and inadequate eosinophil skin homing may be one of the key mechanisms of the pathogenesis of Wells syndrome. Pruritic, erythematous-edematous plaques that evolve rapidly over 2-3 days are its salient clinical features. The lesions often regress spontaneously over 2-8 weeks, leaving residual skin atrophy and hyperpigmentation, which may masquerade as morphea/scleroderma. [2] The disease may follow a waxing-waning, recurrent course, which may last for years. [3] The diagnosis should be considered in those with presumed cellulitis and eosinophilia who fail to respond to antibiotics.
Vesiculo-bullous lesions, due to spongiosis, have been described on occasions; Churg-Strauss syndrome in some while unidentified in others. [1],[4] Histopathological findings follow an evolutionary course through acute, subacute, and resolving stages. [2] Dermal edema and an eosinophilic infiltrate in the upper and deep dermis characterize the acute stage. "Flame figures", intense eosinophilic degranulation of major basic protein coating collagen bundles in the dermis, are the hallmark of subacute stage. Phagocytic histiocytes palisading around the flame figures, and granulomas represent a resolving lesion.
 |
| Figure 1: Wells syndrome, depicting edematous - erythematous plaques with the presence of vesiculo - bullous lesions over the surface, present on back |
 |
| Figure 2: Section from a representative lesion illustrating spongiotic vesicles in the epidermis and interstitial lymphocytic and eosinophilic inflammatory infiltrate in the dermis (H and E, ×100) |
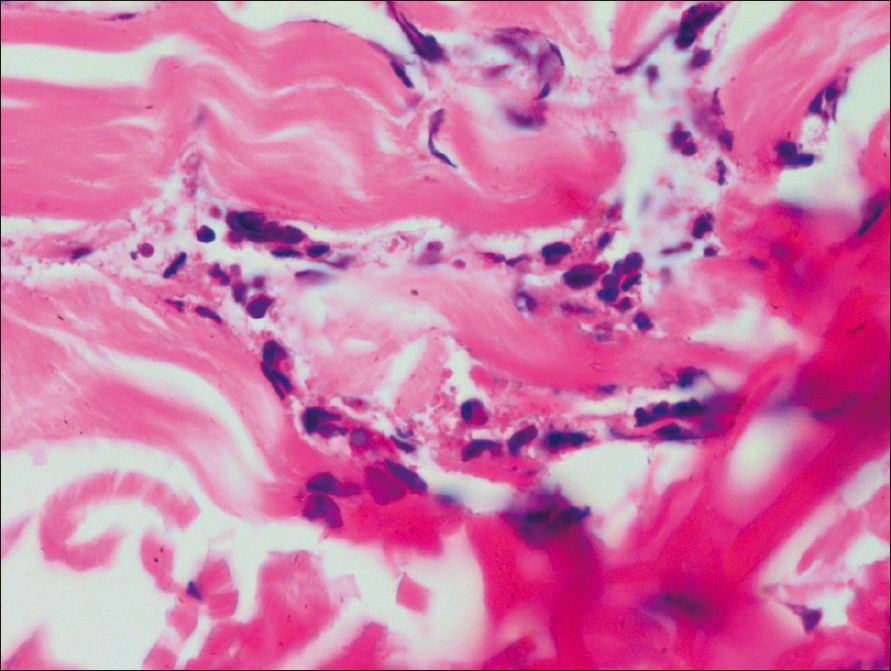 |
| Figure 3: Section from a representative lesion demonstrating a flame Figure (H and E, ×400) |
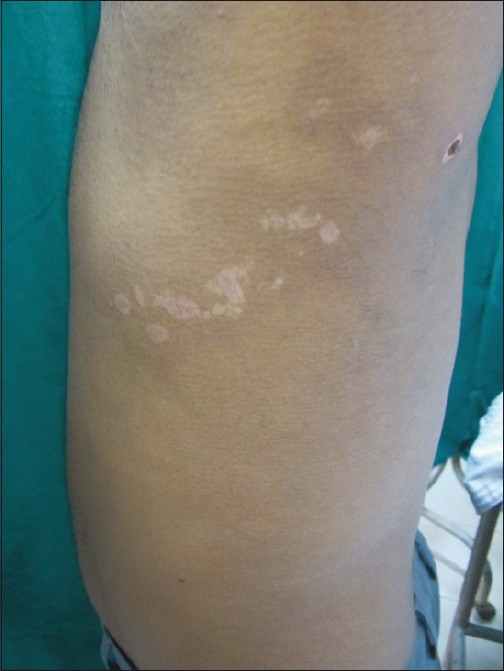 |
| Figure 4: Follow - up photograph at 2 weeks showing resolution of the lesions on back, leaving behind hypopigmentation |
Owing to the scarcity of evidence, it is difficult to draw conclusions regarding whether the existing therapies for eosinophilic cellulitis are truly effective or these cases resolve spontaneously yet oral corticosteroids have been found to be the most effective therapy. In the present case, the patient was started on cetrizine right at the initial presentation and corticosteroids were planned after getting the relevant investigations done. However, there was regression of the lesions while on cetirizine alone initially, therefore, it was decided to avoid aggressive immunosuppressive therapy in the case. If an infection or other treatable precipitating factors can be identified, then there is often improvement with treatment of the underlying condition. [1] A 12-years-old girl with Wells syndrome had a complete recovery with cetirizine. [5] The present case too, responded well to cetirizine. Tacrolimus (FK-506) is a strong immunosuppressant, which also downregulates the high-affinity IgE receptor I(FcRI) expression on Langerhans cells, a pathogenic event in the formation of flame figures. Levels of eosinophilic cationic protein, a key molecule in the pathogenesis of flame figures, have been shown to fall after treatment with tacrolimus eye drops in patients with atopic keratoconjuctivitis. [6] Besides, oral tacrolimus has been successfully used in recurrent eosinophilic cellulitis. [7] Therefore, it was decided to use topical tacrolimus in conjunction with cetirizine. Other options [7] include topical corticosteroids, antimicrobials including minocycline and dapsone; colchicine; antimalarial drugs; and psoralen with ultraviolet A (PUVA), systemic corticosteroids, low-dose cyclosporine, azathioprine, and interferon. [7]
| 1. |
Fujimoto N, Wakabayashi M, Kato T, Nishio C, Tanaka T. Wells syndrome associated with Churg-Strauss syndrome. Clin Exp Dermatol 2011;36:46-8.
[Google Scholar]
|
| 2. |
Moossavi M, Mehregan DR. Wells' syndrome: A clinical and histopathologic review of seven cases. Int J Dermatol 2003;42:62-7.
[Google Scholar]
|
| 3. |
Gilliam AE, Bruckner AL, Howard RM, Lee BP, Wu S, Frieden IJ. Bullous "cellulitis" with eosinophilia: Case report and review of Wells' syndrome in childhood. Pediatrics 2005;116:e149-55.
[Google Scholar]
|
| 4. |
Katoulis AC, Bozi E, Samara M, Kalogeromitros D, Panayiotides I, Stavrianeas NG. Idiopathic bullous eosinophilic cellulitis (Wells' syndrome). Clin Exp Dermatol 2009;34:e375-6.
[Google Scholar]
|
| 5. |
Aroni K, Aivaliotis M, Liossi A, Davaris P. Eosinophilic cellulitis in a child successfully treated with cetirizine. Acta Derm Venereol 1999;79:332.
[Google Scholar]
|
| 6. |
Wakamatsu TH, Tanaka M, Satake Y, Dogru M, Fukagawa K, Igarashi A, et al. Eosinophil cationic protein as a marker for assessing the efficacy of tacrolimus ophthalmic solution in the treatment of atopic keratoconjunctivitis. Mol Vis 2011;17:932-8.
[Google Scholar]
|
| 7. |
Ohtsuka T. Oral tacrolimus treatment for refractory eosinophilic cellulitis. Clin Exp Dermatol 2009;34:e597-8.
[Google Scholar]
|
Fulltext Views
3,300
PDF downloads
1,527





