Translate this page into:
Imatinib mesylate-induced severe lichenoid rash
2 Department of Internal Medicine, Postgraduate Institute of Medical Education and Research, Chandigarh, India
3 Department of Histopathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Correspondence Address:
Dipankar De
Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh - 160 012
India
| How to cite this article: A, De D, Malhotra P, Saikia UN. Imatinib mesylate-induced severe lichenoid rash. Indian J Dermatol Venereol Leprol 2014;80:93-95 |
Sir,
Imatinib mesylate is a potent selective inhibitor of aberrantly expressed tyrosine kinases, central to the pathogenesis of some malignancies like Philadelphia-chromosome positive chronic myeloid leukaemia (Ph+ CML). As the list of cutaneous side effects to imatinib is ever increasing, prompt updates are necessary to enable caregivers to diagnose and treat it more competently.
A 47-year-old female patient was diagnosed with Ph+ CML in accelerated phase by the Hematology services of our institute in April, 2012. She achieved hematological remission with imatinib mesylate (STI 571, Gleevec ; Novartis) 800 mg/day, procured through Novartis Oncology Access program. She was also a known hypertensive, on enalapril for the past 4 years.
After 3-months of imatinib therapy, she started developing crops of pruritic mucocutaneous lesions. On referral, we found multiple lichenoid papules and plaques with minimal scaling, in a photo-distributed pattern on V-area of neck, upper back and dorsa of hands. Well-demarcated, brightly erythematous and hyperkeratotic plaques were present on palms and soles, extending over to the dorsal surfaces of fingers and toes respectively [Figure - 1]a and b. Scalp showed bright pink erythema with overlying scaling [Figure - 2]a. Mucosal involvement was confined to the lower labial mucosa (photo-distributed pattern) and showed a violaceous reticulate plaque with polycyclic margins and superficial erosions [Figure - 2]b. Rest of the oral mucosa and genital mucosa were spared. No evidence of any dental amalgam filling was found. All 20 nails were involved with onycholysis, subungual hyperkeratosis, and onychomadesis, with right great toe nail progressing towards total dystrophy. Potassium hydroxide mount of nail clippings was found to be negative for fungal elements. No history of any previous chronic skin disease was present. General physical examination was non-contributory except for peri-orbital and pedal edema. On the basis of these findings, a clinical diagnosis of lichenoid drug eruption due to imatinib was suggested. Palmoplantar hyperkeratosis, scalp scaling and nail involvement mimicking psoriasiform dermatitis prompted a biopsy.
 |
| Figure 1: (a) Well-demarcated, brightly erythematous to lichenoid, hyperkeratotic plaques present on the palms. (b) Similar rash on dorsal surface of fingers along with nail dystrophy |
 |
| Figure 2: (a) Bright pink erythematous rash with overlying scaling on the scalp. (b) Violaceous reticulate plaque with polycyclic margins and superficial erosions on the lower labial mucosa |
Histopathology of a representative skin lesion revealed hyperkeratosis, hypergranulosis with focal areas of parakeratosis, basal layer degeneration, few apoptotic keratinocytes, band-like lympho-plasmacytic dermal infiltrate and pigment incontinence [Figure - 3]a. Scalp biopsy showed similar changes with a more severe inflammation, resulting in a cleft at dermoepidermal junction [Figure - 3]b, there by negating any psoriasiform dermatitis.
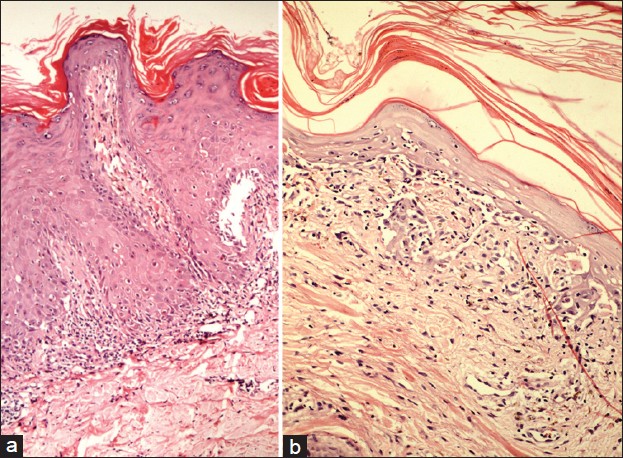 |
| Figure 3: (a) Histological section from the representative skin lesion showing hyperkeratosis, hypergranulosis with focal parakeratosis, basal layer degeneration and few apoptotic keratinocytes, and a band-like lymphoplasmacytic infiltrate in the dermis (H and E, ×100). (b)Scalp section showing more severe infl ammation, resulting in a cleft at the dermo-epidermal junction (H and E, ×100) |
The patient responded well to oral prednisolone, 0.5 mg/kg body weight, which was gradually tapered until discontinuation after 4 months. Lichenoid rash subsided with residual hyperpigmentation, while toe nail dystrophy seemed permanent. Imatinib therapy was maintained throughout at the same dosage in view of its high benefit-risk ratio and the unaffordable cost of second generation tyrosine kinase inhibitors.
Imatinib is a relatively new addition to the list of drugs causing lichenoid eruptions. Dose-dependent relationship of this drug with rash is a result of its pharmacological effect, by altering signal transduction mechanisms rather than its immunological effect. Lichenoid rash generally appears after 1 to 6 months of imatinib therapy. [1] A photo-distributed pattern is generally seen, [2],[3],[4] with lesions healing with hyperpigmentation, [5] as was also observed in our case. Extensive mucocutaneous involvement with palmo-plantar hyperkeratosis along with scalp and 20 nail involvement, as seen in this patient, is uncommon for a lichenoid eruption and has not been observed with imatinib so far. Severe inflammation resulting in histopathological dermoepidermal split in scalp lesions is also unusual for drug induced lichenoid reaction.
Kuraishi et al., [1] reported a case of lichenoid eruptions on extremities with palmo-plantar hyperkeratosis that responded to temporary discontinuation of imatinib. Another case of mucocutaneous lichenoid eruptions with palmo-plantar hyperkeratosis and single nail involvement in the form of longitudinal ridging has been described by Wahiduzzaman and Pubalan. [6] Subungual hyperkeratosis of finger and toe nails accompanying lichenoid eruptions on chest and upper limbs, sparing mucosa, has also been described in one patient by Dalmau et al., [7] that required substitution of imatinib with hydroxyurea.
Imatinib-induced or exacerbated psoriasis is a known entity. Palmoplantar hyperkeratosis revealing psoriasiform histology has been seen in three patients. [8] They all required discontinuation or reduction of imatinib dose for reversion of the cutaneous and nail changes. Altered tyrosine kinase signalling with the possible role of platelet-derived growth factor receptor and c-kit has been proposed as the underlying mechanism. [9] On the contrary, a report of improvement of preexisting psoriasis in another patient on imatinib, has added to the ambiguity. [10]
Most imatinib-induced lichenoid eruptions are well-managed conservatively. A minority require either dose reduction or temporary withdrawal of imatinib and simultaneous therapy with systemic steroids. [1] Even low-dose acitretin has been tried with good results in some patients, especially those with hyperkeratotic lesions, with the added benefit of its antineoplastic effect. [7]
While expanding the spectrum of lichenoid rash induced by imatinib, this case emphasizes on differentiating it from psoriasiform dermatitis. Also, extensive lichenoid reactions can be dealt with by a short course of systemic steroids, without any need for withdrawal or dose alteration of this life-saving drug.
| 1. |
Kuraishi N, Nagai Y, Hasegawa M, Ishikawa O. Lichenoid drug eruption with palmoplantar hyperkeratosis due to imatinib mesylate: A case report and a review of the literature. Acta Derm Venereol 2010;90:73-6.
[Google Scholar]
|
| 2. |
Pascual JC, Matarredona J, Miralles J, Conesa V, Borras-Blasco J. Oral and cutaneous lichenoid reaction secondary to imatinib: Report of two cases. Int J Dermatol 2006;45:1471-3.
[Google Scholar]
|
| 3. |
Brazzelli V, Muzio F, Manna G, Moggio E, Vassallo C, Orlandi E, et al. Photoinduced dermatitis and oral lichenoid reaction in a chronic myeloid leukemia patient treated with imatinib mesylate. Photodermatol Photoimmunol Photomed 2012;28:2-5.
[Google Scholar]
|
| 4. |
Sendagorta E, Herranz P, Feito M, Ramírez P, Feltes R, Floristán U, et al. Lichenoid drug eruption related to imatinib: Report of a new case and review of the literature. Clin Exp Dermatol 2009;34:e315-6.
[Google Scholar]
|
| 5. |
Kagimoto Y, Mizuashi M, Kikuchi K, Aiba S. Lichenoid drug eruption with hyperpigmentation caused by imatinib mesylate. Int J Dermatol 2013. [In press].
[Google Scholar]
|
| 6. |
Wahiduzzaman M, Pubalan M. Oral and cutaneous lichenoid reaction with nail changes secondary to imatinib: Report of a case and literature review. Dermatol Online J 2008;14:14.
[Google Scholar]
|
| 7. |
Dalmau J, Peramiquel L, Puig L, Fernández-Figueras MT, Roé E, Alomar A. Imatinib-associated lichenoid eruption: Acitretin treatment allows maintained antineoplastic effect. Br J Dermatol 2006;154:1213-6.
[Google Scholar]
|
| 8. |
Deguchi N, Kawamura T, Shimizu A, Kitamura R, Yanagi M, Shibagaki N, et al. Imatinib mesylate causes palmoplantar hyperkeratosis and nail dystrophy in three patients with chronic myeloid leukaemia. Br J Dermatol 2006;154:1216-8.
[Google Scholar]
|
| 9. |
Dickens E, Lewis F, Bienz N. Imatinib: A designer drug, another cutaneous complication. Clin Exp Dermatol 2009;34:603-4.
[Google Scholar]
|
| 10. |
Miyagawa S, Fujimoto H, Ko S, Hirota S, Kitamura Y. Improvement of psoriasis during imatinib therapy in a patient with a metastatic gastrointestinal stromal tumour. Br J Dermatol 2002;147:406-7.
[Google Scholar]
|
Fulltext Views
3,963
PDF downloads
3,016





