Translate this page into:
Immunotherapy using topical measles, mumps and rubella vaccine for treatment of verruca plana
Corresponding author: Dr. Suresh Kumar Jain, Department of Dermatology, Venereology and Leprosy, Government Medical College, Kota - 324 005, Rajasthan, India. drsuresh253@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mohta A, Kushwaha RK, Gautam U, Jain SK. Immunothesrapy using topical measles, mumps and rubella vaccine for treatment of verruca plana. Indian J Dermatol Venereol Leprol 2021;87:285-7.
Sir,
Verruca plana or plane warts are flat or slightly raised papular lesions, caused by human papillomavirus (HPV), seen commonly over sites prone to trauma such as face, neck and extremities. Recently, immunotherapy has emerged as an effective modality for warts by enhancing the patient’s delayed hypersensitivity immune reaction. Intralesional measles, mumps and rubella (MMR) vaccine has established itself to be reliable immunotherapy for warts.1,2 Here we report 2 cases of verruca plana, treated with topical MMR vaccine at the department of dermatology, Government Medical College, Kota, Rajasthan.
The first case was of an 18-year-old male patient who presented with multiple hyperpigmented flat-topped papules on the right cheek, temple, bilateral eyelids and forehead for 9 months. He had already been diagnosed to have verruca plana with koebnerization, six months back, for which he was prescribed oral zinc-sulfate and topical tretinoin for two months, with no relief, followed by chemical cauterization using topical trichloroacetic acid (TCA) three months back, before recurrence. The patient had stopped all treatment for the last three months. His immunocompetent status was ensured by carrying out hemogram, renal and liver function test, serology for HIV, hepatitis B and C and VDRL test. The patient was advised not to take any concurrent treatment during this time. The lesional skin was wiped with normal saline and allowed to dry. Standardized lyophilized MMR vaccine (live) I.P. (freeze-dried) TRESIVAC® was reconstituted with 0.5 mL of distilled water and the entire volume was applied over warts for two hours under plastic occlusive dressing. After once a week application for six consecutive weeks, all verruca plana simultaneously disappeared only, leaving behind residual hyperpigmentation [Figures 1 and 2].
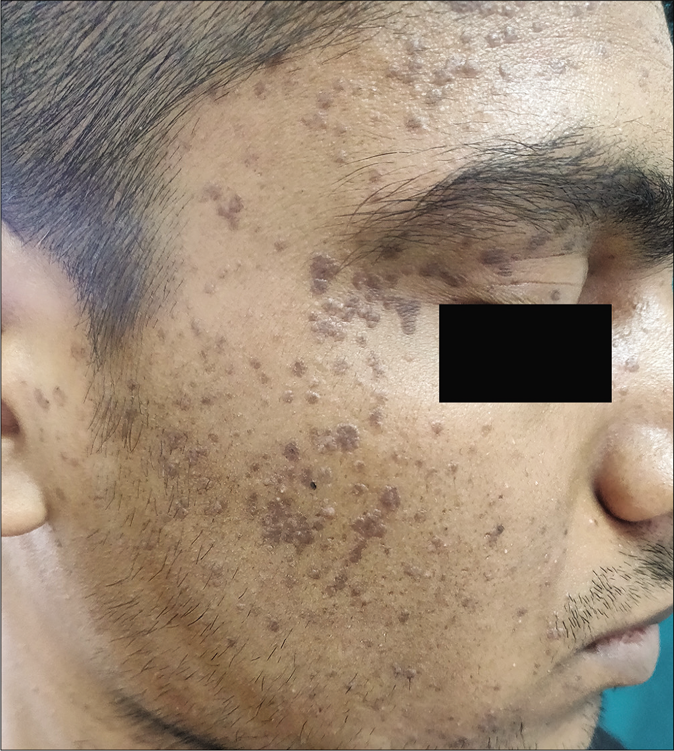
- Multiple verruca plana on right side of face before treatment
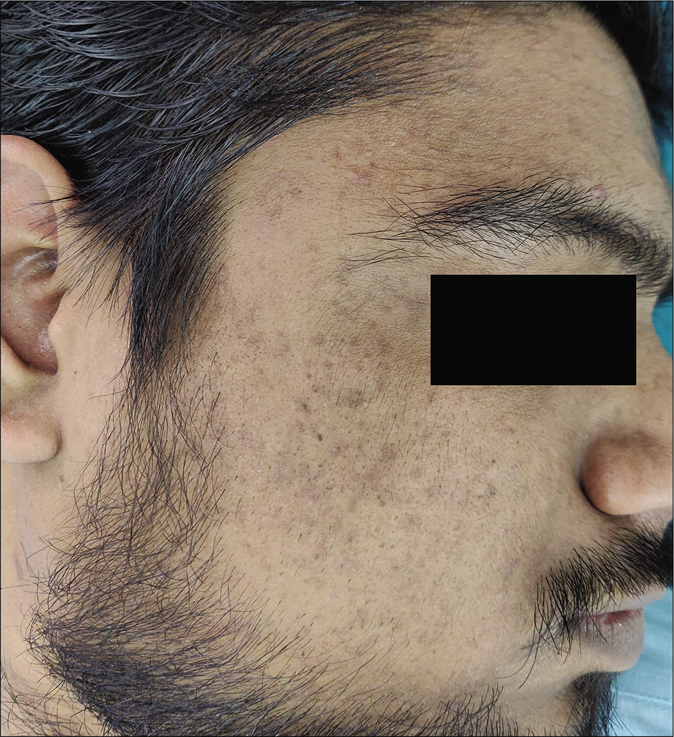
- Complete clearance with residual hyperpigmentation on right side of face after 6 applications
Another patient, a 21-year-old immunocompetent man, presented with multiple clustered flesh-colored smooth papules over the bilateral mandibular and mental region, first noticed by him within three weeks of getting his beard shaved at a new local barbershop. As he continued to shave, he observed a gradual increase in the number of lesions over the last six months. Similar discreet lesions were also present over the temple and forehead. A clinical diagnosis of verruca plana was made, confirmed by histopathological examination revealing hyperkeratosis, mild papillomatosis, and koilocytes in suprabasal layers. The patient was treated similarly with weekly topical MMR application under a plastic occlusive dressing for the next five weeks, which resulted in the complete disappearance of all verruca plana [Figures 3 and 4].
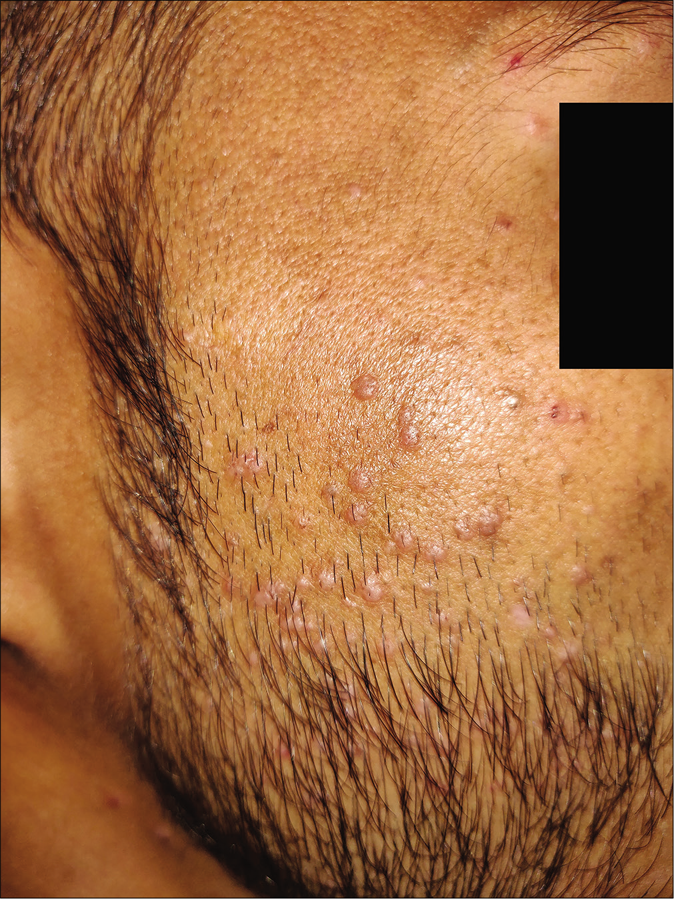
- Multiple verruca plana on right side of face before treatment
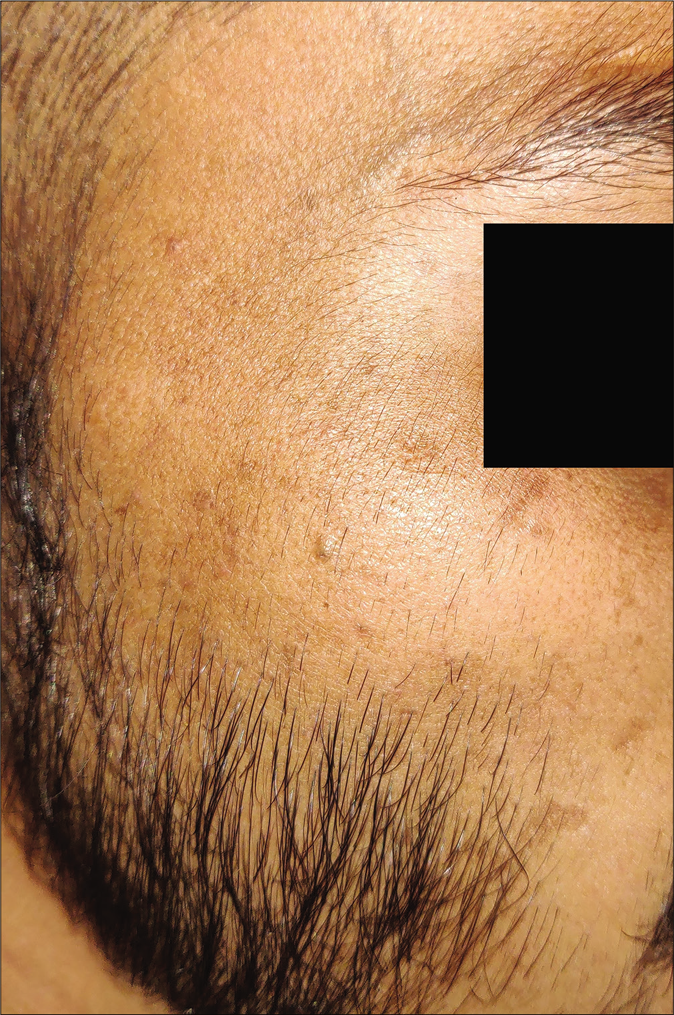
- Complete clearance on right side of face after 5 applications of topical measles, mumps and rubella vaccine
Both patients were explained beforehand about the experimental nature of the therapy. A monthly follow-up was done in both the patients for the next three months, with no recurrence. Various conventional modalities used to treat warts include destruction with salicylic acid, trichloroacetic acid, surgical excision, cryotherapy, and lasers; antiviral (cidofovir), and antiproliferative agents like podophyllin, etc.3 Most of these procedures are either cumbersome or painful with high recurrence rates. Recently immunotherapy has emerged as an alternative treatment option. It is indicated for recalcitrant, recurrent, extensive, and difficult to treat (periungual, palmoplantar) warts.3 Various immunotherapies include autoimplantation, vitamin D3, mumps antigen, candida antigen, Trichophyton skin test antigen, purified protein derivative tuberculin, and e BCG, MMR, and Mycobacterium w vaccine.2 They are most commonly given intralesionally. The only topical immunotherapies tried in the past are topical BCG, sinecatechins, and imiquimod.3,4 MMR vaccine clears the virus and infected keratinocytes by stimulating humoral and cell-mediated immunity. The use of three antigens together helps to incite a stronger immune response against HPV with the production of IL-1, IL-2, IL-4, IL-5 and TNF-α. IL-1 and TNF-α have been shown to have antiviral effects on HPV, through the down-regulation of its gene transcription. Various placebo-controlled studies assessing MMR have reported complete clearance in 67-79% cases along with side effects like pain, itching, erythema and flu-like symptoms.1
The use of topical immunotherapy could overcome these adverse events. Neither of our patients reported any signs of immediate/delayed hypersensitivity or side effects like erythema, burning, itching or urticaria (ruling our hypersensitivity cross-reaction to any growth media or preservative used in MMR vaccine). However, a subclinical reaction cannot be ruled out.
Although literature mentions that the rate of spontaneous clearance in warts is high in children, in adults the rates are much lower and may take up to 24 months.5 It was doubtful that such spontaneous clearance could have occurred during the short period of our patients’ observation and follow-up. Additionally, we only chose patients with no other treatment history, to ensure that the effect of topical MMR vaccine was not influenced by other therapies. We were unable to find any previous studies, reporting the effect of topical MMR vaccine as an immunogen. Though we found topical MMR vaccine to be effective while treating verruca plana with no recurrence or side-effects, our observations are meant merely for generating a hypothesis about its mechanism of action and further controlled studies are needed to reproduce these results.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Intralesional measles-mumps-rubella is associated with a higher complete response in cutaneous warts: A systematic review and meta-analysis of randomized controlled trial including GRADE qualification. J Dermatolog Treat [published online ahead of print, 2020 Jan 27]
- [Google Scholar]
- The efficacy and safety of intralesional immunotherapy with measles, mumps, rubella virus vaccine for the treatment of common warts in adults. Indian Dermatol Online J. 2019;10:19-26.
- [Google Scholar]
- Evolving role of immunotherapy in the treatment of refractory warts. Indian Dermatol Online J. 2016;7:364-70.
- [CrossRef] [PubMed] [Google Scholar]
- Immunotherapy in viral warts with intradermal Bacillus Calmette-Guerin vaccine versus intradermal tuberculin purified protein derivative: A double-blind, randomized controlled trial comparing effectiveness and safety in a tertiary care center in Eastern India. Indian J Dermatol Venereol Leprol. 2017;83:411.
- [CrossRef] [PubMed] [Google Scholar]
- An armamentarium of wart treatments. Clin Med Res. 2006;4:273-93.
- [CrossRef] [PubMed] [Google Scholar]





