Translate this page into:
Impact of combining photodynamic diagnosis with reflectance confocal microscopy, on tumor margin detection and surgical outcomes in patients with extramammary Paget disease
Corresponding author: Dr. Liang Zhao. Department of Dermatologic Surgery, Institute of Dermatology, Chinese Academy of Medical Sciences and Peking Union Medical College, Nanjing, Jiangsu, China. zhaoliang210042@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Cheng X, Zhang Q, Zhang W, Huang L, Sun J, Zhao L, et al. Impact of combining photodynamic diagnosis with reflectance confocal microscopy, on tumor margin detection and surgical outcomes in patients with extramammary Paget disease. Indian J Dermatol Venereol Leprol. 2024;90:447-52. doi: 10.25259/IJDVL_1011_2022
Abstract
Background
The recurrence rate of extramammary Paget disease after surgical resection is high due to the lesions' poorly delineated and unclear margins.
Aim
To evaluate the impact of non-invasive tumour margin detection via photodynamic diagnosis plus reflectance confocal microscopy on the surgical outcomes of patients with extramammary Paget disease.
Methods
Thirty-six patients with histopathologically confirmed primary extramammary Paget disease between January 2017 and June 2018 were included in this study. The skin lesion margins were preoperatively observed using the naked eye, photodynamic diagnosis, and reflectance confocal microscopy. An incision was made 0.5–2 cm from the outermost non-invasive detection marker line. The incision depth was more significant than the follicle level or the deepest level affected by the tumour in the biopsy specimens. After the skin lesions were removed, a pathological examination of the specimens was conducted to ensure clear margins to prevent tumour recurrence and metastases.
Results
A total of 166 good-quality tissue sections were selected from 36 patients. The tumour surfaces and deep margins were within the scope of resection. Six patients (6/36, 15.4%) experienced local recurrence 2–12 months postoperatively. One patient (1/36, 2.8%) had lymph node metastasis without local recurrence 36 months postoperatively and died 50 months postoperatively (1/36, 2.8%).
Limitations
This study is limited by the small patient population, especially the number of patients with mucous membrane involvement.
Conclusion
Using photodynamic diagnosis plus reflectance confocal microscopy to detect the margins of extramammary Paget disease lesions non-invasively reduces the postoperative tumour recurrence rate and is a valuable guide for tumour treatment.
Keywords
Extramammary Paget disease
photodynamic diagnosis
reflectance confocal microscopy
margin
surgery
Plain Language Summary
Extramammary Paget disease (EMPD) is a rare type of malignant skin tumour. Local expanded surgical resection remains the preferred treatment for patients with EMPD. However, the margins of EMPD and the depth of the tumour cell invasion are difficult to delineate in the clinic, leading to a recurrence rate of 20–60%. This study investigates the impact of non-invasive tumour margin detection via photodynamic diagnosis plus reflectance confocal microscopy on the surgical outcomes of patients with EMPD. The results showed that using photodynamic diagnosis plus reflectance confocal microscopy to detect the margins of EMPD lesions non-invasively could reduce the postoperative tumour recurrence rate and is a valuable guide for tumour treatment.
Introduction
Extramammary Paget disease (EMPD) is a rare type of malignant skin tumour. Although Mohs surgery can identify the tumour resection edges and preserve normal tissues, it is time-consuming, expensive, and requires the collaboration of specially-trained dermatologists and pathologists.1–3 Local expanded surgical resection remains the preferred treatment for patients with EMPD.4 However, the margins of EMPD and the depth of the tumour cell invasion are difficult to delineate in the clinic, leading to a 20–60% recurrence rate.5 This study investigates the impact of non-invasive tumour margin detection via photodynamic diagnosis plus reflectance confocal microscopy on the surgical outcomes of patients with EMPD.
Methods
A total of 36 patients who were histopathologically diagnosed with primary EMPD between January 2017 and June 2018 were included in this study. Patients with secondary EMPD, those in whom surgery was contraindicated, and those who refused surgery were excluded from the study. The appropriate ethics committee approved this study. Informed consent was obtained from all patients. This study was conducted according to the principles of the Declaration of Helsinki.
Photodynamic diagnosis and reflective confocal microscopy (Vivascope 1500, wavelength 830nm. Lucid Inc., Rochester, NY, USA) was used preoperatively to locate the lesion margins in all patients [Figures 1 and 2].6 The surgical resection line was marked by expanding 0.5–2.0 cm outward from the outermost, non-invasive detection marker line. The incision depth was greater than the level of the hair follicles or the deepest level affected by the tumour in the biopsy specimens. The surgeon determined the specific extension distance and resection depth.

- Lesion of EMPD showing infiltrative erythema on the pubic mound, the penis, and the scrotum.
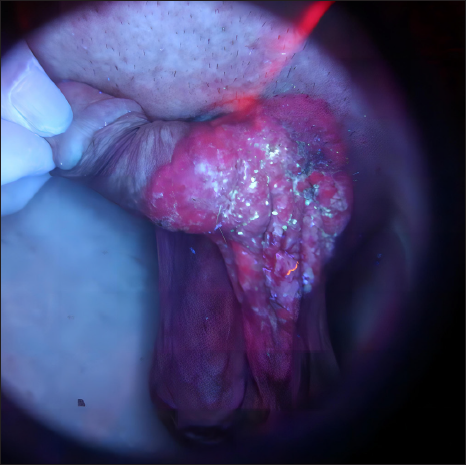
- Photodynamic diagnosis under Wood’s light with brick red fluorescence observed on the pubic mound, penile, and upper scrotum.
The lymph node position was probed and marked using B-mode ultrasound in patients undergoing sentinel lymph node biopsy. Nano carbon was injected 30 min preoperatively at the edge of the skin lesion.7,8 Under local, intravertebral, or general anaesthesia, the skin was cut at the regional lymph nodes, and the subcutaneous tissue was separated to detect the lymph nodes that were stained black. All stained lymph nodes were resected.
The epidermis was cut, using a scalpel, along the marker lines of the photodynamic diagnosis plus reflectance confocal microscopy, the photodynamic fluorescence diagnosis, and the clinical macroscopic skin lesion mark, which was considered as a marker during the histopathological examination [Figure 3]. A new scalpel was used each time a new epidermal marker line was excised. The skin lesion was resected along the surgical excision marker line [Figure 4]. A skin flap or graft was used to repair the wound [Figure 5]. The edges of each resected specimen were cut in one or two places according to different anatomical positions. If the skin lesion was located at the same anatomical site, four specimens were cut in the direction of 12, 3, 6, and 9 o’clock positions. The specimen was cut from the visible skin lesion to the surgical resection margin, including three marker lines visible to the naked eye and examined by photodynamic diagnosis and photodynamic diagnosis plus reflectance confocal microscopy, respectively. The width of the specimens was approximately 0.5 cm, and the specific resection site was recorded. A 1 × 0.5–1 cm section containing the full thickness of the specimen was removed from the thickest region at the centre of each specimen to verify the resection of the base of the tumour.

- After the lymph nodes of the left groin were resected, the surgical resection line was marked by expanding 0.6–0.7 cm outward from the marker line of the photodynamic diagnosis plus reflectance confocal microscopy. The epidermis was cut using a scalpel along the marker lines of the photodynamic diagnosis, reflectance confocal microscopy, and surgical resection. Coloured arrows: Yellow- photodynamic diagnosis plus reflectance confocal microscopy diagnostic line; Black- surgical resection line.

- After the surgical excision.

- A skin flap was used to repair the wound.
The positive rate of tumour cells at the edges or base of each specimen was determined. The distances between the tumour margin and the observed marker lines (determined using the naked eye, photodynamic diagnosis, and photodynamic diagnosis plus reflectance confocal microscopy) were noted. The distances between the tumour margin and the resection margin and between the base of the tumour and the deep resection margin were also noted.
Each patient was followed up for at least 1 year postoperatively [Figure 6]. Follow-up was conducted monthly for the first 3 months postoperatively, then every 2 months up to 1 year. After that, follow-up was performed every 3 months.

- One year later, no obvious abnormalities were seen in the surgical area.
Statistical analysis
Categorical data are expressed as numbers and percentages, and continuous data are described as mean, standard deviation, and median.
Results
A total of 32 men and 4 women (age range, 50–82 years) were included in the study. One patient had axillary lesions, 31 had genital lesions, and all 4 women had vulvar lesions. The disease course ranged from 4 months to 20 years. The area of the macroscopic skin lesions ranged from 0.5 cm × 1.0 cm to 11.4 cm × 15.7 cm. Preoperative histopathological examinations revealed that the tumour cells were limited to the epidermis and involved hair follicles, sweat glands, and other appendages in 23 patients. No obvious metastatic lesions were observed on computed tomography or B-mode ultrasound. The photodynamic diagnosis plus reflectance confocal microscopy lines overlapped with the naked eye or photodynamic lines or were the outermost lines in all patients. A total of 166 good-quality tissue sections were selected from 36 patients. The tumour surface status was observed in 130 specimens, and the deep tumour status was observed in 36 specimens.
Postoperative pathological examination
A total of 83 sections were outside the macroscopic line (false-negative rate, 63.8% [83/130]; mean distance outside the line, 3.5 ± 3.1 mm; median distance, 2.7 mm; and range, 0–14.6 mm). The remaining 47 sections were located within the macroscopic line. The histopathologic tumour margins of 27 sections were located outside the photodynamic diagnosis plus reflectance confocal microscopy lines (false-negative rate, 20.8% [27/130]; mean distance outside the line, 1.4 ± 1.2 mm; median distance, 0.9 mm; and range, 0.1–5.3 mm). The outer margin of the tumour was located within the cutting edge in 130 specimens. The mean distance from the outer margin of the tumour to the cutting edge was 8.9 ± 5.4 mm; the median distance was 7.7 mm, and the range was 0.3–30.2 mm. The base of the tumour was located within the deep resection edge in all 36 sections in which the base of the tumour was observed, including 14 obtained from the scrotum, 12 from the pubic mound, 4 from the penis, 2 from the labia majora, 1 from the lower abdomen, 1 from the vaginal orifice, 1 from the armpit, and 1 from the groin. The mean distance from the base of the tumour to the deep resection edge was 5.9 ± 2.6 mm; median distance, 5.9 mm; and range, 1.5–10.3 mm. The mean tumour thickness was 1.9 ± 2.1mm; median, 1.2 mm; and range, 0.1–6.5 mm. The mean thickness of the resected specimens was 7.8 ± 2.8 mm; median, 7.6 mm; and range, 2.2–14.4 mm.
The regional lymph nodes were swollen on B-mode ultrasound in all 36 patients. The lymph nodes ranged from 11.1 × 9.9 × 5.8 mm to 29.2 × 21.9 × 9.4 mm and were oval. The cortical and medullar structures were clear, with an aspect ratio > 1 and a blood flow resistance index < 0.7. Seventeen patients were selected to undergo sentinel lymph node biopsy in the groin, and 19 lymph nodes were excised. No tumour cells were detected in the pathology specimens.
Six patients had local tumour recurrence within 2–12 months postoperatively, including 4 males with original lesions at the scrotum and recurrent lesions at the incision margin. Two patients had initial and recurrent lesions at the vaginal orifice and labia minora. The scrotum was involved in 26 primary skin lesions and 4 recurrent lesions (15.4%). The labia minora involved 3 primary skin lesions and 1 recurrent lesion (33.3%). The vaginal orifice involved 1 primary skin lesion and 1 recurrent lesion (100%) [Table 1].
| Site | Number of tumours involved (cases) | Number of recurrences (cases) | Recurrence rate (%) |
|---|---|---|---|
| Scrotum | 26 | 4 | 15.4 |
| Penis | 25 | 0 | 0.0 |
| Pubic mound | 25 | 0 | 0.0 |
| Lower abdomen | 7 | 0 | 0.0 |
| Groin | 6 | 0 | 0.0 |
| Labia majora | 4 | 0 | 0.0 |
| Labia minora | 3 | 1 | 33.3 |
| Perineum | 3 | 0 | 0.0 |
| Vaginal orifice | 1 | 1 | 100.0 |
| Armpit | 1 | 0 | 0.0 |
Six patients had local tumour recurrence within 2–12 months postoperatively, including four males with original lesions at the scrotum who had recurrent lesions at the incision margin. Two patients had initial and recurrent lesions at the vaginal orifice and labia minora. The scrotum was involved in 26 primary skin lesions and four recurrent lesions (15.4%). The labia minora involved three primary skin lesions and one recurrent lesion (33.3%). The vaginal orifice was engaged in one primary skin lesion and one recurrent lesion (100%).
Discussion
An accurate and effective margin determination is essential in patients with extramammary Paget disease (EMPD) undergoing surgery, as unclear margins can lead to postoperative recurrence. The methods used in this study aimed to improve the surgical clearance of the tumour and reduce postoperative recurrence while achieving minimal trauma.
The photosensitiser in photodynamic fluorescence is absorbed by target cells and metabolised to porphyrin, which displays fluorescence under a specific wavelength of light. The fluorescence can identify a clear margin line between diseased and normal skin. Photodynamic fluorescence helps to determine the margins of EMPD lesions and is considered a breakthrough technique in diagnosing and treating tumours.9 Huang et al.10 identified a subclinical lesion of EMPD disease 3 cm from the dominant lesion using a combination of photodynamic diagnosis and reflectance confocal microscopy.
The Paget cells in EMPD present as atypical cells inside the epidermis with highly refractive, large-cell nuclei under reflectance confocal microscopy. Busam et al.11 reported that confocal scanning laser microscopy can help surgeons identify the margins of skin lesions, assess the surgical scope, and guide surgical resection. Tannous et al.12 emphasised that Mohs surgery relies on confocal scanning laser microscopy to guide skin tumour excision, maximise normal tissue sparing, and increase the cure rate. However, due to the structures of the reflectance confocal microscopy instruments and the small visual fields, it is challenging to examine large areas of uneven skin, such as that on the scrotum. Therefore, the detection procedure was simplified in this study by labelling the tumour margin to be visible to the naked eye and then performing the photodynamic fluorescence diagnosis in the area 5 cm from the macroscopic line. Therefore, reflectance confocal microscopy was used to detect the tumour margin along the photodynamic diagnostic marker line. This method may simplify the reflectance confocal microscopy detection process and requires less time than the traditional method.
Sufficient resection widths and depths are necessary during the removal of the tumour body, beneficial for clearing the body surface of tumours and invading deep damage such as glands, hair follicles, and other appendages. However, excessive expansion of the resection area can lead to the loss of a large amount of normal tissue, causing relatively severe surgical trauma, resulting in scars and functional limitations. Histopathological examinations are the gold standard for assessing the specimen edges. In this study, 130 tumour margin sections from 36 patients were postoperatively observed, and all tumour margins were determined to be within the resected area. Among 36 sections used to observe the deep tumour resection status, the tumour margins were all within the resection area. Among the 130 sections used to observe the tumour surface margin, 47 sections (36.2%) were within the marker line from direct observation, and 83 sections (63.8%) were outside this line. The furthest distance away from the marker line was 14.6 mm. Among these 83 sections, 46 (35.4%) had tumour margins outside the photodynamic diagnosis line (maximum distance, 5.9 mm). A total of 27 sections (20.8%) had tumour margins outside of the photodynamic diagnosis plus reflectance confocal microscopy lines (maximum distance, 5.3 mm). These results indicate that naked-eye observation, photodynamic diagnosis, and reflectance confocal microscopy do not accurately reflect actual tumour margins. Excisions made based on these marker lines may lead to inadequacies in surgical treatment. Therefore, the scope of resection should be extended by at least 6 mm from the outermost photodynamic diagnosis plus the reflectance confocal microscopy marker line. The resection depth should be greater than the level of the hair follicles or the deepest level affected by the tumour specimen.
The recurrence rate of EMPD is affected by subclinical lesions, multifocal incidence, and the depth of invasion.13 This study used photodynamic diagnosis plus reflectance confocal microscopy within a 5-cm margin around the tumour observed by the naked eye. This approach improved the probability of discovering subclinical lesions in a more extensive range and increased the surgical clearance rate. Six patients (6/36, 16.7%) experienced postoperative local recurrence within 12 months of surgery, including two recurrent lesions within 2 months. Therefore, the frequency of follow-up visits should be increased to identify residual lesions. Overall, recurrent lesions were detected in 15.4% of patients with scrotum lesions, 33.3% of patients with labia minora lesions, and 100% of patients with vaginal orifice lesions, indicating that recurrence rates are higher in regions with mucosal membranes. The presence of wrinkles and extensibility at the scrotal area, mucosal surfaces at the labia minora and vaginal orifice, atypical photodynamic fluorescence,10 difficulties in detection due to the mechanical arm of the desktop reflectance confocal microscope leading to incomplete detection, the lack of Mohs surgery in this study, or the lack of complete pathological examinations at the margins and base of the resected areas in this study may account for these findings.
O’Connor et al. treated 95 patients with surgery. At mean follow-up (wide excision, 65 months; Mohs surgery, 24 months), the disease had recurred in 18 of 83 (22%) patients who underwent standard wide excision, compared with the recurrence in 1 of 12 (8%) who had the Mohs micrographic excision.14 The recurrence rate in our study (6/36, 16.7%) was lower than that in the wide excision group and higher than that in the Mohs surgery group of the previously mentioned study. However, neither was statistically significant, probably related to the small sample size.
A total of 19 sentinel lymph nodes were biopsied in 17 patients, and no tumour cells were observed within the nodes, indicating that the lymph node metastasis was low. However, one male patient experienced left inguinal lymph node swelling 31 months postoperatively. At 36 months postoperatively, the lymph node had an abnormal shape and structure, and imaging findings suggested metastasis. The patient died 50 months postoperatively. Therefore, regional lymph nodes must be carefully monitored in these patients.
Limitations
This study was limited by the small patient population, especially the number of patients with lesions of mucosal membranes.
Conclusion
In conclusion, this study determined the effects of non-invasive methods to detect the margins of EMPD lesions. These methods are feasible and time-efficient. The tumour clearance rate and postoperative recurrence rate were acceptable. Therefore, these methods can be used in the surgical treatment of EMPD.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
1. National key research and development program (2022YFC2504700, 2022YFC2504701, 2022YFC2504705). 2. CAMS Innovation Fund for Medical Sciences (CIFMS, 2020-I2M-C&T-B-091).
Conflicts of interest
There are no conflicts of interest.
References
- Comparison of Mohs micrographic surgery and wide excision for extramammary Paget’s disease: Korean experience. Dermatol Surg. 2009;35:34-40.
- [CrossRef] [PubMed] [Google Scholar]
- Mohs micrographic surgery for extramammary Paget disease: a pooled analysis of individual patient data. J Am Acad Dermatol. 2013;68:632-637.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment and outcomes of patients with extramammary Paget disease. Dermatol Surg. 2017;43:708-714.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of extramammary Paget disease of the vulva with imiquimod: A retrospective, multicenter study by the German Colposcopy Network. J Am Acad Dermatol. 2014;70:644-50.
- [CrossRef] [PubMed] [Google Scholar]
- Extramammary Paget disease: Surgical treatment with Mohs micrographic surgery. J Am Acad Dermatol. 2004;51:767-73.
- [CrossRef] [PubMed] [Google Scholar]
- Utility of photodynamic diagnosis plus reflectance confocal microscopy in detecting the margins of extramammary Paget disease. Indian J Dermatol Venereol Leprol. 2021;87:207-213.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of sentinel lymph node detection by methylene blue and carbon nanoparticle suspension injection in early breast cancer. Zhonghua Zhong Liu Za Zhi. 2011;33:226-228. [Article in Chinese]
- [PubMed] [Google Scholar]
- Sentinel lymph node biopsy using carbon nanoparticles for Chinese patients with papillary thyroid microcarcinoma. Eur J Surg Oncol. 2012;38:718-724.
- [CrossRef] [PubMed] [Google Scholar]
- Fluorescence diagnostics as a guide for demarcation and biopsy of suspected anal cancer. Int J Dermatol. 2012;51:31-34.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of subclinical extramammary Paget’s disease with a combination of noninvasive photodynamic diagnosis and reflectance confocal microscopy. Indian J Dermatol Venereol Leprol. 2021;87:371-374.
- [CrossRef] [PubMed] [Google Scholar]
- Detection of clinically amelanotic malignant melanoma and assessment of its boundaries by in vivo confocal scanning laser microscopy. Arch Dermatol. 2001;137:923-929.
- [PubMed] [Google Scholar]
- In vivo real-time confocal reflectance microscopy: a noninvasive guide for Mohs micrographic surgery facilitated by aluminum chloride, an excellent contrast enhancer. Dermatol Surg. 2003;29:839-846.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical Treatment for Extramammary Paget's Disease. Curr Treat Options Oncol. 2018;19:27.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of mohs micrographic surgery and wide excision for extramammary Paget's disease. Dermatol Surg.. 2003;29:723-7.
- [CrossRef] [PubMed] [Google Scholar]






