Translate this page into:
Ingrown toenails
Correspondence Address:
Niti Khunger
Department of Dermatology and STD, VM Medical College and Safdarjang Hospital, Ring Road, New Delhi - 110 029
India
| How to cite this article: Khunger N, Kandhari R. Ingrown toenails. Indian J Dermatol Venereol Leprol 2012;78:279-289 |
Abstract
Onychocryptosis or ingrown toenail is a very common pathology of the toenail unit, chiefly affecting adolescents and young adults. The ingrown toenail is responsible for disabling complaints like pain and difficulty in walking. It is associated with significant morbidity, hampering the quality of life as it interferes with sporting activities, school, or work. It principally occurs in the hallux. It is ascribed to poor trimming of the nails in combination with local pressure due to ill-fitting footwear, hyperhidrosis, poor foot hygiene and nail abnormalities. Pain, swelling and discharge are the main clinical features. Four stages of the condition have been described. Diagnosis is usually evident, but it should be differentiated from subungual exostosis and tumors of the nail bed. The current standard of care focuses on conservative treatment like the gutter splint technique in the initial stages, and in cases that are resistant to medical management or recurrent, surgical correction is the treatment of choice. There are various surgical techniques that are described in literature. Although there is no ideal technique, lateral nail plate avulsion with lateral matricectomy by phenol is commonly used and reported to be more effective in reducing recurrences. The aim of this review article is to focus on this common pathology of the nail, the various techniques employed in management and aid in the selection of treatment according to the stage and severity of the disease.Introduction
Onychocryptosis (from Greek onyx nail and kryptos hidden) also known as ingrown toenail, or unguis incarnatus [1] is a common and painful form of nail disease. It is most common in teenagers and young adults during the second and third decades of life. The commonest symptom is pain in the affected nail which, if left untreated leads to infection, discharge and difficulty in walking, greatly hampering the quality of life of the individual. Diagnosis is apparent and several treatment approaches exist, ranging from a conservative medical approach to extensive surgical treatment options. The therapeutic approach chosen is dictated by the severity and stage of the ingrown toe nail.
Pathogenesis
The widely accepted theory is that onychocryptosis occurs when the lateral nail fold is penetrated by the edge of the nail plate, resulting in pain, sepsis and, later the formation of granulation tissue. [2] Penetration is often caused by spicules of nail at the edge of the nail plate, which incite an inflammatory response. The great toes are the most often affected. [3]
Various theories have been proposed to explain the aetiology of the ingrown toenail and they can be broadly classified according to whether the primary fault is the nail itself or the soft tissues at the side of the nail. [4],[5],[6] One theory is that the nail is not the real culprit, and it is actually the excess skin surrounding the nail which is the real problem. [6] The persons who develop this condition have an unusually wide area of tissue medial and lateral to the nail and that with weight bearing, this tissue tends to bulge up around the nail, leading to pressure necrosis. [6],[7] A prospective study by Pearson and colleagues [8] failed to demonstrate any abnormality of the nail in patients with symptomatic ingrown toenails, and suggested that treatment should not be based on the correction of a nonexistent nail deformity. Although it is still believed that the real defect lies in the nail, the controversy of whether there is a nail plate abnormality or overgrown nail folds still exists.
Predisposing Factors
Although an ingrown toenail can affect any age group, teenagers are usually most prone to the development of this abnormality. In adolescence, increased perspiration causing the nail fold to become soft and participation in sports result in the production of nail spicules, which can pierce the lateral skin fold of the nail apparatus. In older persons, spicule formation can be caused by reduced ability to care for their nails secondary to reduced mobility or impaired vision. In addition, the natural aging process causes toenails to thicken, making them more difficult to cut and more inclined to exert pressure on the lateral skin at the sides of the nail plate, often becoming ingrown, painful, and infected. [7] Particular nail shapes may be at greater risk of developing this problem. The condition is unilateral in 80% of cases and mostly affects the hallux. Usually males are more commonly affected.
The main factors implicated in the development of an ingrown toenail are as follows:
- Poorly fitting shoes: Extrinsic compression of the great toe by tight footwear and narrow shoes places constant pressure directly on the medial nail wall and indirectly on the lateral wall as the great toe is pushed against the second toe.
-
Improperly trimmed toenails: The toenails should be cut straight across, instead of rounded. [3] [Figure - 1]. Cutting the nail too short will allow more bulging of soft tissue leading to an inflammatory reaction and pressure necrosis. [7]
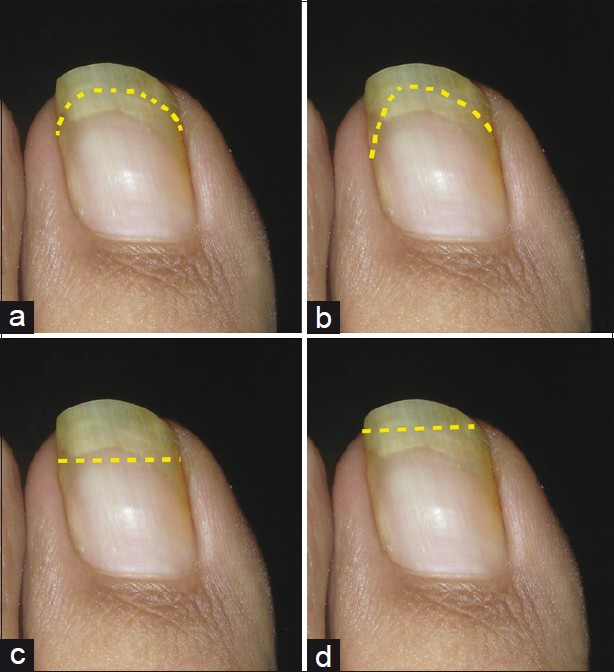
Figure 1: Correct method of trimming of toenails. (a) Improper-rounded. (b) Improper - V - shaped. (c) Improper - too short. (d) Proper - straight across beyond the nail bed - Excessive sweating: Excessive sweating and maceration causes the skin of the nail folds to become soft that can be easily penetrated by the nail.
- Nail infections: In tinea unguium or onychomycotic nails, the nail plate becomes brittle resulting in easy breaking off of nail spicules, making it easier for the nail to pierce the surrounding skin.
- Nail apparatus abnormalities: Improper shape of the nail plate, thick nail folds, medial rotation of the hallux (eversion) and reduced nail thickness can play a role in the development of the ingrown toenail. [7] A nail that is more curved from side to side rather than being flat is more likely to become an ingrown nail. The most severe type is called a ′pincer nail′.
- Others: Congenital onychocryptosis is an infrequent form of presentation, believed to be due to intrauterine trauma or hereditary transmission. [9],[10] Kinds of ingrown toenails during infancy include hypertrophy of the lateral nail folds, distal-lateral nail embedding, congenital malalignment of the great toenails and overcurvature of the nail plate. [11],[12] In some cases a genetic predisposition has been noted and familial cases have been reported. [13] Diabetic patients have been found to have a higher incidence of ingrown nails compared with nondiabetic patients. [14] Ingrown toenail and paronychia have been reported secondary to drugs, such as indinavir and indinavir/ritonavir combination. [15],[16] Excess nail fold granulation tissue and ingrown toenail have also been reported with retinoids, [17] docetaxel, [18] cyclosporine [19] and oral antifungal treatment. [20] Subungual neoplasms may cause ingrown toenails due to compression of the nail plate against the nail fold.
Clinical Features
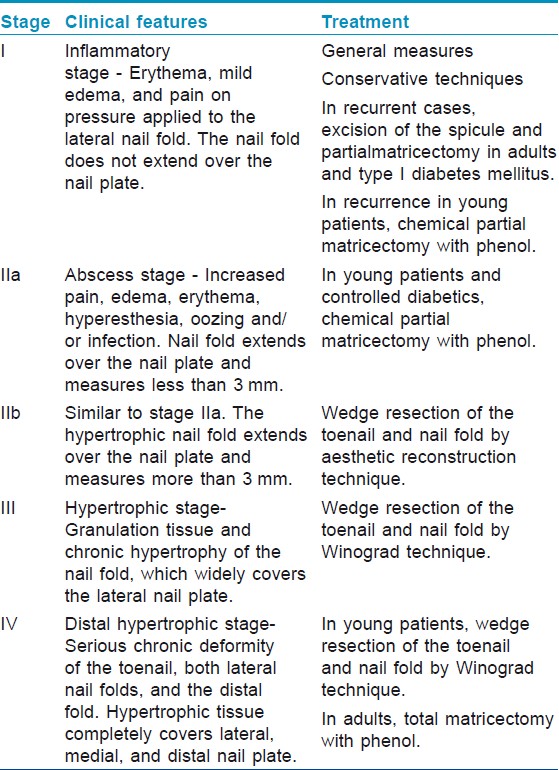
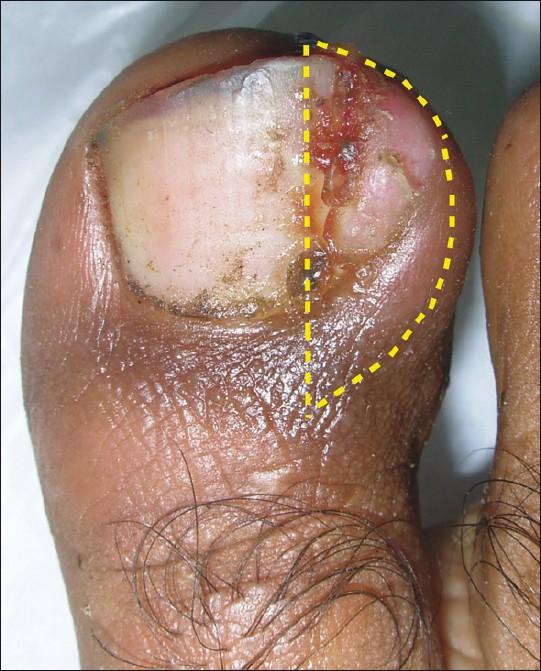
Initially, there is pain and redness, followed by swelling and pus formation. Granulation tissue then forms, increasing the compression, which adds to the swelling and discharge. A recent classification by Mozena [21] has described four stages of onychocryptosis [Figure - 2] and [Table - 1].
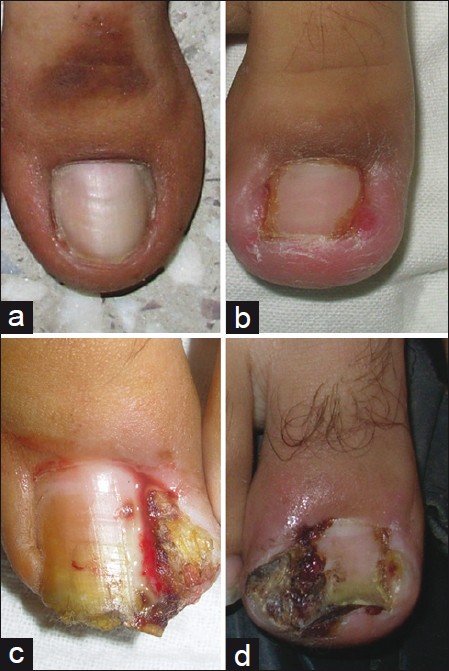 |
| Figure 2: Stages of ingrown toenails. (a) Stage I. (b) Stage IIa. (c) Stage IIb. (d) Stage III |
Diagnosis
Ingrown toenail is not difficult to diagnose. Differential diagnosis includes subungual exostosis, primary osteomyelitis of the phalanx and tumors of the nail bed, including subungual melanoma. Various other tumors, primary or metastatic, can mimic the presentation of an ingrown toenail. [22],[23]
Complications
Paronychia or secondary infection of the nail fold is common and can be caused by Staphylococcus, Psuedomonas, Candida, and superficial dermatophytes. It is important to treat any secondary infections resulting from or following ingrown toenails. Scarring of the nail fold and skin and rarely, cellulitis and osteomyelitis can occur. In diabetics, it may lead to amputations or life-threatening infections.
Treatment
There are various methods to treat ingrown toe nail. The selection of technique depends on the stage and severity of the condition, expertise of the surgeon and the previous treatment of the patient, in cases of recurrence. Mild to moderate lesions with minimal to moderate pain, little erythema and no purulent drainage can be treated with conservative therapies. Moderate to severe lesions with severe, disabling pain, substantial erythema and purulent drainage usually require surgical intervention.
Conservative treatment
Conservative therapy is a reasonable approach in patients with a mild to moderate ingrown toenail, although clinical trials proving its value do not exist. The advantage of conservative therapy is that it provides a cost-effective approach that obviates the need for a minor surgical procedure and its attendant short-term disability and pain. [24] There are various options which exist.
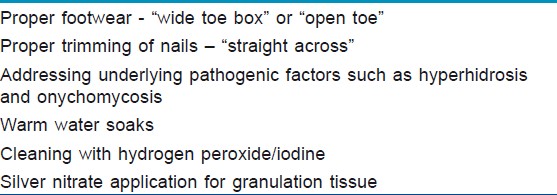
General measures
Proper footwear with a "wide toe box" or "open toe" should be adopted. The patient should be instructed to cut the nail straight across and avoid cutting back the lateral margins in a curved manner. The nail edge should extend past the tissue of the lateral nail fold. Underlying pathogenic factors such as hyperhidrosis, and onychomycosis should be managed. Soaking the affected toe and foot for 10 to 20 minutes in warm, soapy water, followed by a topical antibiotic ointment gives relief. Application of silver nitrate to the granulation tissue may decrease inflammation. Hydrogen peroxide and iodine can be used for cleaning, predominantly in stage I ingrown toenail [Table - 2].
Conservative techniques
1. Gutter splint or sleeve technique
A gutter splint is prepared by slitting a small appropriately cut sterilized vinyl intravenous drip infusion tube from top to bottom with one end cut diagonally for smooth insertion. Under local anesthesia, the lateral edge of the nail plate including the spicule is splinted with this lengthwise-incised flexible plastic tube. The splint is pushed proximally till the nail spicule is totally covered by the split plastic tube. The plastic tube is then attached with either adhesive tape, cyanoacrylate adhesive or wound closure strips [Figure - 3]. [24],[25],[26],[27] After splinting, patients experience instant relief of pain. They are instructed to wash the toe once daily with, povidone-iodine for up to 3 or 4 weeks. The splinted spicule grows out without injuring the nail fold and the granulation tissue subsides.
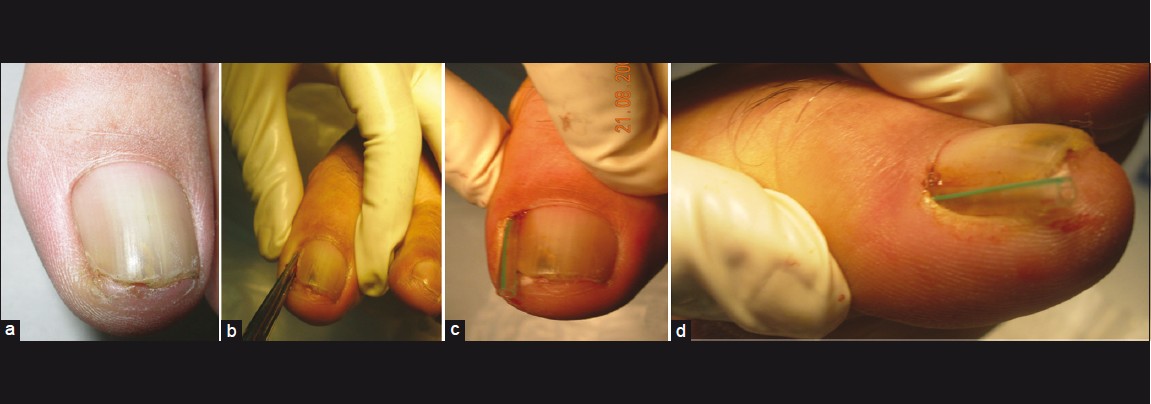 |
| Figure 3: Gutter splint or sleeve technique. (a) Ingrown toenail stage I. (b) Freeing the nail margin. (c) Insertion of vinyl IV tubing cut lengthwise. (d) Trimmed tube to let nail grow beyond the nail bed |
2. Cotton-wick insertion in the lateral groove corner
Wisps of cotton are placed under the ingrown lateral nail edge using a nail elevator or a small curette. A 79% rate of symptomatic improvement using cotton wisps over a mean follow-up period of 24 weeks was seen in an uncontrolled case series. [28]
3. Band-aid method[29]
One end of the tape is placed against the side ofthe ingrown toenail, along the granulation tissue, and the rest is twisted around the toe at an angle so that the other end overlaps the first, but does not cover the wound itself [Figure - 4]. The principle is that by physically pulling the side of the nail bed away from the nail, one can decrease pressure while simultaneously improving drainage of accumulated pus and drying of the wound. There are no controlled studies on this technique.
 |
| Figure 4: Band Aid® method of conservative treatment |
4. Dental floss technique
This noninvasive technique is used in the early stages of ingrown toenail. Without local anesthesia, a string of dental floss is inserted obliquely under the ingrown nail corner and pushed proximally. The lateral edge of the nail plate, including the spicule, is covered and separated with it. The technique is simple, easy to perform and is easily repeated by the patient, producing a fair chance of long-term remission from the ingrown toenail. [30]
5. Nail wiring
In this technique, two holes are made with 23-G needles at the distal free edge of the nailplate. An elastic wire is inserted until the degree of the nail plate becomes less than 60°. The wire is bent forward, cut with clippers, so that it does not protrude from the nail end and the small hole made by the needle is filled with an ethyl 2-cyanoacrylate adhesive agent [Figure - 5]. The elasticity of the wire helps in curing the deformity of the ingrown nail. It was reported in five patients with no recurrence 6 months after treatment. [31]
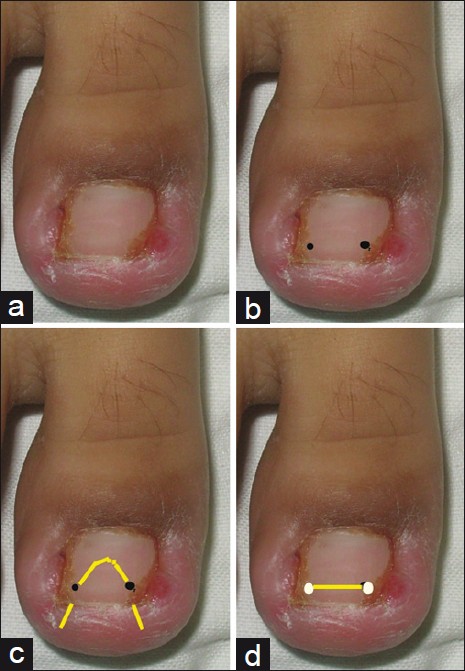 |
| Figure 5: Schematic diagram of nail wiring. (a) Ingrown toenail. (b) Two holes made with a 23 G needle at the sides of the nail plate. (c) Elastic wire inserted. (d) Elastic wire straightened, cut and fixed with cyanoacrylate adhesive |
6. Angle correction technique
The principle of this procedure is to correct the convexity of the nail by filing the whole surface of the nail, reducing its thickness by 50-75%. The procedure is repeated by the patient every 2 months, making the nail thin and soft. Recurrence was not seen in any of the eight patients at the end of 6 months. [32]
7. Others
Using an acrylic artificial nail [33] and a nail brace [34] are other conservative techniques that have been used.
Anesthesia for ingrown toenail surgery
Local anesthesia of the great toe should be performed cautiously to avoid vascular complications as toe necrosis has been reported as a rare serious complication of ingrown toenail surgery. [35] It has been suggested that metatarsal block is safer as compared to a digital block as collateral circulation is well developed, and the subcutaneous tissue is more expandable in the metatarsal area as compared to great toe [36] [Figure - 6]. A 2% lignocaine solution is preferable as a smaller volume is required. Contrary to popular belief, Krunic et al., [37] suggest that addition of epinephrine may reduce the need for a tourniquet and produce better and longer pain control during surgery.
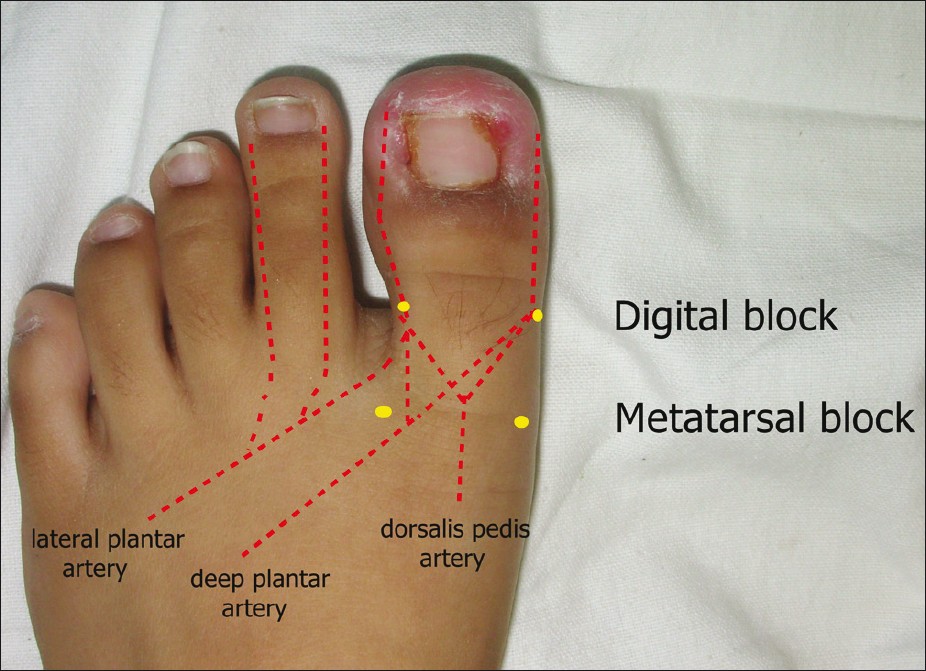 |
| Figure 6: Anesthesia for toenail surgery |
Surgical techniques
There are various surgical treatment options for ingrown toenails, although none of the techniques have been able to establish themselves as the technique of choice. The ideal surgical procedure should result in a high level of patient satisfaction, both functional and aesthetic, a rapid return to normal activities, and a low rate of recurrence. [38] Despite the lack of scientific evidence for the superiority of any one technique, many studies have shown greater success with the phenol-alcohol technique compared with other techniques. [5],[39],[40] Simple nail avulsion alone leads to high recurrence rates, up to 70%. [27],[41]
Excision of the spicule and partial matricectomy: Suppan I technique It is carried out in individuals with a Stage I ingrown toenail affecting the nail plate without hypertrophy of the nail fold and in adults or elderly patients, in whom tissue-regeneration capacity is reduced and likelihood of recurrence is lower. The technique consists of excision of the affected portion of the toenail and partial mechanical matricectomy (with curet or scalpel). Persichetti et al., [42] affirm that simple excision of the matrix using mechanical procedures is most effective, leading to fewer complications and infections and with a shorter healing time. Other studies, however, have found no significant differences between mechanical resection of the matrix and phenolization of the matrix, but discouraged the use of phenol as it is toxic. [43] Use of phenol for matricectomy can lead to tissue necrosis, pain and persistent exudative drainage post operatively. Rarely, systemic toxicity may ensue, due to longer duration of contact, which includes abdominal pain, dizziness, cyanosis, heamoglobinuria and cardiac arrhythmias.
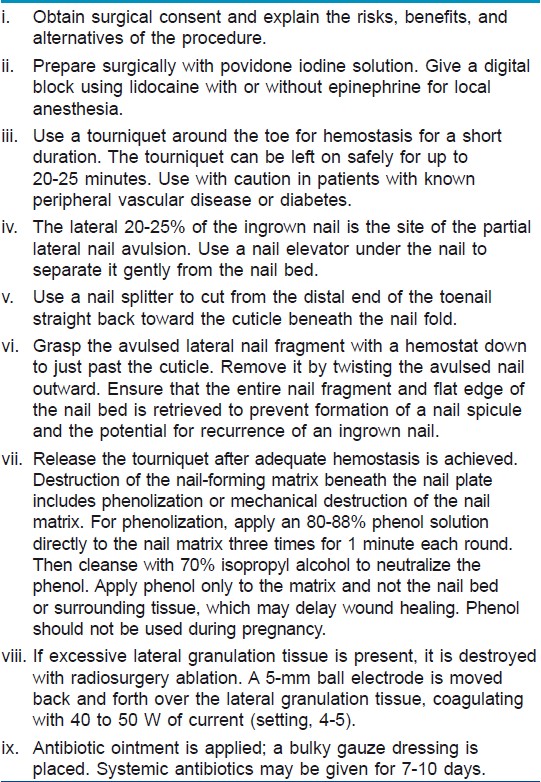
Chemical partial matricectomy: Phenol-Alcohol technique
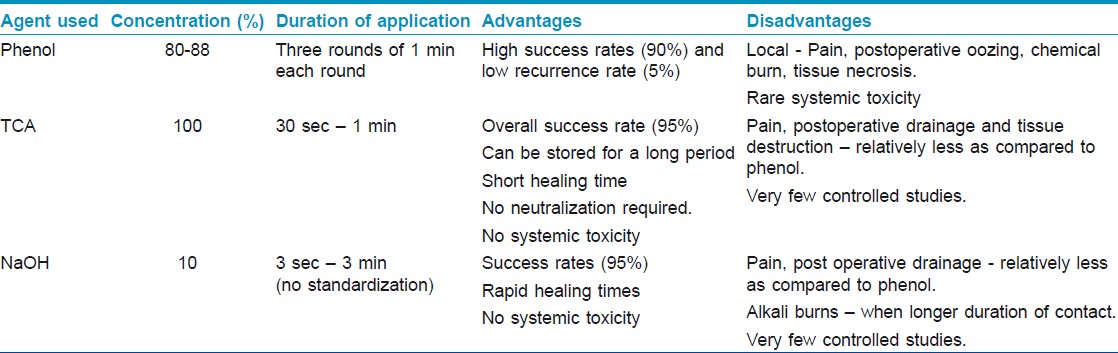
Phenolic ablation has a high success rate up to 90%. It is less painful, has a lower morbidity and has a higher success rate than surgical excision of the matrix. It is likely that there is some phenolic nerve damage at the site of surgery, which provides a degree of analgesia, but does not result in any long-term deficit. Indications for a phenolic ablation include stage I, stage IIa disease, young or adolescent patients because they have great tissue-regeneration capacity and diabetic patients with controlled type 1 or 2 diabetes. The phenol-alcohol technique is safe in diabetic patients who have no vascular risk and have good control of their diabetes. [38] Although there is no reported systemic side effects after phenol application for the treatment of ingrown nail, phenol application results in chemical burn and intense inflammatory changes. Though the recurrence rate is low (5%), post-operative complications like delayed healing and oozing are more common. [44] Oozing may continue for upto 6 weeks, although daily washing, potassium permanganate soaks or usage of 20% ferric chloride [45] will shorten this. The ooze is sometimes mistaken for infection and, although this can occur, it is rare. There is a single case reportwherein poor healing after chemical ablation unmasked significant vascular disease of the lower extremities in two patients. [46] The details of phenol-alcohol procedure are given in [Table - 3] [Figure - 7]. Studies comparing phenol applications of different durations revealed that 1-minute phenol cauterization of the germinal matrix has a better safety profile than prolonged applications in the treatment of ingrown nails. [47] According to a review of various surgical treatment modalities, phenolisation combined with avulsion of a nail is more effective thanmore invasive excisional surgical procedures to prevent symptomatic recurrence at six months or more (OR 0.44; 95% CI 0.24 to 0.80) 5 . The other agents that can be employed in chemical matricectomies are sodium hydroxide, [48],[49] and trichloroacetic acid [50] [Table - 4].
 |
| Figure 7: Treatment with phenol matricectomy. (a) ingrowing toenail Stage III. (b) frontal view showing granulation tissue and hypertrophy around the ingrowing nail plate. (c) Lateral nail plate avulsion with excision of granulation tissue. (d) Lateral chemical matricectomy with 88% phenol. (e) Neutralization of phenol with povidone-iodine alcohol solution. (f) Regrowth of a narrow nail without recurrence at 6 months |
Wedge resection of the toenail and nail fold
This procedure can be carried out via the aesthetic reconstruction technique [42] or the Winograd technique. [51] Both techniques are very similar and are indicated for stage IIb and stage III onychocryptosis [Figure - 8]. The techniques involve excision of the affected portion of the nail plate, partial matricectomy and wedge extirpation of the hypertrophic nail fold and the nail bed. Winograd′s technique is a type of wedge excision with more elaborate attention to the removal of the lateral matrix horn and better preservation of the lateral nail fold, whereas in an aesthetic reconstruction technique the aim is to reduce the convexity of the nail fold, with more attention given to the lateral nail fold. The aesthetic reconstruction technique involves complete removal of the nail plate and debridement of the granulomatous tissue, after which wedge-shaped ellipsis of skin and subcutaneous tissue, lateral to the affected nail fold, is removed. In a comparative study of 100 patients with ingrown toe nail, 50 were treated with the Winograd technique and 50 with the conservative sleeve or gutter splint method. Recurrence was observed in five (10%) patients who underwent sleeve surgery and six (12%) who underwent the Winograd technique. Postoperatively loss in work days was 2.0 weeks with Winograd technique and 1.1 weeks with gutter-splint method. These authors concluded that the sleeve method is more economical and appropriate for patients planning to go back to work soon. The sleeve method also resulted in greater matrix preservation and allowed regrowth of a normal nail with less signs of previous surgery, excellent cosmetic results and immediate pain relief. [52]
 |
| Figure 8: Wedge Resection of the toenail and nail fold |
Total matricectomy
This procedure is indicated for stage IV onychocryptosis in adult patients, onychogryphosis, onychodystrophy and chronic hypertrophy of the distal and lateral folds. Nail excision and total matricectomy with phenol is performed. [53],[54]
Alternative techniques
CO 2 laser, radiofrequency and electrocautery for matricectomy
CO 2 laser has been recommended as an effective primary modality of treatment with a success rate of 50-100%. [55] Well-established advantages of the CO 2 laser technique are less bleeding, reduced postoperative pain, immediate sterilization of infected tissue, and limited thermal damage to the surrounding tissues. [55],[56] Moreover, the possibility to selectively direct the laser beam into the deep recesses of the lateral horns of the matrix makes laser the therapeutic modality of choice. [57] The disadvantage is that re-epithelialization and healing of the tissues by secondary intention takes 3-6 weeks. The Er: YAG laser [58] radiofrequency ablation and electrocautery are other techniques employed for matricectomy.
Decompression technique
This procedure entails unilateral soft tissue resection of the nail fold combined with partial nail plate avulsion technique without permanent matricectomy. No permanent injury is incurred on the matrix, though recurrences are common. [59]
Soft-tissue nail fold excision technique
The procedure pioneered by Vandenbos and Bowers was based on the assumption that the nail is not the causative factor in development of the ingrown toenail. Chapeskie performed this procedure on over 560 patients with no recurrences. [6] This procedure does not touch the nail. After local anesthesia, the soft tissue enveloping the nail is excised widely in an elliptical manner. It is important that all the skin at the edge of the nail be removed. The wound is left open to close by secondary intention. Postoperative management involves soaking of the toe in warm water three times a day for 15-20 minutes. The wound heals by 4-6 weeks. The advantage of this technique is the preservation of the nail and its matrix, excellent cosmetic results, no recurrences and high rates of patient satisfaction. [60] Noel also reported excellent short-term results without recurrences in the 12 month follow-up period in 23 patients treated with soft tissue resection without matricectomy. [61] A major, although rare, postoperative complication that can occur following wide excision of soft tissue is a loss of cutaneous innervation.
Silicone gel sheets
This simple technique involves the excision of the one-quarter part of the lesional side of the nail plate without excising the granulation tissue. After 24 hours, the silicone gel sheet is placed on the granulation tissue and the exposed nail bed and bandaged loosely without applying any pressure. The silicone gel sheets are successful in reducing the thickness of the hypertrophic nail fold and prevent the recurrence of the condition during the regrowth of the nail plate. The advantage of the method is that it is not destructive to the nail matrix and the adjacent tissue. [62]
Role of antibiotics
Oral antibiotics are considered as an essential component in the treatment course of ingrown toenails. [63],[64] However, antibiotic necessity remains controversial. Some physicians feel that instituting oral antibiotics before performing a phenol matrixectomy or at the time of the phenol matrixectomy reduces the risk of developing further infection. [65] Other investigators have indicated that once the offending nail is removed, the localized infection will resolve without the need of antimicrobial agents. [66] Initial treatment with oral antibiotics may not decrease healing times and it may be responsible for the delay in the actual matricectomy, which further leads to prolonged healing times. Furthermore, there was not a significant difference in healing between groups that received concomitant antibiotics and matrixectomy compared with the group that received matrixectomy alone. [67] If at all antibiotics are considered, they must be efficacious against coagulase-negative staphylococcal species, specifically Staphylococcus epidermidis, which is the most commonly cultured pathogen in infected ingrown toenails. [68]
Postoperative care and analgesics
Typically post operative care includes, advising the patient to avoid wearing shoes for 3 days, [69] and to keep the leg elevated for 24-48 hours. The dressing can be removed by the patient on the day after the surgery and is followed by cleaning with betadine or epsom salt soaks for 10-15 minutes, twice daily for a week. Following the soaks the patient is advised to apply antibiotic ointment and a small bandage. Analgesic requirement depends upon the method used to treat the ingrown toenail; usually analgesics prescribed for 2-3 days are enough. The patient can resume work usually after 48 hours. The patient is called for follow-up after 1 week.
Prognosis
Whatever procedure is employed, recurrences can occur. The primary cause for recurrence following these procedures is ineffective or incomplete matrix eradication, and regrowth of keratin tissue, from the matrix as a nail or from the lateral horn as a spicule. The spicule is most commonly located at the junction of the proximal and lateral nail folds or in the lateral groove, and represents one of the most frequent forms of surgical failure. It may easily be treated by superficial keratolytics or by excision and phenolization under local anesthesia.
Simple nail avulsion alone has high recurrence rates (about 70%) and is not advocated. [41] Elliptical longitudinal wedge resection has a reported recurrence rate of 5-20%. [6] Chemical matricectomy with phenol, with a recurrence rate of 5% is a good option for the nonsurgically oriented dermatologist. [40] However, postoperative complications may be more frequently reported. Almost the same therapeuticresults have been obtained with laser matricectomy. Although the lowest recurrence rates with the best cosmetic outcome have been seen in soft tissue nail fold excision technique, it has not been widely reported.
Conclusions
The ingrown toenail continues to be a common source of morbidity worldwide and has a significant impact on the quality of life of an individual. Correct management of onychocryptosis requires identification of the stage and evaluation of the affected tissues [Figure - 9]. Nail surgery should be considered in cases of pain, recurrent onychocryptosis, surgical relapse, and failure of conservative treatment. It is important to select the surgical technique that is best suited to the patient′s particular clinical situation. The evidence suggests that simple nail avulsion combined with the use of phenol, is more effective at preventing symptomatic recurrence of ingrowing toenails, though with an increased risk of infection. Despite innumerable treatment options, ideal technique with a low recurrence rate, low downtime and high cosmetic acceptability is still to be elucidated.
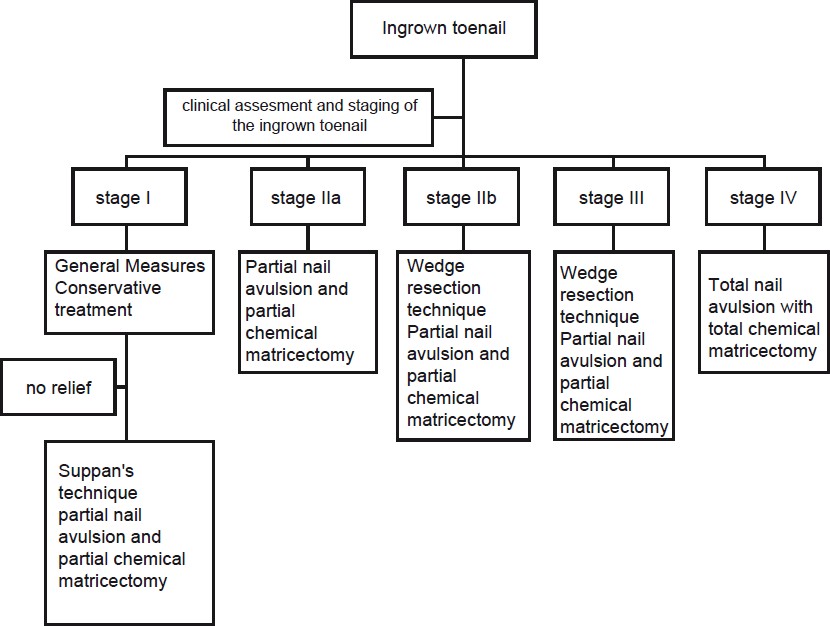 |
| Figure 9: Algorithm for treatment of ingrown toenail |
| 1. |
James WD, Berger T, Elston D. Diseases of the skin appendages. In: James WD, Berger T, Elston D, editors. Andrews' Diseases of the Skin: Clinical Dermatology. 10 th ed. Philadelphia, PA: Elsevier/Saunders; 2006. p. 749-93.
th ed. Philadelphia, PA: Elsevier/Saunders; 2006. p. 749-93.'>[Google Scholar]
|
| 2. |
Baran R, Haneke E, Richert B. Pincer nails: Definition and surgical treatment. Dermatol Surg 2001;27:261-6.
[Google Scholar]
|
| 3. |
De Berker DA, Baran R. Disorders of nails. In: Burns T, Breathnach SM, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 8 th ed. Oxford: Wiley-Blackwell; 2004. p. 65.1-65.54.
th ed. Oxford: Wiley-Blackwell; 2004. p. 65.1-65.54.'>[Google Scholar]
|
| 4. |
Lathrop RG. Ingrowing toenails: Causes and treatment. Cutis 1977;20:l19-22.
[Google Scholar]
|
| 5. |
Rounding C, Bloomfield S. Surgical treatments for ingrowing toenails. Cochrane Database Syst Rev 2005;2: CD001541.
[Google Scholar]
|
| 6. |
Chapeskie H. Ingrown toenail or overgrown toe skin? Alternative treatment for onychocryptosis. Can Fam Physician 2008;54:1561-2.
[Google Scholar]
|
| 7. |
Langford DT, Burke C, Robertson K. Risk factors in onychocryptosis. Br J Surg1989;76:45.
[Google Scholar]
|
| 8. |
Pearson HJ, Bury RN, Wapples J, Watkin DF. Ingrowing toenails: Is there a nail abnormality? A prospective study. J Bone Joint Surg Br 1987;69:840-2.
[Google Scholar]
|
| 9. |
Hendricks WM. Congenital ingrown toenails. Cutis 1979;24:393-4.
[Google Scholar]
|
| 10. |
Kreft B, Marsch WC, Wohlrab J. Congenital and post partum ungues incarnati. Hautarzt 2003;54 : 1083.
[Google Scholar]
|
| 11. |
Tosti A, Piraccini BM. Biology of nails and nail disorders. In: Wolff K, Goldsmith LA, Katz S, Gilchrest B, Paller A, Leffell D, editors. Fitzpatrick's Dermatology in General Medicine. 7 th ed. New York: McGrawHill; 2007. p. 778-94.
th ed. New York: McGrawHill; 2007. p. 778-94.'>[Google Scholar]
|
| 12. |
Katz A. Congenital ingrown toenails. J Am Acad Dermatol 1996;34:519-20.
[Google Scholar]
|
| 13. |
Cambiaghi S, Pistritto G, Gelmetti C. Congenital hypertrophy of the lateral nail folds of the hallux in twins. Br J Dermatol 1997;136:635-6.
[Google Scholar]
|
| 14. |
Riviera A. Risk factors for amputation in diabetic patients: A case controlled study. Arch Med Res 1998;29:179-84.
[Google Scholar]
|
| 15. |
James CW, McNelis KC, Cohen DM, Szabo S, Bincsik AK. Recurrent ingrown toenails secondary to indinavir/ritonavir combination therapy. Ann Pharmacother 2001;35:881-4.
[Google Scholar]
|
| 16. |
Bourezane Y, Thalamy B, Viel JF, Bardonnet K, Drobacheff C, Gil H, et al. Ingrown toenail and indinavir: A case control study demonstrates strong relationship. AIDS 1999;22:2181-2.
[Google Scholar]
|
| 17. |
Baran R. Retinoids and the nails. J Dermatol Treat 1990;1:151-4.
[Google Scholar]
|
| 18. |
Nicolopoulos J, Howard A. Docetaxel- induced nail dystrophy. Australas J Dermatol 2002;43:293-6.
[Google Scholar]
|
| 19. |
Higgins EM, Hughes JR, Snowden S, Pembroke AC. Cyclosporin-induced periungual granulation tissue. Br J Dermatol 1995;132:829-30.
[Google Scholar]
|
| 20. |
Weaver T, Jespersen D. Multiple onychocryptosis following treatment of onychomycosis with oral terbinefine. Cutis 2000;66:211-2.
[Google Scholar]
|
| 21. |
Mozena JD. The Mozena Classification System and treatment algorithm for ingrown hallux nails. J Am Podiatr Med Assoc 2002;92:131-5.
[Google Scholar]
|
| 22. |
Goldenhersh M, Prus D, Ron N. Merkel cell tumour masquerading as granulation tissue on a teenager's toe. Am J Dermatopathol 1992;14:560-3.
[Google Scholar]
|
| 23. |
Lemont H, Brady J. Amelanoticmelanoma masquerading as an ingrown toenail. J Am Podiatr Med Assoc 2002;92:306-7.
[Google Scholar]
|
| 24. |
HeidelbaughJJ, Lee H. Management of the ingrown toenail. Am Fam Physician 2009;79:303-8.
[Google Scholar]
|
| 25. |
Wallace WA, Milne DD, Andrew T. Gutter treatment for ingrowing toenails. Br Med J 1979;2:168-71.
[Google Scholar]
|
| 26. |
Schulte KW, Neumann JN, Ruzicka T. Surgical Pearl: Nail splinting by flexible tube-Anew noninvasive treatment for ingrown toenails. J Am Acad Dermatol 1998;39:629-30.
[Google Scholar]
|
| 27. |
Gupta S, Sahoo B, Kumar B. Treating ingrown toenails by nailsplinting with a flexible tube: An Indian experience. J Dermatol 2001;28:485-9.
[Google Scholar]
|
| 28. |
Senapati A. Conservative outpatient management of ingrowing toenails. J R Soc Med 1986;79:339-40.
[Google Scholar]
|
| 29. |
Manca D. Taping toes-Effective treatment for ingrown toenails. Can Fam Physician 1998;44:275.
[Google Scholar]
|
| 30. |
Woo SH, Kim IH. Surgical Pearl: Nail edge separation with dental floss for ingrown toenails. J Am Acad Dermatol 2004;50:939-40.
[Google Scholar]
|
| 31. |
Moriue T, Yoneda K, Moriue J, Matsuoka Y, Nakai K, Yokoi I, et al. A simple therapeutic strategy with super elastic wire for ingrown toenails. Dermatol Surg 2008;34:1729-32.
[Google Scholar]
|
| 32. |
Ozdil B, Eray IC. New method alternative to surgery for ingrown nail: Angle correction technique. Dermatol Surg 2009;35:990-2.
[Google Scholar]
|
| 33. |
Arai H, Arai T, Nakajima H, Haneke E. Formable acrylic treatment for ingrowing nail with gutter splint and sculptured nail. Int J Dermatol 2004;43:759-65.
[Google Scholar]
|
| 34. |
Erdogan FG, Erdogan G. Long-term results of nail brace application in diabetic patients with ingrown nails. Dermatol Surg 2008;34:84-7.
[Google Scholar]
|
| 35. |
Rueff N, Gapany C. A rare ischemic complication of ingrowing toenail surgery in a child. Dermatol Surg 2009;36:250-2.
[Google Scholar]
|
| 36. |
Noel B. Anesthesia for ingrowing toenail surgery. Dermatol Surg 2010;36:1356-7.
[Google Scholar]
|
| 37. |
Krunic AL, Wang LC, Soltani K, Weitzul S, Taylor RS. Digital anesthesia with epinephrine: An old myth revisited. J Am Acad Dermatol 2004;51:755-9.
[Google Scholar]
|
| 38. |
Martínez-Nova A, Sánchez-Rodríguez R, Alonso-Peña D. A new onychocryptosis classification and treatment plan. J Am Podiatr Med Assoc 2007;97:389-93.
[Google Scholar]
|
| 39. |
Bostanci S, Ekmekcic P, Gurgey E. Chemical matricectomy with phenol for the treatment of ingrowing toenail: A review of literature and a follow up of 172 treated patients. Acta Derm Venereol 2001;81:181-3.
[Google Scholar]
|
| 40. |
Andreassi A, Grimaldi L, D'Anello C, Pianigiani E, Bilenchi R. Segmental phenolization for the treatment of ingrowing toenails: A review of 6 years experience. J Dermatologic Treat 2004;15:179-81.
[Google Scholar]
|
| 41. |
Palmer BV, Jones A. Ingrowing toenails: The results of treatment. Br J Surg 1979;66:575.
[Google Scholar]
|
| 42. |
Persichetti P, Simone P, Livecchi G, Di Lella F, Cagli B, Marangi GF. Wedge excision of the nail fold in the treatment of ingrown toenail. Ann Plast Surg 2004;52:617-20.
[Google Scholar]
|
| 43. |
Gerritsma-Bleeker CL, Klaase JM, Geelkerken RH, Hermans J, van Det RJ. Partial matrix excision or segmental phenolization for ingrowing toenails. Arch Surg 2002;137:320-5.
[Google Scholar]
|
| 44. |
Moossavi M, Scher RK. Complications of nail surgery: A review of the literature. Dermatol Surg 2001;27:225-8.
[Google Scholar]
|
| 45. |
Aksakal AB, Atahan C, Oztaº P, Oruk S. Minimizing postoperative drainage with 20% ferric chloride after chemical matricectomy with phenol. Dermatol Surg 2001;27:158-60.
[Google Scholar]
|
| 46. |
Toybenshlak M, Elishoov O, London E, Akopnick I, Leibner DE. Major complications of minor surgery. J Bone Joint Surg Br 2005;87:1681-3.
[Google Scholar]
|
| 47. |
Tatlican S, Yamangokturk B, Eren C, Eskioglu F, Adiyaman S. Comparison of phenol applications of different durations for the cauterization of the germinal matrix: An efficacy and safety study. Acta Orthop Traumatol Turc 2009;43:298-302.
[Google Scholar]
|
| 48. |
Ozdemir E, Bostanci S, Ekmekci P, Gurgey E. Chemical matricectomy with 10% sodium hydroxide for the treatment of ingrowing toenails. Dermatol Surg 2004;30:26-31.
[Google Scholar]
|
| 49. |
Tatlican S, Eren C, Yamangokturk B, Eskioglu F, Bostanci S. Chemical matricectomy with 10% sodium hydroxide for the treatment of ingrown toenails in people with diabetes. Dermatol Surg 2010;36:219-22.
[Google Scholar]
|
| 50. |
Kim SH, Ko HC, Oh CK, Kwon KS, Kim MB. Trichloroacetic acid matricectomy in the treatment of ingrowing toenails. Dermatol Surg 2009;35:973-9.
[Google Scholar]
|
| 51. |
Winograd AM. Modification in the technique of operation for ingrown toe-nail.1929. J Am Podiatric Med Assoc 2007;97:274-7.
[Google Scholar]
|
| 52. |
Peyvandi H, Robati RM, Yegane RA, Hajinasrollah E, Toossi P, Peyvandi AA, et al. Comparison of two surgical methods (winograd and sleeve method) in the treatment of ingrown toenail. Dermatol Surg 2011;37:331-5.
[Google Scholar]
|
| 53. |
De Berker DA, Dahl MG, Comaish JS, Lawrence CM. Nail surgery: An assessment of indications and outcome. Acta Derm Venereol 1996;76:484-7.
[Google Scholar]
|
| 54. |
Boyce S, Huang CC. Surgical Pearl: Hemostat-assisted nail avulsion revisited. J Am Acad Dermatol 2001;45:943-4.
[Google Scholar]
|
| 55. |
Andre P. Ingrowing nails and carbon dioxide laser surgery. J Eur Acad Dermatol Venereol 2003;17:288-90.
[Google Scholar]
|
| 56. |
Lin YC, Su HY. A surgical approach to ingrown nail: Partial matricectomy using CO2 laser. DermatolSurg 2002;28:578-80.
[Google Scholar]
|
| 57. |
Leshin B, Whitaker DC. Carbon dioxide laser matricectomy. J Dermatol Surg Oncol 1988;14:608-11.
[Google Scholar]
|
| 58. |
Wollina U. Modified Emmet's operation for ingrown nails using the Er: YAG laser. J Cosmet Laser Ther 2004;6:38-40.
[Google Scholar]
|
| 59. |
Aksakal AB, Oztas P, Atahan C, Gurer MA. Decompression for the management of onychocryptosis. J Dermatolog Treat 2004;15:108-11.
[Google Scholar]
|
| 60. |
Chapeskie H, Kovac JR. Soft-tissue nail-fold excision: A definitive treatment for ingrown toenails. Can J Surg 2010;53:282-6.
[Google Scholar]
|
| 61. |
Noel B. Surgical Treatment of Ingrown Toenail without Matricectomy. Dermatol Surg 2008;34:79-83.
[Google Scholar]
|
| 62. |
Aksakal AB, O'zsoy E, Gurer MA. Silicone gel sheeting for the management and prevention of onychocryptosis. Dermatol Surg 2003;29:261-4.
[Google Scholar]
|
| 63. |
Monheit GD. Nail surgery. Dermatol Clin 1985;3:521-30.
[Google Scholar]
|
| 64. |
Brown FC. Chemocautery of ingrown toenails. J Dermatol Surg Oncol 1981;7:331-3.
[Google Scholar]
|
| 65. |
Eisele SA. Conditions of the toenails. Orthop Clin North Am 1994;25:183-8.
[Google Scholar]
|
| 66. |
Burzotta JL, Turri RM, Tsouris J. Phenol and alcohol chemical matrixectomy. Clin Podiatr Med Surg 1989;6:453-67.
[Google Scholar]
|
| 67. |
Reyzelman MA, Trombello AK, Vayser DJ, Armstrong DG, Harkless BL. Are antibiotics necessary in the treatment of locally infected ingrown toenails? Arch Fam Med 2000;9:930-2.
[Google Scholar]
|
| 68. |
Wolf EW, Hodge W, Spielfogel WD. Periungual bacterial flora in humanfoot. J Foot Surg 1991;30:253-63.
[Google Scholar]
|
| 69. |
Ogur R, Tekbas OF, Hasde M. Managing infected ingrown toenails: Longitudinal band method. Can Fam Physician 2005;51:207-8.
[Google Scholar]
|
Fulltext Views
50,666
PDF downloads
10,348





