Translate this page into:
Insight into pediatric-versus adult-onset lichen planus: A retrospective analytical study from Northern India
Corresponding author: Dr. Deepika Pandhi, Department of Dermatology and STD, University College of Medical Sciences and GTB Hospital, University of Delhi, New Delhi, India. pandhi.deepika@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Daulatabad D, Pandhi D, Bhattacharya SN, Deuri D, Singal A, Malhotra RK. Insight into pediatric-versus adult-onset lichen planus: A retrospective analytical study from North India. Indian J Dermatol Venereol Leprol 2022;88:112-4.
Sir,
Lichen planus, the prototype of the group of inflammatory dermatoses with characteristic clinical and histopathological features,1 has an overall estimated prevalence of 0.22–5% worldwide.2 The prevalence is considered to be lesser in children (1–4% of the adult cases) but this has been refuted by many large series, most of which represent children of Asian, Indian and African origin.3,4 We present the data from a retrospective analytical study conducted in the Department of Dermatology, University College of Medical Sciences and Guru Teg Bahadur Hospital, an urban-based tertiary care center located in North India. In the study, records of all the patients diagnosed as lichen planus from January 1996 to May 2018 were retrieved and analyzed. This study focuses on the differences between pediatric onset and adult-onset lichen planus.
The patients were clinically diagnosed independently by two dermatologists and a histological confirmation was done when in doubt. Incomplete records were excluded from the study. The data were divided into two groups, pediatric onset (Group A, onset before 18 years of age) and adult onset (Group B, onset at or after 18 years of age). The primary diagnosis was as per the predominant type of lichen planus. Likewise, the primary diagnosis of oral, nail or genital lichen planus was made when they, respectively, were the main feature or the only site of involvement. otherwise, they were documented as lichen planus with oral, nail or genital involvement, respectively. The principles outlined in the Declaration of Helsinki were followed, patient’s consent was not required as the patient identity was not revealed or compromised. The data were analyzed using SPSS version 17, qualitative variables were tested between the groups using chi square and Fisher’s exact test and quantitative variables were using unpaired Student’s t test (level of significance: P<0.05).
The data of 1872 patients were included for analysis, of these 519 (27.7%) had pediatric onset (Group A) and 1353 (72.3%) had adult-onset disease (Group B). This shows that every fourth patient had a childhood onset disease. No gender predilection was observed in Group A. The demographic details of the study population are depicted in Table 1. Table 2 depicts the proportion of different types of lichen planus diagnosed. The presence of more than one morphological type was common to both the groups, especially cutaneous with mucosal lesion (oral involvement being the commonest). Table 3 depicts the differential clinical presentation in the two groups. Eruptive lichen planus, blaschko-linear involvement, generalized distribution and nail findings such as trachyonychia and nail dystrophy were more common in pediatric-onset group whereas oral and genital lesions were more common in the adult-onset subset. The most common oral lesions were of reticulate pattern and most common genital lesions observed were papules and plaques. Concurrent involvement of both oral and genital mucosa was also documented.
| Parameter | Group A; n=519 mean±SD* (range) | Group B; n=1353 mean±SD* (range) |
|---|---|---|
| Age (years) | 12.97±4.63 (2–37) | 38.56±13.76 (18–90) |
| Age at onset (years) | 11.64±4.27 (0–17.96) | 37.02±13.46 (18–88.5) |
| Duration (months) | 18.88±33.32 (0.5–240) | 20.14±37.04 (0.25–360) |
| Gender | M:F=259:260 | M:F=597:756 |
| Sex ratio | M:F=1:1 | M:F=1:1.27 |
| Diagnosis | Group A n=518(%) | Group B n=1351(%) | P-value |
|---|---|---|---|
| Classic LP | 266 (51.35) | 651 (48.19) | 0.221 |
| Oral LP | 56 (10.81) | 309 (22.87) | 0.000* |
| LP hypertrophicus | 62 (11.97) | 138 (10.21) | 0.272 |
| LP pigmentosus | 44 (8.49) | 110 (8.14) | 0.804 |
| LP pilaris | 39 (7.53) | 99 (7.33) | 0.882 |
| Nail LP | 29 (5.6) | 59 (4.37) | 0.261 |
| Eruptive LP | 37 (7.14) | 38 (2.81) | 0.000* |
| LP actinicus | 8 (1.54) | 43 (3.18) | 0.052 |
| Genital LP | 3 (0.58) | 45 (3.33) | 0.001* |
| Blaschko-linear LP | 10 (1.99) | 9 (0.68) | 0.033* |
| Annular LP | 3 (0.58) | 15 (1.11) | 0.293 |
| Follicular LP | 7 (1.35) | 9 (0.67) | 0.15 |
| LP atrophicus | 2 (0.39) | 9 (0.67) | 0.479 |
| Lichenoid dermatitis | 1 (0.19) | 5 (0.37) | 0.166 |
| Bullous LP | 1 (0.19) | 2 (0.15) | 0.381 |
| Subjects with more than one type of LP | 75 (14.48) | 206 (15.25) | 0.480 |
| Findings | Group A n=518(%) |
Group B n=1351(%) |
P-value |
|---|---|---|---|
| Generalized distribution | 113 (22.51) | 197 (14.94) | 0.000* |
| Blaschko-linear distribution | 10 (1.99) | 9 (0.68) | 0.033* |
| Eruptive LP | 37 (7.14) | 38 (2.81) | 0.000* |
| Leukonychia | 7/77 (9.09) | 2/192 (1.04) | 0.001* |
| TND/trachyonychia | 6/77 (7.79) | 3/192 (1.56) | 0.002* |
| Complete nail dystrophy | 7/77 (9.09) | 5/192 (2.60) | 0.017* |
| Longitudinal melanonychia | 6/77 (7.79) | 38/192 (19.79) | 0.035* |
| Presence of oral lesions | 129 (24.90) | 556 (41.31) | 0.000* |
| Presence of genital lesions | 16 (3.08) | 82 (6.07) | 0.002* |
Nail involvement was similar in both groups (Group A: 77 (14.9%) and Group B: 192 (14.2%); P = 0.586). The most common nail changes were longitudinal striation, longitudinal melanonychia and thinning and less common were pterygium, onychoschizia, onychorrhexis and total dystrophy. Twenty nail dystrophy was observed in six children and three adults, one each child had associated vitiligo and lichen striatus.
The associated immune-mediated disorders included vitiligo in 16 (eight in each group), urticaria in five (one in Group A), hypothyroidism in three (all were in Group B), alopecia areata in nine (seven in Group A), lichen nitidus in five (two in Group A) and lichen striatus in one (Group A) of the patients.
The treatment data were available for a total of 1296 adults and 500 children and are summarized in Figure 1. The most common modality of treatment used was topical corticosteroids, steroid-induced atrophy and perilesional hypopigmentation was the major adverse effect thereof. Oral lesions were treated mainly with tretinoin gel.
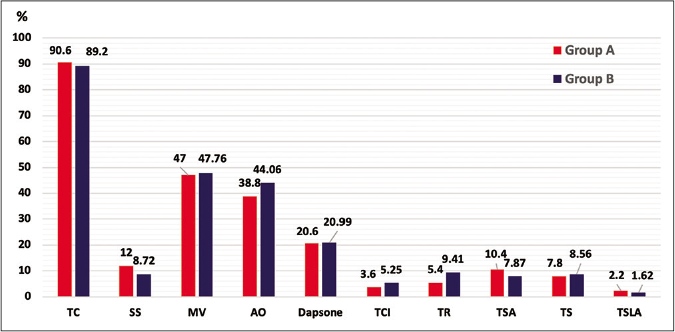
- Bar graph depicting the treatment offered to subjects in both the groups. The X-axis represents the therapeutic modalities used and the Y-axis represents the percentage of subjects who received the particular treatment option. Red- and blue-colored bars represent Groups A and B, respectively. TC: Topical corticosteroids, SS: Systemic steroids (inclusive of oral mini pulse – betamethasone, daily oral steroids – prednisolone and injectable steroids – triamcinolone acetonide), MV: Multivitamins – Vitamin A, C and E, AO: Antioxidants – selenium, glutathione, etc.; TCI: Topical calcineurin inhibitors – tacrolimus 0.03%, 0.1% gel and cream, pimecrolimus 1% cream, TR: Topical retinoids – tretinoin 0.025%, 0.05% gel and cream, TSA: Topical salicylic acid, TS: Topical sunscreen, TSLA: Topical skin lightening agents
Systemic treatment options were reserved for eruptive or rapidly progressive disease, erosive oral or genital disease and disfiguring and/or scarring nail or hair disease. Good response with short courses of daily oral steroids (0.5–1 mg/kg, tapered off over eight to 12 weeks) was evident, followed by either dapsone (one to two milligram/ kilogram, over three to 12 months) or oral mini pulse (OMP, 0.1 mg/kg betamethasone or dexamethasone per day on two consecutive days in the week) for maintenance. In the mini pulse group, hypertrichosis was observed in one individual. Intralesional steroids (triamcinolone acetonide) were given mainly in lichen planus hypertrophicus (5– 20 mg/ml) and intramatricially in nail lichen planus (five to ten milligram/milliliter) 4–6 weekly. In an exceptional case, it was administered for hypertrophic genital lesion with intractable pruritus which was non-responsive to topical steroids and topical calcineurin inhibitors. Dapsone-induced adverse reactions (deranged liver enzymes in five patients out of whom three were children, anemia in ten patients out of whom six were children, one patient developed fixed drug eruption and another extensive toxic epidermal necrolysis) were observed in 17 patients that warranted discontinuation of dapsone. Less often used drugs were acitretin, metronidazole, tetracyclines, chloroquine, hydroxychloroquine, methotrexate and levamisole. Follow-up data, as of at least one visit after diagnosis confirmation, were available for 709 patients (52.4%) in Group B and 281 patients (54.1%) in Group A. Among these, 513 (72.4%) in Group B and 216 (76.9%) in Group A noticed improvement. Further, 126 (17.8%) in Group B and 39 (13.9%) in Group A observed no change while the rest reported worsening. Post-inflammatory hyperpigmentation was the most common sequel in both the groups.
In our series, we observed concomitant occurrence of different clinical types of lichen planus, for example, classic lichen planus with hypertrophic lesions, lichen planopilaris, mucosal lichen planus or blaschko-linear lesions. The individual disease types manifested themselves mostly independent of the other types and followed their own course. This aspect of coexistence of different morphologies has been neglected so far and we would like to forward the term “multifocal lichen planus,” for this entity. The management for such cases was decided as per the site affected, except in cases where systemic treatment was warranted.
The major distinction of this study is that it is the largest series of lichen planus reported till now, whereas retrospective study design and lack of adequate follow-up are the drawbacks of the study. The study tries to analyse the features of children and adults who presented with lichen planus to our setup during the defined time period. As both the sections of subjects are derived from the same population pool, it is meaningful to draw conclusions with respect to the variations observed in both groups.
Declaration of patient consent
The patient's consent is not required as the patient's identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Cutaneous and mucosal lichen planus: A comprehensive review of clinical subtypes, risk factors, diagnosis, and prognosis. Scientific World Journal. 2014;30:742826.
- [CrossRef] [PubMed] [Google Scholar]
- Lichen planus in childhood: A series of 316 patients. Pediatr Dermatol. 2014;31:59-67.
- [CrossRef] [PubMed] [Google Scholar]
- Lichen planus in childhood: Report of 100 cases. Clin Exp Dermatol. 2010;35:257-62.
- [CrossRef] [PubMed] [Google Scholar]





