Intense pulsed light versus pulsed dye laser in the treatment of nail psoriasis: Intra-patient left to right comparative controlled study
Corresponding author: Dr. Shaimaa Ismail Omar, Department of Dermatology, Venereology and Andrology, Alexandria University, Alexandria, Egypt. shimaa.abdelhamid@alexmed.edu.eg
-
Received: ,
Accepted: ,
How to cite this article: El Morsy E, Mohamed R, Omar SI. Intense pulsed light versus pulsed dye laser in the treatment of nail psoriasis: Intra-patient left to right comparative controlled study. Indian J Dermatol Venereol Leprol. 2024;90:713-21. doi: 10.25259/IJDVL_429_2023
Abstract
Background
Until now, the management of psoriatic nails has not been satisfactory. Pulsed dye laser (PDL) as well as intense pulsed light (IPL) have been evaluated separately for the management of psoriatic nails and proved to be effective.
Aim
This study aimed to measure and compare the usefulness as well as the safety of intense pulsed light versus pulsed dye laser for the management of psoriatic nails.
Methods
The psoriatic fingernails of 20 patients were managed using intense pulsed light on one hand and pulsed dye laser on the other. Two to three psoriatic nails were left without treatment as controls. The therapeutic sessions were conducted monthly for a period of 6 months. Evaluation of the clinical outcomes was assessed by a blinded dermatologist depending on the total, nail bed, nail matrix, modified and target NAPSI scores. Patient global assessment, in addition to Nail Psoriasis Quality of Life (NPQL10), was performed to assess the response to the therapy.
Results
A significant reduction in the total, target and modified NAPSI scores from baseline to the end of the study was detected, but no significant differences were detected between the two treatments. The responses of the nail matrix and bed lesions to both modalities were nearly the same. All patients stated that the two devices were efficient and improved their quality of life. The intense pulsed light treatment was more painful. Complete clearance of nail lesions was not obtained.
Limitations
Lack of long-term follow-up of cases and preset laser parameters were the major limitations of this study.
Conclusion
Intense pulsed light, like pulsed dye laser, is safe and efficient in treating nail psoriasis; however, the former is more painful. Dermoscopy had an additive function in analysing the response of nail psoriasis to therapy.
Keywords
Nail psoriasis
PDL
IPL
IPL
NAPSI
Nail bed
Introduction
Psoriatic nails are one of the various presentations of psoriasis, affecting about 50% of cases.1 Clinically, it appears with signs of the nail matrix and/or bed affection.2 It usually involves the fingernails, and other than the unacceptable appearance, 50% of patients complain of pain.1–3 The etiology of nail psoriasis has not been completely understood.4
There are several therapeutic approaches that have been used with different levels of effectiveness in nail psoriasis.5
Laser or light systems that were tried for treating psoriatic nails include pulsed dye laser (PDL), Nd:YAG, intense pulsed light (IPL), psoralen and UVA (PUVA), and excimer laser.5,6 PDL targets oxyhemoglobin and the vascular pathogenetic nature of psoriasis prompted dermatologists to use it in treating psoriasis, given its capability to destroy the dilated and tortuous papillary dermal capillaries in the lesions and consequently decrease infiltrating inflammatory cells.7–10 IPL is a non-laser, polychromatic light source that can release an incoherent output of broad wavelengths ranging between 500 nm and 1200 nm.11 Thus, it has the ability to damage the abnormal vascularity of psoriatic lesions.12
There is no research comparing the efficacy of PDL with IPL in managing psoriatic nails. Hence the key aim of this study was to compare the efficacy and safety of IPL and PDL therapy with controls in treating psoriatic nails. In addition, the study also aimed to compare the responses of nail bed versus nail matrix to each device separately. Dermoscopy is used in evaluating the response of skin psoriasis to treatments and can help diagnose nail psoriasis.13–16 We therefore also aimed to determine if dermoscopy has a role in evaluating the response of psoriatic nails to treatment.
Methods
This prospective, interventional, randomised, single blinded, intra-patient controlled clinical study was carried out on 20 adult patients with bilateral fingernail psoriasis; they were recruited from the Dermatology, Venereology and Andrology outpatient clinic. They were diagnosed according to the clinical and dermoscopic characteristics of nail psoriasis.16 All study cases signed informed consent forms at enrollment. The study protocol was validated by the Ethical Committee of the Faculty of Medicine (ethics code: 0106305) and by the Institutional Review Board for Human Subject Research (number: 00012098). Patients with mild to moderate psoriasis (Psoriasis Area and Severity Index, PASI score <10% of body surface area) who had not received systemic therapy and cases of severe psoriasis who had previously received systemic treatment or phototherapy with no obvious improvement of their nail psoriasis were included in the study.
We excluded pregnant and lactating females, cases suffering from onychomycosis or pustular nail psoriasis, patients who had received any topical anti-psoriatic medications on the nail unit 3 months prior to recruitment, who were treated with systemic or phototherapy for psoriasis within the past 6 months and those with a history of keloid formation. Initially, a complete personal medical history was recorded, and clinical evaluation of nail psoriasis severity was scored via the use of nail bed, nail matrix, total, modified and target NAPSI scores.1,2,17,18
Dermoscopic examination (DermLite DL4, 3Gen LLC, San Juan Capistrano, CA, USA) of nail psoriasis was carried out to ensure diagnosis and determine severity. The dermoscope was placed without pressure over the nail (dry dermoscopy) and a layer of ultrasound gel was used for wet dermoscopy.
The psoriatic fingernails of each patient were randomised into three groups. Fingernails of the right or left hand were randomly managed using PDL (595 nm, V-beam, Prima-Candela Laser Corporation, Wayland, MA, USA), and psoriatic nails of the other side received IPL (Angelite, Advanced Technology, Laser Co., Ltd., Shanghai, China).
Two to three psoriatic nails from the two hands in each patient were left without treatment as controls. The psoriatic nails on each hand were selected randomly using a closed opaque envelope holding a card labelled either ‘PDL’ or ‘IPL’.
Treatment was carried out once in a month for 6 months. The nail plates as well as all nail folds were managed with two passes of laser beams. The following parameters were used for PDL–treatment: 6 ms pulse duration, 10 mm spot size, 6 J/cm2 laser energy with the Moral DCD cooling system. The parameters used for IPL (560 Handpiece)–treatment were: 5 ms pulse duration, 4×1 cm spot size, 5–10 ms pulse delay, 25 J/cm2 fluence.
All patients were instructed to Latex gloves over cotton gloves while applying topical medications to their skin lesions.
Each patient in our study was followed up for 3 months to observe improvement as well as side effects.
Standardised digital, clinical and dermoscopic photographs using the iPhone 11 Pro camera (Apple, Cupertino, Ca, USA) with digital zoom up to 2X and with a connector were obtained at baseline, before the third and fifth treatment sessions, and 3 months after the sixth session to evaluate therapeutic efficacy.
Total, modified and target NAPSI scores were calculated at baseline, during and after treatment by an independent dermatologist to evaluate the outcomes.
The clinical improvement of fingernails was evaluated depending upon the following measures:
The percent reduction in the calculated scores.
Clinical scoring via the use of the index variation.19
Patient global assessment score.20
Patients filled out Nail Psoriasis QOL 10 (NPQL10) questionnaires.
Patient satisfaction with each device was evaluated according to five grading five grading scores in which, 0 means unsatisfied; 1: poor; 2: fair; 3: satisfied; and 4 means extremely satisfied.21
Adverse effects were detected and recorded. The pain was rated by patients following each session on a visual analogue scale.20
Statistical analysis
Data was fed to the computer to be analysed via IBM SPSS software package version 20.0 (Armonk, NY: IBM Corp.). The Shapiro–Wilk test was utilised to verify the normality of distribution. Quantitative data were described via the use of range (minimum and maximum), mean, standard deviation, median and interquartile range. Chi-squared test was used to compare categorical variables between different groups, and Monte Carlo correction was used to adjust the chi-square when more than 20% of the cells had an anticipated count of ˂5. For normally distributed quantitative variables, the F-test (ANOVA) was utilised for comparing between >two groups; Paired t-test was utilised for comparing two periods; ANOVA with repeated measures was estimated for comparing >two periods or stages; and the post-hoc test for pairwise comparisons. For abnormally distributed quantitative variables, the Kruskal Wallis test was utilised for comparing >2 studied groups, the Wilcoxon signed rank test was calculated to compare between two periods, the Friedman test was utilised for comparing >2 periods or stages and the post-hoc test (Dunn’s) for pairwise comparisons. The significance of the obtained results was judged at the 5% level.
Results
Twenty patients [8 men (40%) and 12 women (60%)] participated in the study. The mean age of patients ± standard deviation was 40.25 ± 16.11 years. The majority of sessions were on time. In case of delay, it didn’t exceed one week.
The clinical data of patients is shown in Table 1. A total of 187 psoriatic nails were included in the study; 65 nails were managed using PDL, 68 nails were managed using IPL, and 54 nails were left without treatment as the control arm of the study. The total, modified and target NAPSI scores did not differ significantly between the groups at baseline. The commonest nail change was nail pitting (In Psoriatic nails of all patients), and the least common was red spots in the lunula (in psoriatic nails of 3 patients, 15% of patients).
| No. | % | |
|---|---|---|
| Associated comorbidities | ||
| Negative | 15 | 75.0 |
| Positive | 5 | 25.0 |
| DM | 1 | 5.0 |
| HTN | 4 | 20.0 |
| Joint Affection | 12 | 60.0 |
| Nail disease | 20 | 100.0 |
| Duration (years) | ||
| Min – Max | 3.0–17.0 | |
| Mean ± SD | 7.10 ± 4.01 | |
| Total NAPSI score | ||
| PDL | 4.55 ± 1.36 | |
| IPL | 4.51 ± 1.29 | |
| Control | 3.76 ± 1.75 | |
| Test of Sig. (p) | F = 1.784 (P = 0.177) | |
| Nail Bed Score | ||
| PDL | 1.30 (0.38–2.0) | |
| IPL | 1.28 (0.50–2.0) | |
| Control | 1.0 (0.0–1.90) | |
| Test of Sig. (p) | H = 1.561 (P = 0.458) | |
| Nail Matrix score | ||
| PDL | 3.60 (2.28–4.0) | |
| IPL | 3.63 (2.43–4.0) | |
| Control | 3.38 (2.0–4.0) | |
| Test of Sig. (p) | H = 1.408 (P = 0.495) | |
| Target NAPSI score | ||
| PDL | 5.41 ± 2.16 | |
| IPL | 5.57 ± 2.31 | |
| Control | 4.43 ± 2.23 | |
| Test of Sig. (p) | F = 1.532 (P = 0.225) | |
| Modified NAPSI | ||
| PDL | 3.50 (2.25–4.40) | |
| IPL | 3.13 (2.30–3.63) | |
| Control | 2.55 (1.50–3.75) | |
| Test of Sig. (p) | H = 3.813 (P = 0.149) | |
| Psoriasis | 17 | 85.0 |
| Duration (years) (n = 17) | ||
| Min – Max | 2.0–20.0 | |
| Mean ± SD | 7.94 ± 4.81 | |
| PASI Score (n = 17) | ||
| Min – Max | 5.20–9.50 | |
| Mean ± SD | 7.32 ± 1.56 | |
F: F for One-way ANOVA test; H: H for Kruskal–Wallis test; P: P-value for comparing between the three studied groups; IQR: inter quartile range; SD: standard deviation
Normally quantitative data was expressed in mean ± SD and was compared using a One-way ANOVA test.
While not normally distributed data was expressed in median (IQR) and was compared using Kruskal–Wallis test.
DM: Diabetes mellitus, HTN: Hypertension, NAPSI: Nail Psoriasis Severity Index, PDL: Pulse dye laser, IPL: Intense pulsed light, PASI: Psoriasis Area and Severity Index.
The mean total and target NAPSI scores in both the PDL and IPL– treated nails were significantly reduced during and following treatment in comparison with baseline (P < 0.001). Significant differences were also observed between the scores at 3 months following the last session and the scores before the third treatment session. Moreover, with intense pulsed light, the scores at the fifth treatment visit were significantly decreased in comparison with the third treatment visit. The median-modified NAPSI score achieved with each device following therapy was significantly decreased in comparison with the score before therapy (P < 0.001). In the control group, there was no significant change in the scores throughout the treatment and follow-up visits.
The difference between both treatment groups was not significant with respect to the percentage decrease in total, target or modified NAPSI scores (P > 0.05). The median decrease in the three scores of the PDL and IPL–treated groups was significantly higher in comparison with the controls.
Evaluation of treatment success using the index variation revealed improvement in almost all treated nails with PDL and IPL without a statistically significant difference between them. With intense pulsed light, all patients’ treated nails improved, and with PDL, only one patient’s (5%) treated nails didn’t get better. The majority of nails showed minimal, mild and moderate improvement. Only one patient (5%) achieved great improvement (76–99%) of his treated nails with PDL at the third treatment visit that continued until the fifth visit, and another patient exhibited complete improvement (100%) of his treated nails with IPL at the fifth visit [Table 2 and Figure 1].
| % of improvement in NAPSI score from before sessions | PDL | IPL | Control | χ2 | MCP | |||
|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |||
| Before 3rd session | ||||||||
| Not improvement | 5 | 25.0 | 3 | 15.0 | 12 | 63.2 | 15.051* | 0.014* |
| Minimal (≤25%) | 11 | 55.0 | 14 | 70.0 | 6 | 31.6 | ||
| Mild (>25–50%) | 3 | 15.0 | 1 | 5.0 | 1 | 5.3 | ||
| Moderate (>50–75%) | 0 | 0.0 | 2 | 10.0 | 0 | 0.0 | ||
| Great (>75–99%) | 1 | 5.0 | 0 | 0.0 | 0 | 0.0 | ||
| Complete (100%) | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | ||
| Sig. bet. grps. | MCP1=0.339,MCP2=0.091,MCP3=0.006* | |||||||
| Before 5th session | ||||||||
| Not improvement | 4 | 20.0 | 1 | 5.0 | 14 | 73.7 | 31.317* | <0.001* |
| Minimal (≤25%) | 10 | 50.0 | 7 | 35.0 | 5 | 26.3 | ||
| Mild (>25–50%) | 5 | 25.0 | 9 | 45.0 | 0 | 0.0 | ||
| Moderate (>50–75%) | 0 | 0.0 | 2 | 10.0 | 0 | 0.0 | ||
| Great (>75–99%) | 1 | 5.0 | 0 | 0.0 | 0 | 0.0 | ||
| Complete (100%) | 0 | 0.0 | 1 | 5.0 | 0 | 0.0 | ||
| Sig. bet. grps. | MCP1=0.158,MCP2=0.002*,MCP3<0.001* | |||||||
| 3 months after sessions | ||||||||
| Not improvement | 1 | 5.0 | 0 | 0.0 | 15 | 78.9 | 45.229* | <0.001* |
| Minimal (≤25%) | 7 | 35.0 | 3 | 15.0 | 4 | 21.1 | ||
| Mild (>25–50%) | 9 | 45.0 | 14 | 70.0 | 0 | 0.0 | ||
| Moderate (>50–75%) | 3 | 15.0 | 3 | 15.0 | 0 | 0.0 | ||
| Great (>75–99%) | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | ||
| Complete (100%) | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | ||
| Sig. between groups | MCP1=0.297,MCP2<0.001*, MCP3<0.001* | |||||||
MC: Monte Carlo; χ2: Chi square test
P: P-value for comparing between the three studied groups
P1: P-value for comparing between PDL and IPL
P2: P-value for comparing between PDL and Control
P3: P-value for comparing between IPL and Control
| Nail Bed Score | Before Sessions | Before 3rd session | Before 5th session | 3 months after sessions | p |
|---|---|---|---|---|---|
| PDL | |||||
| Min.–Max. | 0.0–3.0 | 0.0–3.0 | 0.0–3.0 | 0.0–2.50 | 0.054 |
| Median (IQR) | 1.30 (0.38–2.0) | 1.15 (0.13–2.0) | 1.15 (0.25 –1.88) | 0.68 (0.0–1.80) | |
| IPL | |||||
| Min.–Max. | 0.0–3.0 | 0.0–3.0 | 0.0–2.0 | 0.0–3.0 | <0.001* |
| Median (IQR) | 1.28 (0.50–2.0) | 1.28 (0.25–2.0) | 1.0 (0.13–1.7) | 0.40 (0.0–1.50) | |
| p0 | 0.327 | 0.023* | 0.001* | ||
| Sig. bet. periods | p1 = 0.198, p2 = 0.017*, p3 = 0.270 | ||||
| Control | |||||
| Min.–Max. | 0.0–2.0 | 0.0–2.0 | 0.0–2.0 | 0.0–2.0 | 0.133 |
| Median (IQR) | 1.0 (0.0–1.90) | 0.50 (0.0–1.60) | 0.50 (0.0–1.80) | 0.50 (0.0–1.55) | |
IQR: Inter quartile range; SD: Standard deviation
Fr: Friedman test, Sig. bet. Periods was done using Post Hoc Test (Dunn’s)
p: p value for comparing between the four studied periods
p0: p value for comparing between before sessions and each other periods
p1: p value for comparing between before 3rd session and before 5th session
p2: p value for comparing between before 3rd session and 3 months after sessions, PDL: Pulse dye laser, IPL: Intense pulsed light.
p3: p value for comparing between before 5th session and 3 months after sessions
| Nail Matrix Score | Before Sessions | Before 3rd session | Before 5th session | 3 months after sessions | p |
| PDL | |||||
| Min.–Max. | 1.25–4.0 | 0.0–4.0 | 0.0–4.0 | 0.0–4.0 | <0.001* |
| Median (IQR) | 3.60 (2.28–4.0) | 3.15 (2.0–4.0) | 2.80 (1.75–3.68) | 2.55 (1.68–3.38) | |
| p0 | 0.027* | <0.001* | <0.001* | ||
| Sig. bet. periods | p1 = 0.058, p2 = 0.043*, p3 = 0.903 | ||||
| IPL | |||||
| Min.–Max. | 1.25–4.0 | 0.0–4.0 | 0.0–4.0 | 0.0–4.0 | <0.001* |
| Median (IQR) | 3.63 (2.43–4.0) | 3.50 (2.0–4.0) | 2.80 (1.25–3.50) | 2.0 (1.75–3.25) | |
| p0 | 0.221 | <0.001* | <0.001* | ||
| Sig. bet. periods | p1 = 0.006*, p2 = 0.004*, p3 = 0.903 | ||||
| Control | |||||
| Min.–Max. | 0.0–4.0 | 0.0–4.0 | 0.0–4.0 | 0.0–4.0 | 0.413 |
| Median (IQR) | 3.38 (2.0–4.0) | 3.38 (1.80–4.0) | 3.50 (2.0–4.0) | 3.38 (2.0–4.0) | |
IQR: Inter quartile range; SD: Standard deviation
Fr: Friedman test, Sig. bet. Periods was done using Post Hoc Test (Dunn’s)
p: p value for comparing between the four studied periods
p0: p value for comparing between before sessions and each other periods
p1: p value for comparing between before 3rd session and before 5th session
p2: p value for comparing between before 3rd session and 3 months after sessions
p3: p value for comparing between before 5th session and 3 months after sessions, PDL: Pulse dye laser, IPL: Intense pulsed light.

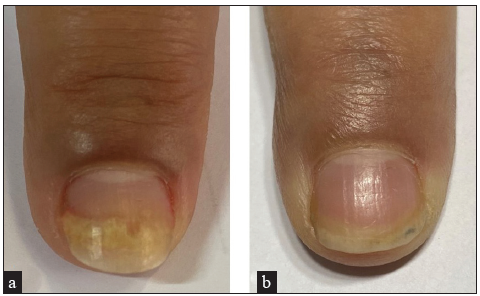
- Right hand psoriatic nails. (a) Before treatment with Intense pulsed light (IPL). (b) Mild Intense pulsed light improvement three months after last right hand psoriatic nails of a 50 years old male.
With both PDL and IPL, there was no significant difference between the median decrease of the nail bed and the nail matrix NAPSI [Figure 2].
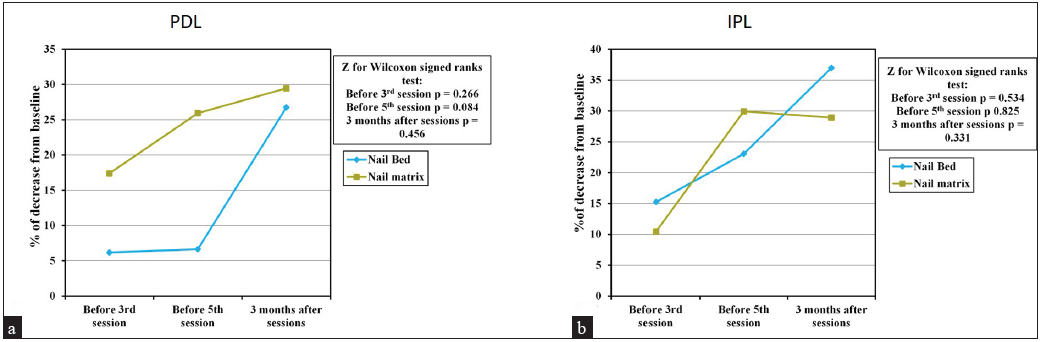
- Comparison between nail bed and nail matrix according to percent improvement from before sessions. (a) With Pulse dye laser (PDL) (b) With Intense pulsed light (IPL).
When we compared the impact of both treatments on the nail bed and matrix scores too, no significant difference was observed (P > 0.5).
Regarding the median nail bed score, there was no statistically significant decrease (P = 0.054) from baseline 1.30 (0.38–2.0) throughout treatment 1.15 (0.13–2.0) and 1.15 (0.25–1.88), respectively and follow up period 0.68 (0.0–1.80) on using PDL. With IPL, significant reduction started following the third session 1.28 (0.25–2.0) and was observed before the fifth treatment visit 1.0 (0.13–1.7) (P = 0.023) and 3 months following the sessions 0.40 (0.0–1.50) (P = 0.001) as well, in comparison to baseline. No significant change (P = 0.133) was observed in controls. Tables 3 and 4 in control 1.0 (0.0–1.90) at baseline and 0.50 (0.0–1.55) 3 months following sessions.
For the median nail matrix score, significant decrease started early with PDL before the third session 3.15 (2.0–4.0), and there was a statistically significant lower score throughout treatment (before 5th session) 2.80 (1.75–3.68) and follow-up period 2.55 (1.68–3.38) (P < 0.001) in comparison to baseline 3.60 (2.28–4.0). With IPL, the significant decrease started later, after the third treatment session, significantly lower scores were observed only before the fifth treatment visit (P < 0.001) and at the follow-up visit 2.0 (1.75 - 3.25) (P < 0.001). There were no significant changes in the untreated [Table 4] groups. untreated group 3.38 (2.0 - 4.0) at baseline and 3 months after last session.
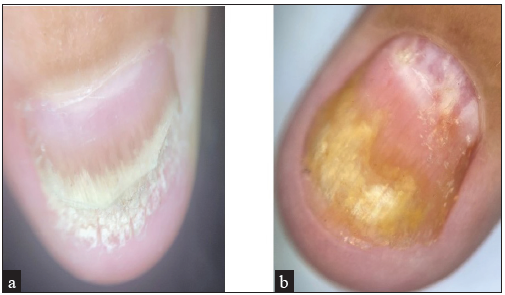
Splinter haemorrhages and lunular erythema were the first and best to respond. Crumbling, leukonychia, onycholysis and ‘oil drops’ showed good improvement, while pitting improved slightly. The least response was seen with subungual hyperkeratosis. [Figures 3 and 4]. By dermoscopy, splinter haemorrhage and oil drops were clearer, and onycholysis severity was well seen. Moreover, it helped in the distinction from onychomycosis [Figure 5].

- Right index psoriatic nail of a 42 years old male (a) Crumbling before treatment with Intense pulsed light (IPL) clinically. (b) Improvement three months after the last session clinically.
- Right index psoriatic nail. Right index psoriatic nail of a 23 years old female (a) Onycholysis before treatment with Pulse dye laser (PDL) clinically. (b) Improvement of onycholysis three months after last session clinically.
- Dry onychoscopy (10x) of psoriatic fingernails. (a) Oil drop, distal onycholysis and subungual hyperkeratosis. (b) Distal onycholysis, oil drops and red spots in lunula.
A significant increase in p value for comparing between the three studied periods with IPL and PDL was <0.001 (p < 0.001) in the mean patient global assessment scores was observed in laser-treated nails without statistically significant differences between IPL and PDL. Before 3rd session: IPL: 3.30 ± 1.30, PDL: 3.35 ± 0.88, (P = 0.887). before 5th session: IPL: 4.90 ± 1.12 PDL: 4.85 ± 1.14, (P = 0.889). After 3 months of sessions: IPL: 7.60 ± 1.19, PDL: 7.25 ± 1.16, (P = 0.353)
Regarding NPQL10, there was a statistically significant decrease (P < 0.001) in the mean score from baseline (PDL: 10.60 ± 4.27, IPL: 10.45 ± 4.71) to the end of the study (PDL: 5.0 ± 2.29, IPL: 4.60 ± 2.76) without significant differences between PDL (5.0 ± 2.29) and IPL (4.60 ± 2.76) treated groups (P = 0.621) after sessions. Patient satisfaction was nearly equal in both laser-treated groups (P = 0.587). The majority of cases (60%) were satisfied with the improvement. Five patients (25%) were extremely satisfied with PDL, seven patients (35%) had the same impression with IPL, and three patients (15%) reported fair satisfaction with PDL and only one patient (5%) with IPL.
The pain was transient and felt mainly during the session. It lasted for seconds to minutes in the majority of patients and in few patients, pain persisted for hours. Transient pain was felt by all treated patients. The mean pain score in the IPL–treated group (5.80 ± 1.24) was significantly higher when compared to the PDL–treated group (4.05 ± 1.28) (P < 0.001). There were no other reported adverse effects.
Discussion
Management of nail psoriasis remains a challenge because it requires addressing diverse pathological alterations. Lasers have become one of the most attractive, non-invasive therapeutic modalities for psoriatic nails, as they have the capability of penetrating the nail plate to treat lesions with no systemic adverse influences. PDL has been studied for treating psoriatic nails and its efficiency confirmed. Nevertheless, there is no agreement among the parameters to be used.5,9,22,23 We found only two studies that investigated the effect of IPL on nail psoriasis.12,24
In this study, there was a significant reduction in total, modified and target NAPSI scores from baseline throughout all sessions to 3 months following therapy using PDL and IPL separately, while there were no significant changes in the control group.
In spite of using various parameters, the results of the current study were in coherence with the findings of previous studies on the treatment of nail psoriasis with PDL.9,22,25,26
Tawfik et al. concluded that twice-per-month treatment with IPL for 6 months was an efficient and safe therapeutic modality for psoriatic nails.12 Shaheen et al. found that even six treatment sessions with IPL over 3 months were sufficient to improve nail psoriasi.24 These findings too are in accordance with our observations.
The NAPSI score provides an objective evaluation of improvement and is the most commonly used scoring method. It also helps evaluate the influence of therapy on the nail matrix and bed. Nevertheless, it is not adequately sensitive. So, in addition, modified and target NAPSI scores were calculated to provide a more comprehensive evaluation of the target nail for each of the eight parameters.1,2 The significant decrease in modified NAPSI score with PDL in the current study was concordant with the results documented by Huang et al.23 and highlights the added value of using this score to ensure clinical responses to therapy. Similar to Roter et al.27 who treated the psoriatic nails with PDL alone versus ND-YAG and PDL every 4 weeks for 3 months, there was a significant reduction in target NAPSI with PDL.
This study is the first to calculate the target and modified NAPSI for evaluating the impact of IPL on nail psoriasis. Additionally, this work is the first to analyse all three scores in the same study.
This is also the first study comparing PDL versus IPL in the treatment of psoriatic nails, and the results showed no significant differences between the two treatment devices with regard to the percent reduction in NAPSI scores.
Evaluation with index variation revealed that the highest percentage of improvement with PDL (>76–99 %) had been achieved before the third session in only one patient (5 %) and was maintained till before the fifth session, and with IPL it was 100% improvement which had been achieved in a single patient (5%) before the fifth session. To the best of our knowledge, there was no previous study that calculated this score. However, Al-Mutairi et al.28 documented that 55% of the hands treated with PDL achieved NAPSI 75, and 14% achieved NAPSI 100 following 3 months of therapy, and these achievements continued till the end of the study. Furthermore, with intense pulsed light,Tawfiq et al.12 reported that 86.4% of the nail lesions improved. In the current work, all nails treated with IPL improved.
In the current study, although nail matrix lesions improved earlier with PDL and nail bed signs showed improvement earlier with IPL, there was no statistically significant difference between the effects of PDL and IPL on nail bed and matrix lesions. From what we know, no previous study mentioned this result. With PDL, although the decreased nail matrix scores were significant and the decreased nail bed scores were non-significant, no significant differences were demonstrated between the response of nail bed and nail matrix lesions to PDL and such results were consistent with the observations of previous studies.25–28 On the other hand, one previous study concluded that the principal influence was on nail matrix lesions,23 while yet another report mentioned better improvement of nail bed psoriasis.9
In this study, with IPL, significant improvements in nail bed and matrix lesions started following the third session. In opposition, Tawfiq et al.12 reported that nail bed lesions improved faster than nail matrix lesions and better.
Regarding the isolated nail bed and matrix lesions, in contrast to Treewittayapoom et al.,22 in the current study, as expected for the light system that targeted oxyhaemoglobin, splinter haemorrhage improved best with therapy. This finding was in agreement with a recent observation.27 At variance with Oram et al.9 and Al-Mutairi et al.28 who used PDL and Tawfiq et al.12 with IPL, subungual hyperkeratosis was most refractory to therapy with both devices in our study. The explanation for this might be that a thickened nail plate and accumulated scales limit the transfer of the laser beam to the nail bed, and more sessions might be necessary to improve the subungual hyperkeratosis.
Dermoscopic signs were utilised in conjunction with the clinical findings to determine psoriatic nail lesions and to assess nail changes with therapy for more precise evaluation. In consonance with Alessandrini et al., Khashaba et al. and Wanniang et al., splinter haemorrhage was determined to be more prominent with dermoscopy.29–31
All patients reported that their nail lesions continuously improved during the treatment period and the improvement continued following cessation of sessions with both devices, with no significant differences. Al-Mutairi et al.28 had similar findings with PDL. In contrast, Huang et al.23 found that only 47.3% of the treated cases felt that their nails showed improvement after using PDL.
All patients revealed different degrees of satisfaction with the results of both therapy, with no statistically significant differences between both devices. Tawfiq et al.12 documented that 10% of their cases were not satisfied with the results of IPL. In our work, the treatment of nail psoriasis with PDL and IPL improved the patients’ quality of life without significant differences. A similar observation was reported by Roter et al. and Peruzzo et al., who instead used the DLQ1 survey to detect the impact of PDL.27,32
In contrast with Treewittayapoom et al. and Soliman et al.22,33 who detected purpura with PDL, no such effects were reported with PDL in this study: this might be due to our usage of non-purpuric device parameters.
Fernandez-Guarino et al. and Perruzo et al. observed pain with PDL, and Tawfik et al. revealed pain with IPL use in psoriatic nails.25,32,12 Despite all patients complaining of temporary pain following each treatment session, the majority of patients reported that they felt pain during session and pain lasted for seconds to minutes. In a few of them, pain lasted for hours and all reported that treatment with IPL was significantly more painful. This might be attributed to the built-in dynamic cooling equipment system used in PDL but not with IPL. To our knowledge, this study was the first to compare PDL with IPL regarding pain sensation, the pain was equal (nail plate as nail folds in the intensity).
Limitations
The main limitation of our study was the absence of long follow-up period. As a result, there may have been a false impression regarding the absence of relapse. Long-term follow-up should be considered for future research. This study was also limited by the use of preset parameters and number of sessions which made it impossible to compare the influence of varied parameters and number of sessions on nail psoriasis.
Conclusion
According to our results, IPL is as effective as PDL in treating nail bed and matrix psoriatic lesions. Furthermore, both therapies are well accepted by patients. However, neither of the devices achieved complete clearance, and IPL was more painful. Dermoscopy has an additive role in evaluating psoriatic nail response to therapy.
Ethical approval
The study protocol was validated by the Ethical Committee of the Faculty of Medicine (ethics code: 0106305) and by the Institutional Review Board for Human Subject Research (number: 00012098).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Diagnosis and management of nail psoriasis. Actas Dermosifiliogr. 2008;99:34-43.
- [PubMed] [Google Scholar]
- Nail psoriasis severity index: A useful tool for evaluation of nail psoriasis. J Am Acad Dermatol. 2003;49:206-12.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis of the nails associated with disability in a large number of patients: Results of a recent interview with 1,728 patients. Dermatology. 1996;193:300-3.
- [CrossRef] [PubMed] [Google Scholar]
- Nail psoriasis: Clinical features, pathogenesis, differential diagnoses, and management. Psoriasis (Auckl). 2017;7:51.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Laser and light therapies for the treatment of nail psoriasis. J Eur Acad Dermatol Venereol. 2016;30:1278-84.
- [CrossRef] [PubMed] [Google Scholar]
- Non-pharmacological treatments of nail psoriasis and the assessment of therapeutic progress. Prz Dermatol. 2019;106:280-90.
- [Google Scholar]
- Laser and novel light source treatments for psoriasis. Lasers Surg Med. 2004;35:165-73.
- [CrossRef] [PubMed] [Google Scholar]
- Pulsed dye laser in the treatment of nail psoriasis. Dermatol Surg. 2010;36:377-81.
- [CrossRef] [PubMed] [Google Scholar]
- In vivo quantification of the structural abnormalities in psoriatic microvessels before and after pulsed dye laser treatment. Br J Dermatol. 2005;152:505-11.
- [CrossRef] [PubMed] [Google Scholar]
- Novel treatment of nail psoriasis using the intense pulsed light: A one-year follow-up study. Dermatol Surg. 2014;40:763-8.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy as a prognostic tool for the therapeutic response of phototherapy and methotrexate in psoriasis. J Egypt Women’s Dermatol Soc. 2020;17:164.
- [Google Scholar]
- Dermoscopic hemorrhagic dots: An early predictor of response of psoriasis to biologic agents. Dermatol Pract Concept. 2016;6:7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermoscopy to detect signs of subclinical nail involvement in chronic plaque psoriasis: A study of 68 patients. Indian J Dermatol. 2015;60:272.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A study of dermoscopic features of nail psoriasis. Postep Derm Alergol. 2017;34:28-35.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The modified Nail Psoriasis Severity Index: Validation of an instrument to assess psoriatic nail involvement in patients with psoriatic arthritis. J Rheumatol. 2007;34:123-9.
- [PubMed] [Google Scholar]
- Recommendations for the definition, evaluation, and treatment of nail psoriasis in adult patients with no or mild skin psoriasis: A dermatologist and nail expert group consensus. J Am Acad Dermatol. 2019;81:228-40.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of nail psoriasis with pulse dye laser plus calcipotriol betametasona gel vs. Nd: YAG plus calcipotriol betamethasone gel: An intrapatient left-to-right controlled study. Actas Dermosifiliogr. 2017;108:140-4.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional carbon dioxide laser for keratosis pilaris: A single‐blind, randomized, comparative study. Bio Med Res Int. 2016;2016:1928540.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The effect of different pulse durations in the treatment of nail psoriasis with 595-nm pulsed dye laser: A randomized, double-blind, intrapatient left-to-right study. J Am Acad Dermatol. 2012;66:807-12.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of pulsed dye laser plus topical tazarotene versus topical tazarotene alone in psoriatic nail disease: A single‐blind, intrapatient left‐to‐right controlled study. Lasers SurgMed. 2013;45:102-7.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison between the efficacy of intense pulsed light (IPL) versus photodynamic therapy with methylene blue in the treatment of nail psoriasis. QJM. 2021;114:hcab093.12.
- [Google Scholar]
- Pulsed dye laser vs. photodynamic therapy in the treatment of refractory nail psoriasis: Comparative pilot study. J Eur Acad Dermatol Venereol. 2009;23:891-5.
- [CrossRef] [PubMed] [Google Scholar]
- Pulsed dye laser in the treatment of psoriatic nails: A controlled study. J Eur Acad Dermatol Venereol. 2016;31:e49-e50.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of nail psoriasis with pulsed dye laser versus combined pulsed dye and Nd: YAG lasers—An intrapatient left‐to‐right study. Lasers Surg and Med. 2022;54:688-92.
- [CrossRef] [PubMed] [Google Scholar]
- Single blinded left-to-right comparison study of excimer laser versus pulsed dye laser for the treatment of nail psoriasis. Dermatol Ther (Heidelb). 2014;4:197-205.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermoscopy in the evaluation of nail disorders. Skin Appendage Disord. 2017;3:70-82.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Efficacy of long-pulsed Nd-YAG laser in the treatment of nail psoriasis: A clinical and dermoscopic evaluation. J Dermatolog Treat. 2021;32:446-52.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative study of clinical and dermoscopic features in nail psoriasis. Indian Dermatol Online J. 2020;11:35.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Nail psoriasis treated with pulsed dye laser. An Bras Dermatol. 2017;92:885-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pulsed-dye laser versus intralesional steroid in the management of nail psoriasis: A randomized, intra-patient, comparative, controlled study. The J Clin Aesthet Dermatol. 2021;14:45-9.
- [PubMed] [PubMed Central] [Google Scholar]






