Translate this page into:
Interface dermatitis without cornoid lamellae is a pitfall in the diagnosis of porokeratosis: A report of three cases
2 Department of Dermatology, Santa Casa de Misericórdia de Curitiba Hospital, Paraná, Brazil
Correspondence Address:
Rajiv Joshi
14 Jay Mahal, A Road, Churchgate, Mumbai, Maharashtra - 400 020
India
| How to cite this article: Joshi R, Mesquita L. Interface dermatitis without cornoid lamellae is a pitfall in the diagnosis of porokeratosis: A report of three cases. Indian J Dermatol Venereol Leprol 2016;82:70-72 |
Sir,
The histopathological sine qua non of porokeratosis in all its clinical variants is the presence of the cornoid lamella which consists of a column of parakeratotic corneocytes that appear to arise from a dell in the epidermis in association with focal absence of the stratum granulosum.[1] Dyskeratotic cells are frequently seen in the upper spinous layers.[1] In the absence of a cornoid lamella it is difficult to render a histological diagnosis of porokeratosis.
Porokeratosis is also considered in the differential diagnosis of a lichenoid dermatitis as it frequently shows the presence of a focal lichenoid infiltrate, composed of lymphocytes and a few melanophages. The lichenoid changes are often subtle and in the superficial actinic and non-actinic types of porokeratosis may be very focal and restricted to a small area just beneath the cornoid lamellae. In the classical Mibelli form of porokeratosis, the lichenoid infiltrate with melanophages may also be seen in the atrophic central part of the lesion.
Interface dermatitis with basal cell vacuolization, however, is not commonly seen in porokeratosis and if present, dermatoses like lichen planus and lupus erythematosus must be considered. Vacuolar-interface dermatitis with dermal melanosis occurs in lichen planus pigmentosus, pigmenting atrophic lichen planus and discoid lupus erythematosus but is not seen usually in porokeratosis.
We describe three cases of porokeratosis that presented with interface dermatitis without typical cornoid lamellae in the initial sections which caused confusion in the histological diagnosis.
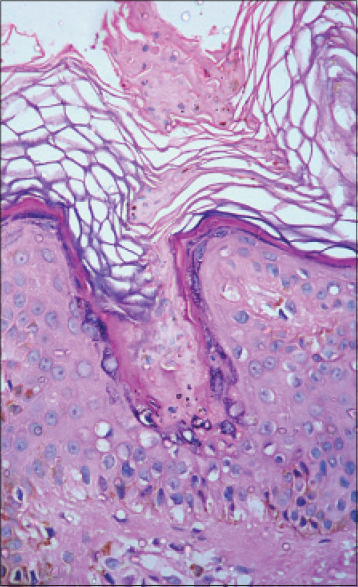
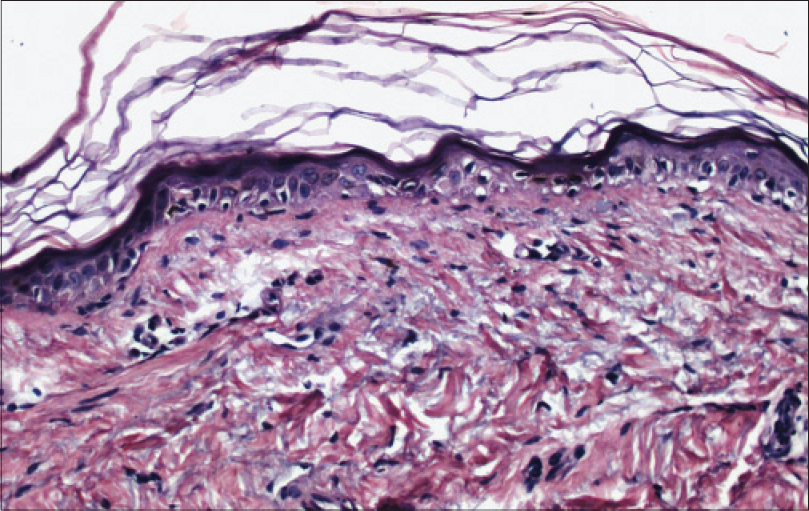
Case 1 was a 7-year-old boy who had a keratotic pigmented lesion on the back of the leg noticed for a few months. The referring clinician had a differential diagnosis of lichen planus and porokeratosis, however, no further morphological details were available. A 4 mm punch biopsy from the lesion was received and it showed features of pigmenting interface dermatitis with a flattened epidermis, basket weave stratum corneum, basal cell vacuolization, colloid bodies in the upper papillary dermis and incontinence of melanin with numerous melanophages in the papillary dermis [Figure - 1]. No cornoid lamella was identifiable.
 |
| Figure 1: Case 1, Interface dermatitis with extensive basal cell vacuolization and numerous melanophages in the papillary dermis (H and E, ×100) |
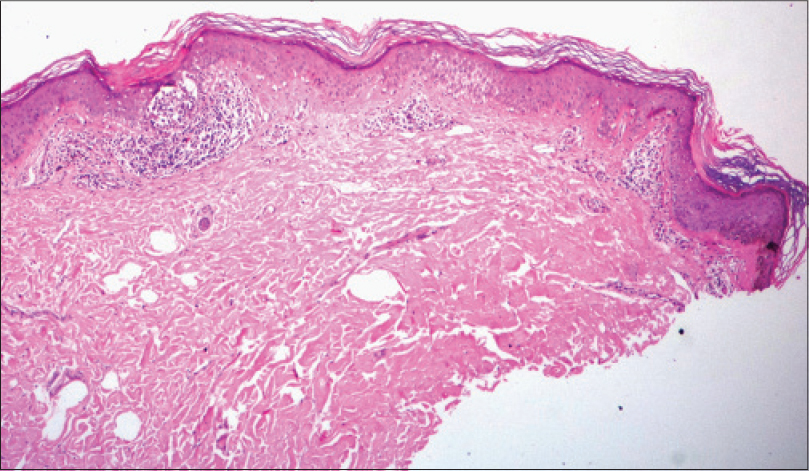
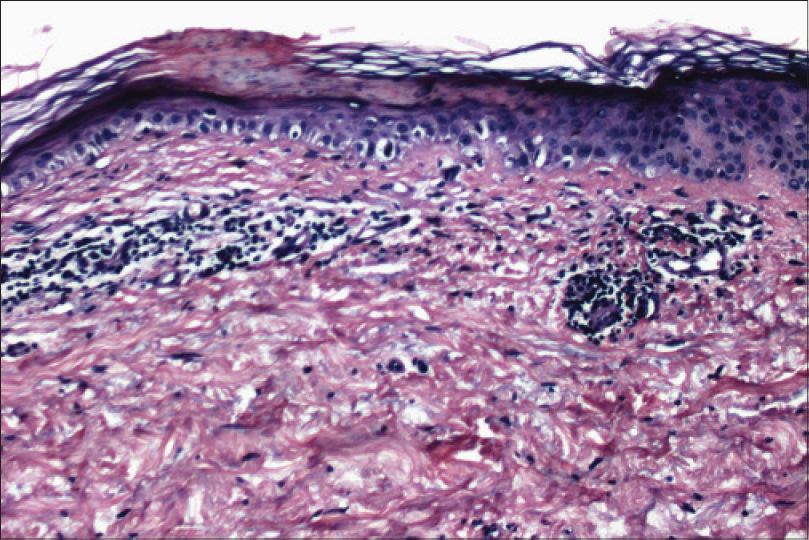
Considering the clinical diagnosis of lichen planus with the histological findings of an interface dermatitis and absence of cornoid lamella, a diagnosis of pigmenting interface dermatitis consistent with atrophic lichen planus was rendered. At the request of the clinician, deeper sections were obtained and to our surprise showed, in addition to pigmenting interface dermatitis, the presence of a cornoid lamella at one end of the section [Figure - 2]. The diagnosis was accordingly revised to porokeratosis.
 |
| Figure 2: Case 1, Deeper sections demonstrating a cornoid lamella (H and E, ×400) |
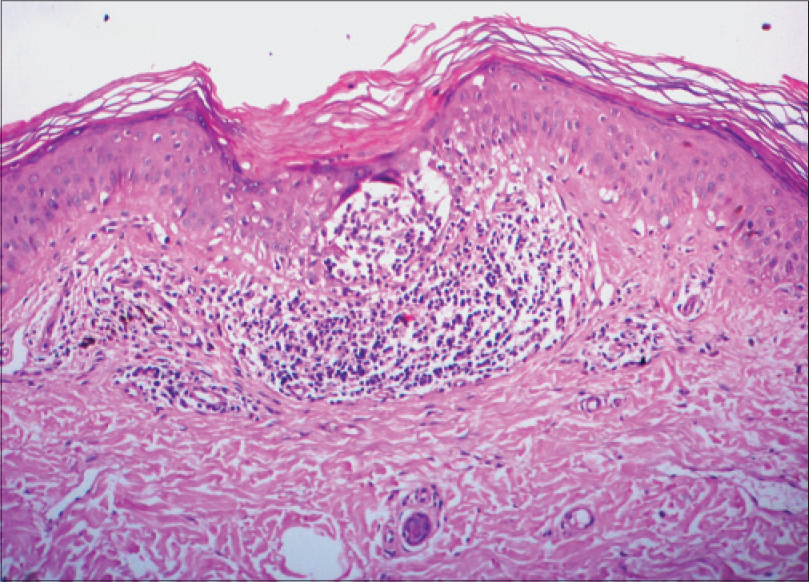
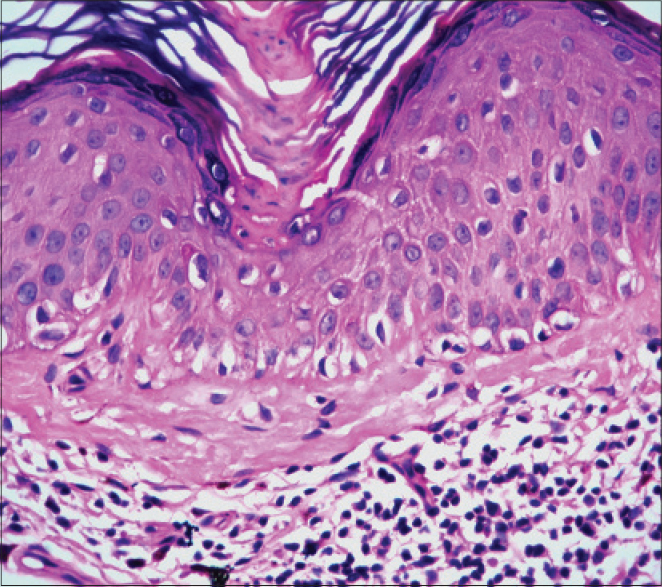
Case 2 was a 27-year-old man who had multiple small hyperpigmented flat-topped papules on the extensor surfaces of both forearms, chest and face for a few months. The clinical differential diagnoses were disseminated superficial actinic porokeratosis, lentigines, plane warts and dermatosis papulosa nigra. A 4 mm punch biopsy from the dorsum of the right hand showed focal interface-lichenoid dermatitis in three locations without cornoid lamellae [Figure - 3]. One of the areas showed a lichenoid lymphocytic infiltrate with melanophages in the papillary dermis with infiltration of the lower epidermis by many lymphocytes and with an overlying thickened laminated horny layer without parakeratosis or cornoid lamella formation [Figure - 4]. Deeper sections taken through the block revealed a short cornoid lamella typical of superficial porokeratosis, with a lichenoid lymphocytic infiltrate in the papillary dermis [Figure - 5].
 |
| Figure 3: Case 2, Interface-lichenoid dermatitis seen in three foci (H and E, ×100) |
 |
| Figure 4: Case 2, Higher power showing a lichenoid lymphocytic infi ltrate with melanophages, lymphocytic collection in the lower epidermis and a thickened horny layer without parakeratosis (H and E, ×400) |
 |
| Figure 5: Case 2, Deeper sections showing a small cornoid lamella overlying a lichenoid lymphocytic infi ltrate (H and E, ×400) |
Case 3 was a 76-year-old man who presented with scaly plaques on both legs for a few months. The clinician had a differential diagnosis of lichen simplex chronicus and psoriasis. A 3 mm punch biopsy from the right leg revealed a flat epidermis with very mild basal cell vacuolization, occasional colloid bodies at the dermo-epidermal junction, occasional melanophages and mild solar elastosis without a significant dermal inflammatory infiltrate [Figure - 6]. A histological diagnosis of possible vacuolar interface dermatitis was suggested. The patient was subsequently seen by another clinician who considered the possibility of porokeratosis and requested deeper sections which did indeed show a small cornoid lamella, overlying a focal lichenoid lymphocytic infiltrate in the papillary dermis [Figure - 7].
 |
| Figure 6: Case 3, Flat epidermis with very mild basal cell vacuolization and a few colloid bodies at the dermo-epidermal junction (H and E, ×100) |
 |
| Figure 7: Case 3, Deeper sections demonstrating a cornoid lamella (H and E, ×400) |
These three cases highlight the fact that porokeratosis may occasionally present histologically with interface dermatitis without the pathognomonic cornoid lamellae and may be mistaken for true interface diseases like lichen planus, lichen planus pigmentosus, cutaneous lupus erythematosus or other dermal melanoses.
The presence of interface-lichenoid dermatitis in porokeratosis has been described in a few publications in patients with disseminated superficial actinic porokeratosis. In all of them the lichenoid infiltrate with basal cell vacuolization was always associated with a cornoid lamella allowing for the histological diagnosis of porokeratosis.[2],[3] 'One of the features of (disseminated superficial actinic porokeratosis) is that the lichenoid inflammation is associated with a parakeratotic column in contrast to the orthokeratosis seen with lichen planus, the prototype of lichenoid reaction pattern'.[2]
In our cases, the vacuolar changes were more prominent than the lichenoid and were not associated with parakeratotic columns in the initial sections; thus constituting a pitfall, as pathologists would tend to diagnose more common interface dermatoses like lichen planus, especially if the clinical differential diagnosis was indeed lichen planus!
Parenthetically, if the biopsy were to include only the centre of the lesion and not the cornoid lamella located at the periphery, a psoriasiform dermatitis or an atrophic lichenoid dermatitis may be seen.
It is therefore important for histopathologists to be aware that vacuolar-interface dermatitis without cornoid lamellae may be seen in porokeratosis in initial sections and may be wrongly diagnosed as other interface dermatoses, especially if the clinician does not suspect the diagnosis of porokeratosis. Alternately, if the clinical diagnosis is porokeratosis, and even if another diagnosis is possible on initial sections, it is advisable to look for cornoid lamellae in deeper sections.
| 1. |
Porokeratosis: In Dermatopathology. 3rd ed. In: Barnhill R, Crowson AN, Magro CM, Piepkorn MW, editors. New York: McGraw Hill; 2010.p. 323-4
[Google Scholar]
|
| 2. |
Shumack S, Commens C, Kossard S. Disseminated superficial actinic porokeratosis. A histological review of 61 cases with particular reference to lymphocytic inflammation. Am J Dermatopathol 1991;13:26-31.
[Google Scholar]
|
| 3. |
Inazawa M, Satoh T, Yokozeki H. Hyperkeratotic variant of inflammatory disseminated superficial porokeratosis with lichenoid reaction and extensive amyloid deposition. Int J Dermatol 2014;53:e94-5.
[Google Scholar]
|
Fulltext Views
4,460
PDF downloads
1,979





