Translate this page into:
Intralesional methotrexate as an adjuvant treatment for pyoderma gangrenosum: A case report
2 Department of Dermatology, Medicine School, Pontificia Universidad Católica de Chile, Santiago; Department of Dermatology, Unit of Immunology and Connective Tissue Diseases, Medicine School, Pontificia Universidad Católica de Chile, Santiago, Chile
Correspondence Address:
Cristián Vera-Kellet
Department of Dermatology, Unit of Immunology and Connective Tissue Diseases, Medicine School, Pontificia Universidad Católica de Chile, Santiago
Chile
| How to cite this article: del Puerto C, Navarrete-Dechent CP, Carrasco-Zuber JE, Vera-Kellet C. Intralesional methotrexate as an adjuvant treatment for pyoderma gangrenosum: A case report. Indian J Dermatol Venereol Leprol 2017;83:277 |
Sir,
Pyoderma gangrenosum is a chronic and relapsing ulcerative neutrophilic dermatosis. In up to 70% of cases, it is associated with systemic diseases, mainly inflammatory bowel disease, seronegative arthritis and lymphoproliferative disorders.[1]
The disease presents as painful, rapidly growing ulcers with erythematous-violaceous undermined borders that leave behind cribriform scars. First-line therapies include wound care, occlusive dressings, topical antimicrobial agents, topical and intralesional corticosteroids and high doses of systemic corticosteroids.[1]
We present the case of an otherwise healthy man with pyoderma gangrenosum who showed an excellent response to intralesional methotrexate and oral corticosteroids.
A 35-year-old man presented with an eighteen-month history of painful ulcers on both calves. Three ulcers with erythematous-violaceous undermined borders were noticed on his right leg and one on the left leg [Figure - 1]. A detailed laboratory evaluation was done including complete blood counts, erythrocyte sedimentation rate, antinuclear antibodies, chest radiograph, quantiferon gold assay for tuberculosis and human immunodeficiency virus (HIV) serology all of which were unremarkable. Bacterial, fungal and mycobacterial cultures from the ulcer were negative. A skin biopsy showed ulceration surrounded by granulation tissue with a scant, diffuse infiltrate of lymphocytes, neutrophils and plasmacytes and fibrosis but without any signs of vasculitis [Figure - 2] and a negative periodic acid-Schiff stain, all suggestive of pyoderma gangrenosum. Associated systemic diseases were ruled out with normal blood and urine protein electrophoresis, sacroiliac radiography, rheumatoid factor and gastroenterology evaluation including colonoscopy.
 |
| Figure 1: Painful ulcer with undermined borders, at first visit |
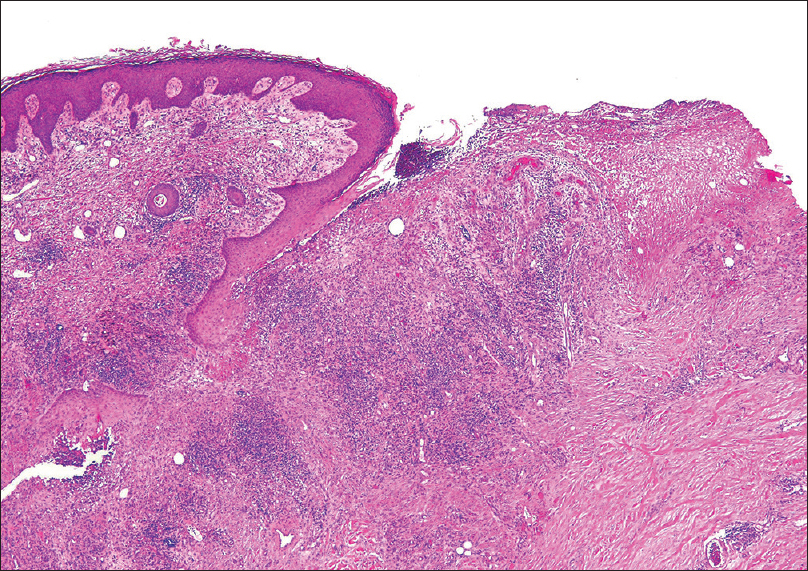 |
| Figure 2: An ulcer surrounded by granulation tissue with fibrosis and scant diffuse infiltrate of lymphocytes, neutrophils and plasmacytes without signs of vasculitis (biopsy taken from the border of one ulcer) (H and E, ×100) |
Treatment was initiated with oral prednisolone, 60 mg/day and the ulcers were managed with regular wound care but there was hardly any response even after 40 days. Therefore, oral methotrexate 10 mg weekly was added for 2 months, again without much response. Then we decided to change the route of administration of methotrexate and intralesional methotrexate (injectable solution of methotrexate 50 mg/2 ml; given 25 mg/week) was given along the erythematous border of the ulcers, in addition to oral prednisone. The response was outstanding since the first dose and by the seventh injection, almost 90% of ulcers on his right leg were cicatrized [Figure - 3]. Lesions on his left calf also showed a similar response. At 10 months of follow-up, the patient was completely free of disease and without new lesions.
 |
| Figure 3: Almost complete response after the seventh injection of intralesional methotrexate |
Pyoderma gangrenosum is a painful ulcerating dermatosis that can be a cause of considerable disfigurement, impacting the quality of life and associated with high morbidity and even mortality.[1] There are no standardized guidelines for the management of pyoderma gangrenosum. For most workers, systemic corticosteroids and systemic cyclosporine are first-line therapies.[1],[2] Second-line therapies include tumor necrosis factor-alpha inhibitors (infliximab, adalimumab and etanercept), dapsone and immunosuppressive agents.[2],[3] Immunosuppressive agents such as mycophenolate mofetil, methotrexate and azathioprine are commonly used as adjunctive therapies.[2] For recalcitrant pyoderma gangrenosum, alkylating agents such as cyclophosphamide and chlorambucil as well as intravenous immunoglobulin have been tried with some success. However, their high cost and potentially severe side effects prompt the use of other interventions.
Methotrexate is a potent anti-inflammatory agent when used in low concentrations.[4] Its mechanism in cutaneous disease is controversial but is thought to be mainly mediated by adenosine, a purine nucleoside with potent anti-inflammatory effects. Methotrexate inhibits 5-aminoimidazole-4-carboxamide ribonucleotide transformylase, promoting intracellular accumulation of 5-aminoimidazole-4-carboxamide ribonucleotide which increases local adenosine release.[4] There is inhibition of neutrophil and monocyte oxidative burst, inhibition of neutrophil chemotaxis and reduction in the secretion of inflammatory cytokines (tumor necrosis factor-alpha and interleukin-2).
In this case, the use of oral methotrexate elicited no clinical response even after 8 weeks, though response was expected in the first 4–8 weeks of treatment. However, after the first dose of intralesional methotrexate itself, there was a remarkable response. We believe that due to local inflammation, the bioavailability of oral methotrexate was lower in the wound site. Intralesional cyclosporine has been tried previously in patients with refractory pyoderma gangrenosum with complete resolution. However, in our country, the cost of cyclosporine is ten times higher than methotrexate. Besides, the fact that cyclosporine is not covered by public health insurance favored the use of methotrexate. On the basis of the case reports which cite successful response of keratoacanthomas, squamous cell carcinoma, primary cutaneous CD30+ T-cell lymphomas and other inflammatory conditions like nail psoriasis to intralesional methotrexate, we thought that intralesional methotrexate could have a better local bioavailability and faster action in comparison to oral methotrexate.[5]
We were unable to find any previous reports of pyoderma gangrenosum successfully treated with intralesional methotrexate in addition to systemic corticosteroids. Considering that pyoderma gangrenosum is a disease which requires long term treatment with immunosuppressive agents, intralesional methotrexate may be considered as a good adjuvant in the management of recalcitrant cases. Further studies are needed in order to confirm our findings.
Acknowledgment
Sergio González, MD.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Binus AM, Qureshi AA, Li VW, Winterfield LS. Pyoderma gangrenosum: A retrospective review of patient characteristics, comorbidities and therapy in 103 patients. Br J Dermatol 2011;165:1244-50.
[Google Scholar]
|
| 2. |
Ruocco E, Sangiuliano S, Gravina AG, Miranda A, Nicoletti G. Pyoderma gangrenosum: An updated review. J Eur Acad Dermatol Venereol 2009;23:1008-17.
[Google Scholar]
|
| 3. |
Brooklyn TN, Dunnill MG, Shetty A, Bowden JJ, Williams JD, Griffiths CE, et al. Infliximab for the treatment of pyoderma gangrenosum: A randomised, double blind, placebo controlled trial. Gut 2006;55:505-9.
[Google Scholar]
|
| 4. |
Shen S, O'Brien T, Yap LM, Prince HM, McCormack CJ. The use of methotrexate in dermatology: A review. Australas J Dermatol 2012;53:1-18.
[Google Scholar]
|
| 5. |
Good LM, Miller MD, High WA. Intralesional agents in the management of cutaneous malignancy: A review. J Am Acad Dermatol 2011;64:413-22.
[Google Scholar]
|
Fulltext Views
3,823
PDF downloads
1,849





