Translate this page into:
Intralesional radiofrequency ablation for nodular angiolymphoid hyperplasia on forehead: A minimally invasive approach
2 Department of Radiodiagnosis, All India Institute of Medical Sciences, New Delhi, India
3 Department of Pathology, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Somesh Gupta
Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi - 110 029
India
| How to cite this article: Singh S, Dayal M, Walia R, Arava S, Sharma R, Gupta S. Intralesional radiofrequency ablation for nodular angiolymphoid hyperplasia on forehead: A minimally invasive approach. Indian J Dermatol Venereol Leprol 2014;80:419-421 |
Abstract
Angiolymphoid hyperplasia with eosinophilia (ALHE) is an idiopathic acquired condition characterized by erythematous papulo-nodular lesions with a predilection for the head and neck. The lesions are cosmetically disfiguring, resistant to most medical and surgical therapies and tend to recur. We report the novel use of radiofrequency equipment in the management of nodular ALHE on forehead of a 53-year-old man. Intra-lesional radiofrequency ablation was done using a modified 18 gauge intravenous cannula and three sittings over a period of four years yielded cosmetically acceptable results with no recurrence and minimal side effects.INTRODUCTION
Angiolymphoid hyperplasia with eosinophilia (ALHE) is an acquired disorder of unknown etiology. Its exact nosological status is unclear since it has been variously described as either a T cell pseudolymphoma or benign reactive vascular proliferation. [1] It has a predilection for the head and neck region and is cosmetically disfiguring. ALHE is a difficult condition to treat and recurrences are common despite treatment. Radiofrequency (RF) is a form of high frequency electro-surgery which works on the principle of increasing the frequency and voltage while simultaneously decreasing the amperage of alternating current. This electrical energy gets converted to heat when faced with tissue resistance. [2] The procedure has the advantages of good intra-operative hemostasis and simplicity of the procedure. We tried a novel technique of intra-lesional RF surgery in a patient with nodular ALHE on the forehead and were able to achieve a good cosmetic result without recurrence.
CASE REPORT
A 53-year-old man presented with an asymptomatic, slowly-growing nodular swelling over forehead and frontal scalp for a period of 15 years along with multiple erythematous papules and nodules over and around the swelling for the past 10 years. The smaller papules were gradually increasing in number and occasional bled on trivial trauma. He did not have any systemic complaints. Dermatological examination revealed an approximately 6 × 6 cm oval, skin-colored, subcutaneous nodule on the left side of forehead. There were multiple erythematous papules and nodules of 0.5 to 1.5 cm scattered over and around the nodule. The lesions were firm in consistency, non-tender and did not have any overlying ulceration or active bleeding [Figure - 1]. There was no regional lymphadenopathy. Routine investigations including hemogram, liver and renal function tests and urine microscopy did not reveal any abnormality. Fine needle aspiration cytology from the large nodule revealed blood admixed with lymphocytes. With a provisional clinical diagnoses of ALHE and vascular malformation, skin biopsy was done from both the subcutaneous large nodule as well as superficial papules. Biopsy showed numerous capillaries in the dermis with prominent plump endothelial cells surrounded by dense aggregates of lymphocytes and eosinophils, a picture consistent with ALHE [Figure - 2]. On magnetic resonance imaging (MRI), T1 weighted images showed a hypo-intense soft tissue lesion in the frontal scalp with no underlying defect or communication and a small subcutaneous nodule in the occipital region which was not felt on examination [Figure - 3] left half]. Both these lesions showed heterogeneous enhancement following gadolinium contrast [Figure - 3] right half]. The swelling showed minimal response to ten fortnightly intra-lesional triamcinolone injections. Considering the large size, depth and vascularity of the swelling, we decided to perform intra-lesional RF ablation. An 18 gauge intravenous cannula Venflon® (BD India Pvt Ltd, Haryana, India) was taken and a small window was created in its plastic sheath using a 15-number surgical blade. In addition, the distal 0.5 to 1 cm of the plastic catheter was also removed to ensure wider release of electrosurgical output power [Figure - 4]a. This cannula, intact with the metallic trocar, was then inserted inside the ALHE lesions to appropriate depth (so that the window remained outside the tissue). Intra-lesional RF was then performed under field block, using the standard Ellman® (Ellman International, New York, USA) electro-surgery unit set at high power (between 6 to 9) and coagulation mode. We used a multiple pass ′fanning′ technique through single epidermal entry point. The RF probe was kept in contact with the metallic needle via the window in the plastic cannula [Figure - 4]b. This arrangement avoided thermal damage to the superficial uninvolved epidermis and dermis. Three such sessions were performed for the larger swelling over a period of four years resulting in 75-80% reduction in size. There was no increase in size between sessions and till two years after the last session. Smaller lesions showed complete subsidence after 1-2 sittings of superficial RF ablation and did not recur over the follow up period of three years. Some intra-lesional RF insertion sites healed with depigmentation [Figure - 4]c. Overall, the patient was satisfied.
 |
| Figure 1: A single 6 × 6 cm oval subcutaneous swelling over left side of forehead, at baseline. Overlying and adjacent scalp shows numerous 0.5 to 1.5 cm-sized erythematous papules and nodules |
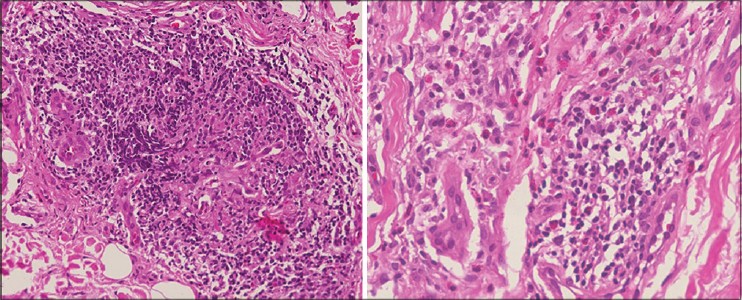 |
| Figure 2: Left image shows capillaries lined by plump 'histiocytoid' endothelial cells and surrounded by a dense aggregate of lymphocytes (H and E, ×200) Right image shows a different section with perivascular aggregate of lymphocytes admixed with numerous eosinophils and a few plasma cells (H and E, ×400) |
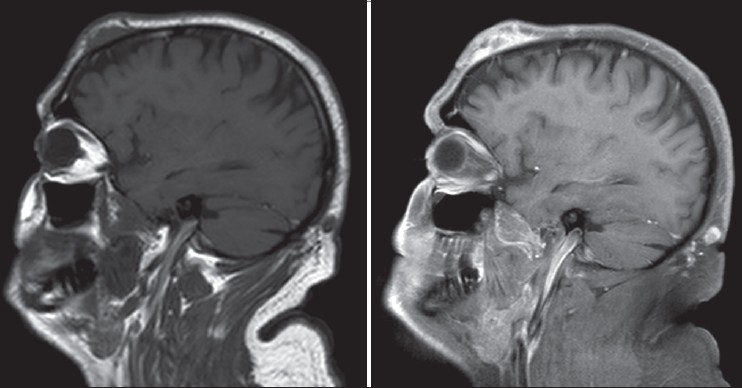 |
| Figure 3: T1W image in sagittal plane on left shows a hypo-to iso-intense soft tissue lesion in the left frontal region. A smaller lesion of similar nature is seen in the occipital region. T1W post contrast image in sagittal plane on right shows heterogenous enhancement of the left frontal and occipital scalp lesions |
 |
| Figure 4: The intra-lesional RF technique and the result, (a) An 18-gauge intravenous cannula showing a small window in its plastic sheath near proximal end of cannula near the hub. The distal 0.5 cm of the metallic needle has also been freed of the plastic (black arrows), (b) The technique-Ellman® RF probe touching the metallic needle through the window in the plastic cannula. RF coagulation is apparent by pallor and wrinkling of skin overlying the nodule, (c) Post operative photograph showing remarkable improvement two years after the 3rd sitting of intra-lesional RF for the large nodule and three years after superfi cial RF for the smaller lesions. Punctate post infl ammatory de-pigmentation is observed |
DISCUSSION
Angiolymphoid hyperplasia with eosinophilia was first described by Wells and Whimster in 1969 and despite several modalities being tried, its treatment remains unsatisfactory. Medical therapies tried so far have generally shown poor results, barring a few reports of success with systemic retinoids, topical/intra-lesional/systemic steroids, pentoxiphylline and indomethacin. Ablative/cytotoxic therapies that have been tried include surgical excision, cryotherapy, electrosurgery, laser therapy, radiotherapy and intra-lesional chemotherapy with some success. [1] More recently, a combination therapy of RF followed by sclerotherapy using 3% polidocanol was used in three cases with good results and no recurrence after 6 months to three years of follow-up. [3] Based on the small amount of available literature, some authors have recommended surgical excision as first line treatment followed by laser therapy. [1]
Since ALHE is a benign disease with the complaint mainly of a cosmetic nature, a minimally invasive approach with a good safety profile such as intra-lesional RF would be appropriate.
Intra-lesional RF is commonly used outside the domain of dermatology for various tumours (hepatic, breast and bone), varicose veins and of late in head and neck surgery as a treatment for sleep related breathing disorder. [4] These probes are designed so that the un-insulated part stays inside the area of interest and RF energy destroys it. To the best of our knowledge, there are only two reports of intra-lesional RF for dermatological indications, albeit using different techniques. Fruth et al., treated 14 patients with auricular keloids with intra-lesional RF using insulated probes and achieved good cosmetic results in ten patients, with no recurrence over a follow up period ranging from four to 66 months. [5] Huang et al., treated 64 patients with peri-orbital syringomas with RF using needle electrodes inserted in the lesions for 1-2 seconds followed by rapid withdrawal. Overall, 100% response was seen after three sessions. There was no recurrence during six months of follow-up. [6]
Post inflammatory depigmentation seen in our case might be due to superficial RF causing damage to melanocytes. Overall, our technique of intra-lesional RF is simple, novel, cost-effective, and an easily available alternative to insulated RF probes. It may be used at cosmetically important sites for various lesions not involving the epidermis, deep or subcutaneous swellings, benign dermal tumors or cysts and vascular structures. However, it is a blind procedure and cannot be done in areas where important structures like major nerves and vessels lie in the vicinity of or within the lesion.
| 1. |
Chong WS, Thomas A, Goh CL. Kimura's disease and angiolymphoid hyperplasia with eosinophilia: Two disease entities in the same patient. Case report and review of literature. Int J Dermatol 2006;45:139-45.
[Google Scholar]
|
| 2. |
Hainer BL. Electrosurgery for the skin. Am Fam Physician 2002;66:1259-66.
[Google Scholar]
|
| 3. |
Khunger N, Pahwa M, Jain RK. Angiolymphoid hyperplasia with eosinophilia treated with a novel combination technique of radiofrequency ablation and sclerotherapy. Dermatol Surg 2010;36:422-5.
[Google Scholar]
|
| 4. |
Powell NB, Riley RW, Guilleminault C. Radiofrequency tongue base reduction in sleep-disordered breathing: A pilot study. Otolaryngol Head Neck Surg 1999;120:656-64.
[Google Scholar]
|
| 5. |
Fruth K, Gouveris H, Kuelkens C, Mann WJ. Radiofrequency tissue volume reduction for the treatment of auricle keloids. Laryngoscope 2011;121:1233-6.
[Google Scholar]
|
| 6. |
Huan LP, Zhang L, Wang XL, Liu XC, Jiang TY, Lin BW. A technique for periorbital syringomas: Intra-lesional radiofrequency ablation. Int J Ophthalmol 2012;5:181-5.
[Google Scholar]
|
Fulltext Views
4,256
PDF downloads
1,930





