Translate this page into:
Isolated distal cutaneous thrombosis: An unusual presentation and an interesting etiology
2 Department of Medicine, Lady Hardinge Medical College and Smt. Sucheta Kriplani Hospital, New Delhi, India
3 Department of Pathology, Lady Hardinge Medical College and Smt. Sucheta Kriplani Hospital, New Delhi, India
Correspondence Address:
Anupam Prakash
2, Small Registrar Flats, Lady Hardinge Medical College Campus, New Delhi - 110 001
India
| How to cite this article: Mendiratta V, Prakash A, Jain A, Jain M. Isolated distal cutaneous thrombosis: An unusual presentation and an interesting etiology. Indian J Dermatol Venereol Leprol 2011;77:494-497 |
Abstract
A middle-aged hypertensive male, with a fatty liver and chronic alcohol intake, relocated to a high altitude of 2100 m above sea level; in the first winter season, he developed bluish skin lesions over the tip of the nose, margins of both ear lobes, both knees, and subungual location. Systemic examination was unremarkable. Skin biopsy showed thrombi in dermal vessels without any evidence of vasculitis; immunofluorescence was negative. Investigations revealed mild elevation in plasma homocysteine levels, weakly positive antinuclear antibodies and elevated antiphospholipid antibodies, methylene tetrahydrofolate reductase C677T heterozygosity, and protein S deficiency. The patient received prednisolone for 2 weeks, aspirin and pentoxyphylline for 3 months, and continues to be on folic acid and vitamin B6. After 3 months, antiphospholipid antibodies and antinuclear antibody levels were normal. Isolated distal cutaneous thrombosis is an uncommon entity and precipitation by extreme cold in a hypertensive male with three thrombophilic states - one transient, one hereditary, and one acquired - is fascinating.Introduction
Cutaneous lesions are a common accompaniment of thrombotic conditions. However, "isolated cutaneous thrombosis" is a very unusual presentation. In fact, purpura, vasculitis, or pseudovasculitic lesions are the commoner mimics. Diagnosis requires histological evidence of dermal vessel thrombosis in the presence of a normal vessel wall. A biopsy-proven case of "isolated distal cutaneous thrombosis" in an adult hypertensive male on exposure to extreme cold at an altitude of 2100 m above sea level is described here, in association with a peculiar combination of three thrombophilic states.
Case Report
A 55-year-male hypertensive on regular treatment, with habitual alcohol consumption on a daily basis, presented with sudden onset of painful bluish lesions over the tip of the nose, bilateral rims of ears, knees, and beneath his nails in the month of December. There was no history of prior drug intake, fever, arthritis, or headache. He used to perform a supervisory nature of work. He had relocated 6 months back to Joshimath, a hilly area of India situated 2100 m above sea level, known for its severely cold winters (temperature ranging from ?9 to +8C). Examination revealed tender, necrotizing bluish lesions on the tip of the nose and bilaterally on the ear pinnae and knees, along with subungual purpuric lesions on the left ring finger [Figure - 1]. Systemic examination, including that of the joints and mucous membranes, was unremarkable. Possibilities entertained were postinfectious vasculitis, ANCA-associated vasculitis, and cryoglobulinemia.
 |
| Figure 1: Necrotic blue cutaneous lesions affecting the pinna (a), subungual area (b), and bilateral knees (c) |
Investigations revealed Hb 15 g/dL, TLC 9690/mm 3 , platelets 239,000/mm 3 , and ESR 85 mm at the end of the first hour (Westergren) with a normocytic normochromic blood picture. Serum biochemistry revealed creatinine 0.7 mg/dL, total protein 8.7 g/L, albumin 4.1 g/L, total bilirubin 0.46 mg/dL, AST 31 U/L, ALT 23 U/L, ALP 259 U/L (normal 95-270 U/L), TSH- 2.64 IU/mL, normal lipid profile, and negative serology for HBV, HCV, and HIV. INR, aPTT, urine, and stool examination, electrocardiography, echocardiography, and chest radiograph were normal. Ultrasonography of the abdomen showed a fatty liver. Antinuclear antibodies were weakly positive by ELISA; p-ANCA, c-ANCA, antibody to double-stranded DNA and cryoglobulins were negative. Antiphospholipid antibodies were present: IgM 38.95 MPL U/mL and IgG 17.79 GPL U/mL, normal values being <10 for both.
Skin biopsy was performed from the lesions over his knee. Histopathological examination showed the presence of flattened rete ridges and a thinned out epidermis but dermal appendages were normal and there was no perivascular inflammation or inflammation of the dermis. Superficial dermis showed dilated and congested vascular channels filled with a pink fibrinous material, mixed with polymorphonuclear cells and red blood cells, obliterating the entire lumen and endothelial lining of the vessel wall, suggestive of thrombosis [Figure - 2]. Direct immunofluorescence was negative for both IgG and IgM.
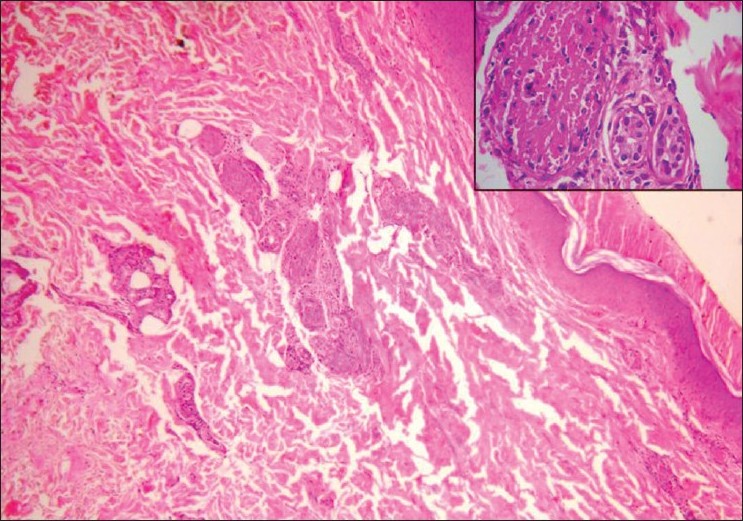 |
| Figure 2: Histopathology (H and E, ×10) demonstrating intravascular noninflammatory infiltrate. The inset shows intravascular thrombus (×40) |
Further work-up for thrombophilic states revealed the absence of Factor V Leiden R506Q, Factor V Cambridge Arg306Thr, and Factor II (prothrombin G20210A) mutations; however, MTHFR (methylene tetrahydrofolate reductase) C677T heterozygosity was detected. Functional Protein S was 56% of the normal (the normal range being 77-143) while functional protein C level was 75.2% (normal being 70-140). Plasma homocysteine levels were 16.3 ΅mol/L (normal range 6.26-15).
The patient was treated with oral prednisolone (40 mg/day) for 2 weeks while aspirin 75 mg/day and pentoxyphylline 400 mg tid were continued for a period of 12 weeks. The lesions improved gradually over 6-8 weeks and healed with scarring and hyperpigmentation. No fresh lesions appeared after relocating to plains (Delhi). After 3 months of the initial episode, antinuclear antibodies were negative, anticardiolipin antibodies had returned to normal range (IgM 4.23, IgG 4.34), and no lupus-like anticoagulant was present. The patient has been asymptomatic for a year since shifting from the high-altitude area to the plains.
The diagnostic amalgam turns out to be "hypertensive male," "isolated distal cutaneous thrombosis," "exposure to extreme cold at an altitude of 2100 m above sea level," "fatty liver superimposed over chronic alcohol intake," "hyperhomocysteinemia (HHy) associated with MTHFR C677T heterozygosity," "transient elevation of antiphospholipid antibodies," and "protein S deficiency."
Discussion
The present case has a number of unique features. Firstly, the manifestation as isolated distal cutaneous thrombosis (biopsy proven) is a rarity. In fact, it has been shown that at low temperatures, actin-related changes occur in platelets resulting in an abrupt change in their shape to spiny spheres with irregular projections which in turn promotieg platelet aggregation and thrombosis. Hence, the platelets are considered to be more activable at temperatures at the body surface than at core body temperature. [1] Extreme cold at an altitude of 2100 m above sea level therefore is one of the plausible reasons contributing to isolated distal cutaneous thrombosis, in the present case. However, the absence of any other case in that area for several years was intriguing. One characteristic factor was the presence of hypertension, since there is a definite risk of thrombosis in cold weather in hypertensives. [2]
Thrombosis is associated with a number of risk factors. Most of these risk factors cause venous thrombosis, but antiphospholipid antibody syndrome, protein C deficiency, and HHy are known to cause arteriovenous thrombosis. Distinctively, three thrombophilic states were concomitantly present in this case - transient presence of antiphospholipid antibodies, HHy secondary to the MTHFR C677T heterozygous state, and secondary protein S deficiency.
MTHFR C677T homozygous mutation has been reported to be associated with recurrent fetal loss, [3] but the heterozygous state results in mild-to-moderate HHy which can contribute to both arterial and venous thrombosis, more commonly the latter. A link with recurrent deep vein thrombosis [4] and coronary artery disease exists. [5] Interestingly, two cases of HHy presenting with isolated distal cutaneous lesions similar to the present case have been reported. [6],[7]
Antiphospholipid antibody syndrome may present as arterial and/or venous thrombosis, and dermatologic manifestations have been reported in 49% of patients and were the presenting manifestations in 30.5%. [8] Antiphospholipid antibodies syndrome associated with HHy related to MTHFR gene heterozygous mutations has been reported. [9] However, the astonishing feature in the present case was the transient elevation of antiphospholipid antibodies coinciding with the episode of thrombosis. Similar transient elevation has been observed in association with viral infections and thrombosis. [10],[11]
A diminished protein S activity can occur due to hereditary causes, hepatic damage, pregnancy, oral contraceptive use, estrogen therapy, oral anticoagulation, and treatment with l-asparaginase. The latter four causes do not stand in this case and in the presence of fatty liver and chronic alcoholism, it is likely that some amount of hepatic damage contributed to protein S deficiency.
Interestingly, four thrombophilic factors have been reported in a 72-year-female but she had three deep vein thromboses in addition to cutaneous necrosis. [12] Distinctively, isolated distal cutaneous thrombosis with three peculiar thrombophilic factors - one transient, one acquired, and the third genetic - precipitated by extreme cold at a high altitude of 2100 m, in the presence of hypertension, is an exceptional scenario with a very fascinating pathophysiology as discussed.
| 1. |
Hoffmeister KM, Falet H, Toker A, Barkalow KL, Stossel TP, Hartwig JH. Mechanisms of cold-induced platelet actin assembly. J Biol Chem 2001;276:24751-9.
[Google Scholar]
|
| 2. |
Kawahara J, Sano H, Fukuzaki H, Saito K, Hirouchi H. Acute effects of exposure to cold on blood pressure, platelet function and sympathetic nervous activity in humans. Am J Hypertens 1989;2:724-6.
[Google Scholar]
|
| 3. |
Altomare I, Adler A, Aledort LM. The 5,10 methylenetetrahydrofolate reductase C677T mutation and risk of fetal loss: A case series and review of literature. Thromb J 2007;5:17.
[Google Scholar]
|
| 4. |
Pathare A, Alkindi S, Albalushi T, Bayoumi R, Dennison D, Muralitharan S. Heterozygous methylene tetrahydrofolate reductase mutation with mild hyperhomocysteinemia associated with deep vein thrombosis. Clin Lab Haematol 2004;26:143-6.
[Google Scholar]
|
| 5. |
Varga EA, Sturm AC, Misita CP, Moll S. Homocysteine and MTHFR mutations: Relation to thrombosis and coronary artery disease. Circulation 2005;111:e289-93.
[Google Scholar]
|
| 6. |
Didier AF, Tourand JP, Collet E, Dalac S, Becker F, Lambert D. Distal cutaneous necrosis, an unusual etiology: Hyperhomocysteinemia. Ann Dermatol Venereol 1999;126:822-5.
[Google Scholar]
|
| 7. |
Boeckler P, Grange F, Krzisch S, Grosshans E, Guillaume JC. Acral purpura and hyperhomocysteinemia. Ann Dermatol Venereol 2003;130:542-5.
[Google Scholar]
|
| 8. |
Frances C, Niang S, Laffitte E, Pelletier F, Costedoat N, Piette C. Dermatologic manifestations of the antiphospholipid syndrome: Two hundred consecutive cases. Arthritis Rheum 2005;52:1785-93.
[Google Scholar]
|
| 9. |
Nucera C, Vaccaro M, Moleti M, Priolo C, Tortorella G, Angioni A, et al. Antiphospholipid antibodies syndrome associated with hyperhomocysteinemia related to MTHFR gene C677T and A1298C heterozygous mutations in a young man with idiopathic hypoparathyroidism (DiGeorge syndrome). J Clin Endocrinol Metab 2006;91:2021-6.
[Google Scholar]
|
| 10. |
Tanizawa K, Nakatsuka D, Tanaka E, Inoue T, Sakuramoto M, Minakuchi M, et al. Pulmonary thrombosis with transient antiphospholipid syndrome after mononucleosis-like illness. Intern Med 2009;48:1231-4.
[Google Scholar]
|
| 11. |
Toyoshima M, Maegaki Y, Yotsumata K, Takei S, Kawano Y. Antiphopspholipid syndrome associated with human herpes virus-6 infection. Pediatr Neurol 2007;37:449-51.
[Google Scholar]
|
| 12. |
Combemale P, Amiral J, Estival JL, Dupin M, Chouvet B, Berruyer M. Cutaneous necrosis revealing the coexistence of an antiphospholipid syndrome with acquired protein S deficiency, factor V Leiden and hyperhomocysteinemia. Eur J Dermatol 2002;12:278-82.
[Google Scholar]
|
Fulltext Views
2,662
PDF downloads
2,156





