Translate this page into:
Isolated unilateral palisaded neutrophilic and granulomatous dermatitis
Correspondence Address:
Rameshwar Gutte
Department of Dermatology, Seth GS Medical College and KEM Hospital, Parel, Mumbai 400 012
India
| How to cite this article: Gutte R, Khopkar U. Isolated unilateral palisaded neutrophilic and granulomatous dermatitis. Indian J Dermatol Venereol Leprol 2011;77:615-617 |
Sir,
Palisaded neutrophilic and granulomatous dermatitis (PNGD) is a rare entity that has not been clearly defined either histopathologically or clinically. [1] It usually presents as asymptomatic to painful papulonodular lesions with predilection for extensor aspect of joints. [2],[3] PNGD, though usually associated with systemic disease, we encountered a case without any underlying disease.
Our patient, a 21-year-old unmarried male presented with asymptomatic skin colored raised lesions around left elbow since 2 months. There was no history of trauma, prior drug intake, ulceration, or discharge from the lesions. He denied history of any soy product intake. There was no history of photosensitivity, breathlessness, Raynaud′s phenomenon, muscle weakness, joint pain or swelling, fever, weight loss, loss of appetite, per rectal bleeding, or any other symptom suggesting systemic disease.
Examination revealed multiple skin colored to brownish, nontender, indurated papules, and nodules around left elbow with peau-de-orange appearance [Figure - 1]. Joint movements were normal and there were no other skin lesions. No lymphadenopathy was seen. Systemic examination was also normal.
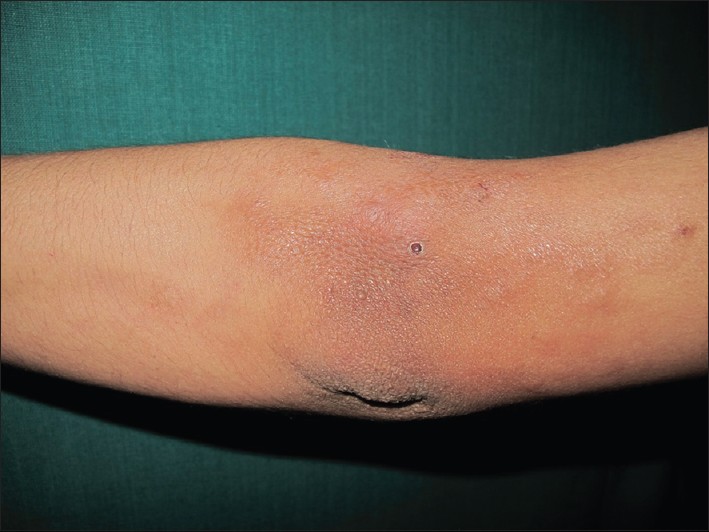 |
| Figure 1: Multiple skin colored to brownish papulonodular lesions around left elbow with post-biopsy crusting |
Based on history and examination, a differential diagnosis of, panniculitis, morphea, and deep fungal infection was thought.
Histopathologic examination showed normal epidermis and granulomatous inflammation throughout the dermis. Granulomas were made up of histiocytes and a few lymphocytes, neutrophils with histiocytic palisades around degenerated collagen. There were also intact neutrophils and nuclear dust with moderate fibrin deposition within walls of small vessels and thickened collagen at places with linictal in lower dermis [Figure - 2]. Alcian blue stain at pH 2.5 confirmed interstitial mucin deposition [Figure - 3]. On clinicopathological correlation, a diagnosis of neutrophilic palisaded and granulomatous dermatitis, well developed stage was made.
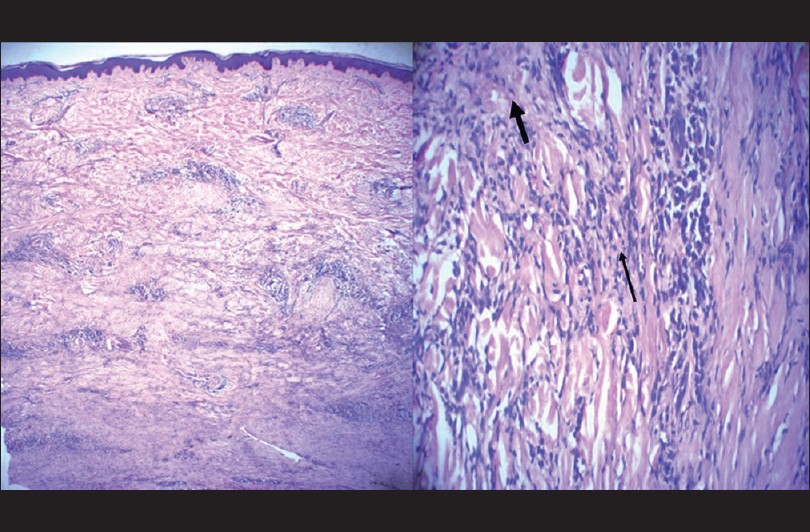 |
| Figure 2: Skin biopsy showing normal epidermis and nodular infiltrates in the dermis with scant mucin (H and E, ×25) Neutrophilic dust and intact neutrophils along with degenerated collagen, fibrin, and mucin surrounded by the palisades of histiocytes (H and E, ×200) |
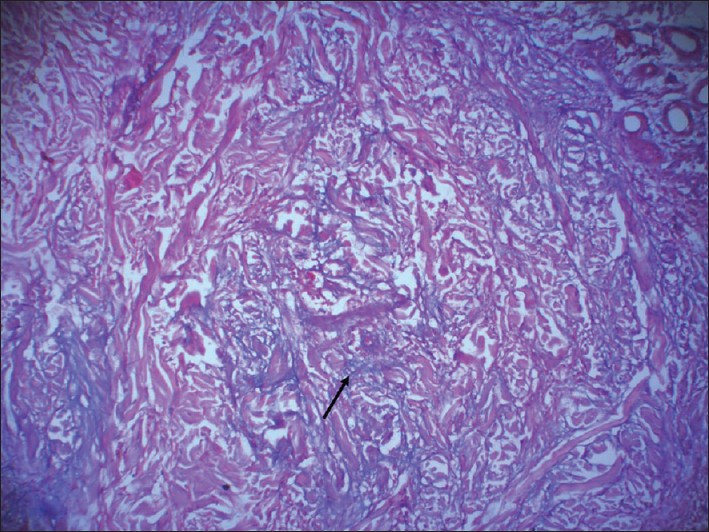 |
| Figure 3: Alcian blue stain at pH 2.5 showing bluish stringy mucin deposited interstitially (Alcian blue, ×200) |
The patient was investigated for underlying systemic cause. On investigations, we found hemoglobin 14.4 g%, with normal complete and differential blood count, erythrocyte sedimentation rate of 15 mm at the end of one hour, normal liver and kidney function tests, thyroid profile (T3, T4, and thyroid stimulating hormone), and blood sugars. Ultrasound examination of the abdomen and radiograph of left elbow joint was normal. Antinuclear antibodies, anti-dsDNA antibodies, rheumatoid factor, and ELISA for human immunodeficiency virus antibodies turned negative. Urine and stool examination was normal as also muscle enzymes and anti-streptolysin-o antibody titre. No underlying cause could be found in our patient.
The patient was prescribed tablet dapsone 100 mg per oral daily at nighttime along with potent topical steroid cream and is under follow up.
Palisaded neutrophilic and granulomatous dermatitis (PNGD) is an umbrella term proposed by Chu et al, to encompass clinical and histological spectrum of disorders such as rheumatoid nodules, interstitial granulomatous dermatitis with arthritis, Churg-Strauss granuloma and superficial ulcerating rheumatoid necrobiosis. [2],[4]
Clinically, it usually presents with lesions that are distributed often symmetrically. Overlying epidermis may be normal. [1],[4],[5] Most commonly lesions are seen over distal upper extremity or fingers, though other sites such as thighs, trunk, and lower back are known to be affected. [1] Most of the patients are asymptomatic but pain, tenderness, or itching may occur. The condition may persist indefinitely. [1],[4]
Various associations of PNGD include connective tissue disorders, such as rheumatoid arthritis, diabetes, thyroid dysfunction, systemic vasculitis, lympho-proliferative diseases, inflammatory bowel disease, Wegner′s granulomatosis, Behcet′s disease, sarcoidosis, and infective endocarditis. [1],[2],[5] Misago et al, [3] have reported a 60-year-old lady with PNGD presenting as multiple tender nodules involving both upper and lower extremities without any underlying cause.
Histologically PNGD shows three patterns with sometimes overlapping features, depending on age of the lesions. Early lesions show leucocytoclastic vasculitis like changes, fully developed lesions resemble granuloma annulare and at the other end of the process, it resembles necrobiosis lipoidica. [2],[4] Thus histopathology differs at each stage leading to a long list of differential diagnoses such as vasculitis, interstitial granuloma annulare, interstitial granulomatous dermatitis with/without arthritis, etc., and clinicopathological correlation is needed to make the diagnosis.
Various treatment modalities tried include oral steroids, dapsone, colchicine, cyclosporine, cyclophosphamide, hydroxychloroquine, and nonsteroidal anti-inflammatory agents with variable success rate. Oral steroids appear to be the most beneficial therapy. [1],[4]
We believe PNGD in our patient may represent a premonitory sign of occult systemic disease, which may appear later, and thus long-term follow up is warranted.
| 1. |
Heidary N, Mengden S, Pomeranz MK. Palisaded neutrophilic and granulomatous dermatosis. Dermatol Online J 2008;14:17.
[Google Scholar]
|
| 2. |
Ko CJ, Glusac EJ, Shapiro PE. Noninfectious granulomas. In: Elder DE. Editor. Lever's Histopathology of the skin, 10 th ed. India: Wolters Kluwer Publishing; 2009. P. 361-87.
th ed. India: Wolters Kluwer Publishing; 2009. P. 361-87.'>[Google Scholar]
|
| 3. |
Misago N, Shinoda Y, Tago Mnarisawa Y. Palisaded neutrophilic granulomatous dermatitis with leukocytoclastic vasculitis in a patient without any underlying systemic disease detected to date. J Cutan Pathol 2010;37:1092-7.
[Google Scholar]
|
| 4. |
Al-Daraji WI, Coulson IH, Howat AJ. Palisaded neutrophilic and granulomatous dermatitis. Clin Exp Dermatol 2005;30:578-9.
[Google Scholar]
|
| 5. |
OP, Caudell MD, Mengesha YM, Davis LS, Barnes CJ, Griffin JE, et al. Palisaded neutrophilic granulomatous dermatitis in rheumatoid arthritis. J Am Acad Dermatol 2002;47:251-7.
[Google Scholar]
|
Fulltext Views
4,439
PDF downloads
2,498





