Translate this page into:
Keloidal atypical fibroxanthoma on the back of an 80-year-old man, pitfalls in the clinical and histological diagnosis
Correspondence Address:
Chiu Cheng-Sheng
Department of Dermatology, Chang Gung Memorial Hospital, 199, Tun Hwa North Road, Taipei 105
Taiwan
| How to cite this article: Yi-Hsin H, Cheng-Sheng C. Keloidal atypical fibroxanthoma on the back of an 80-year-old man, pitfalls in the clinical and histological diagnosis. Indian J Dermatol Venereol Leprol 2012;78:409 |
Sir,
Keloidal atypical fibroxanthoma (AFX) is a new and under-recognized histological variant of AFX. We, herein, report a case of a keloidal AFX with the unusual presentation of a rapid growing, ulcerative plaque on the back of an 80-year-old male.
An 80-year-old man presented with an asymptomatic, rapid growing, infiltrating erythematous plaque on his back for 3 months. He denied previous trauma in this area. There was no constitutional symptoms such as fever or weight loss. Clinical examination revealed a 7 × 5 cm, ill-defined, firm and violaceous plaque on the lower back. Overlying epidermis was erosive and crusted [Figure - 1]. Lymph node examinations revealed no neck, axillary or inguinal lymphadenopathy. Other physical, examinations showed no abnormal findings. His comorbidities included Parkinsonism, hypertension and hyperlipidemia. A squamous cell carcinoma was clinically suspected and an incisional biopsy on the plaque was performed. Histopathological findings revealed a poor circumscribed, hypercellular tumor extending deeply into the reticular dermis [Figure - 2]a. The lesion revealed diffuse infiltration of pleomorphic spindle cells around prominent keloidal broad collagen fibers. The neoplastic cells demonstrated prominent atypia with bizarre, large hyper chromatic nuclei and numerous mitotic Figures [Figure - 2]b. Some larger tumor cells contained cytoplasmic hyaline globules with hemosiderin granules [Figure - 2]c. Tentative pathological diagnosis was sarcomatoid pleomorphic tumor. Immuonohistochemical study was performed for further differential diagnosis.
 |
| Figure 1: A 7 � 5 cm, ill-defined, erythematous to violaceous plaque on the back with surface erosion |
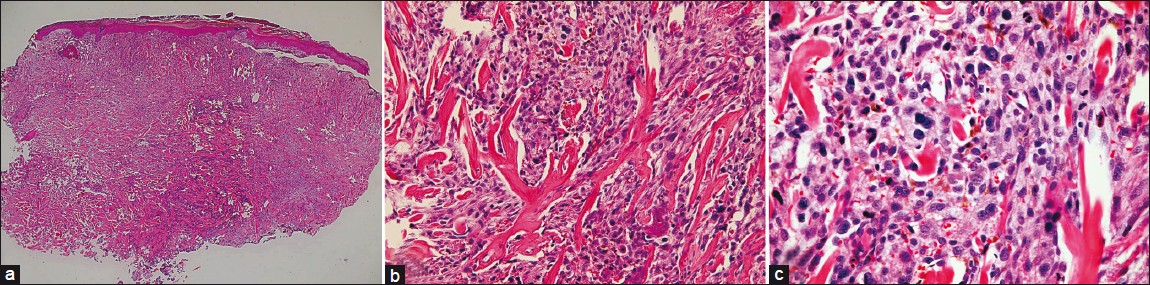 |
| Figure 2: (a) Low power field revealed a poor circumscribed, hyper-cellular tumor extending deeply into the reticular dermis (H and E, ×40), (b) The lesion revealed diffuse infiltration of pleomorphic spindle cells around prominent keloidal broad collagen fibers. The neoplastic cells demonstrated prominent atypia with bizarre, large hyper chromatic nuclei. and numerous mitotic Figures (H and E, ×100). (c) Some larger tumor cells contained cytoplasmic hyaline globules with hemosiderin granules (H and E, ×400) |
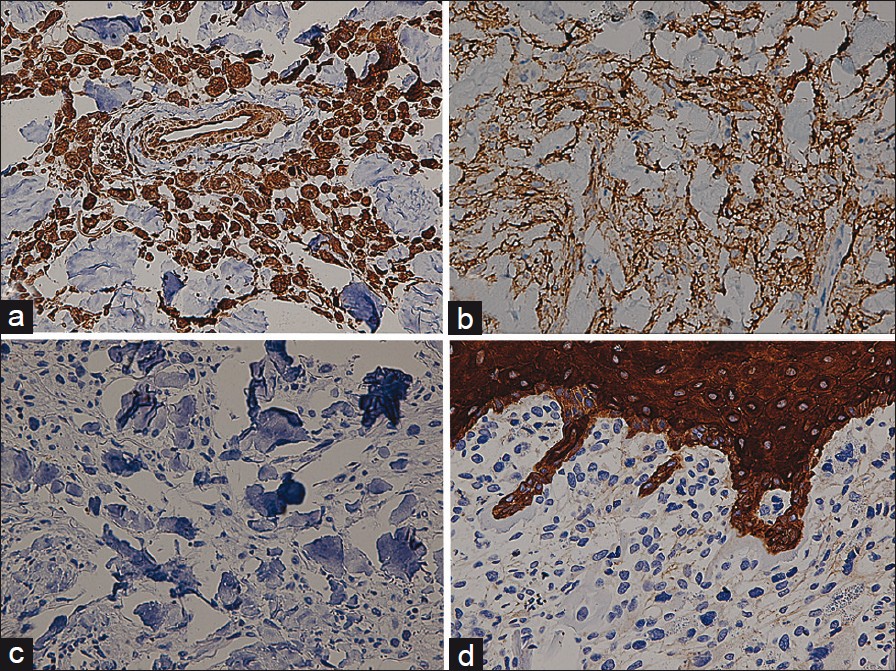 |
| Figure 3: (a and b) Immunohistochemical features: Most spindle cells expressed Vimentin (a) and CD10 (b) (×400). (c and d) Negative S100 (c) and Pancytokeratin (d) immunohistochemical staining presented throughout the neoplasm (×400) |
AFX, a pleomorphic fibrohistiocytic tumor, develops prominently on actinically damaged skin on the head and neck of elderly. Clinically, AFX begins as a rapid growing, solitary erythematous nodule and may be ulcerated. There are bimodal distribution of anatomical location and age of AFX. [1] Most of the patients are in the 7 th -8 th decade and present with AFX on the face and neck, indicating previous solar damage. Conversely, smaller group of patients present in their 4 th -5 th decade with AFX on the trunk and limbs without prominent actinic damage. [2] Our case is unique with the presentation of a keloidal AFX on the back, an uncharacteristic location for his demographic group, which raises the clinical diagnostic difficulties.
Histologically, AFX was characterized by sarcomatous appearance of mixed spindle and bizarre pleomorphic cells with evident mitoses and xanthomatous histiiocytes. [3] Histological variants of AFX included tumors with pigment, clear cell change, granular cell change, osteoclast-like giant cell and keloidal changes.
Keloidal AFX, first formally described in 2009, [3] is an unusual and under-recognized histological variant. Typical keloidal AFX is characterized by atypical pleomorphic fibrohistiocytic cells trapped within interstitial thick, glassy, eosinophilic collagen throughout the majority of the tumor. Occasionally, the keloidal collagen distribute around ring-shaped vascular structures. [4]
Clinical differential diagnosis of our case includes squamous cell carcinoma, metastatic carcinoma, melanoma or sarcoma. Histologically, pleomorphic spindle cells with keloidal collagens result in diagnostic challenges in the classical histopathological study. Further immunohistochemistry techniques are required to exclude malignant and benign neoplasm with keloidal change and dermatofibroma with monster cell. AFX typically expresses Vimentin, CD10, CD68 and CD99. Lack of S100 staining distinguishes the lesion from desmoplastic melanoma. Absence of pancytokeratin and desmin staining differentiate AFX from spindle cell squamous cell carcinoma and metastatic leiomyosarcoma, respectively. [4] Dermatofibroma with monster cell can be excluded upon negative staining of factor XIIIa.
The presence of keloidal collagen in AFX does not influence the clinical prognosis. [3] In spite of the highly atypical cytological appearance, general prognosis of AFX is good. Local recurrence is reported in 5% of the patient but metastases are exceptional. [5] Surgical excision is the main treatment strategy. In poorly circumscribed tumors with infiltrative border, excision with wider margin is suggested to avoid recurrence. Mohs surgery has been recommended by case series as a favorable method to optimize cosmetic outcome and decrease the recurrence rate. [4],[5]
With the combination of unusual clinical presentation and prominent keloidal collagen in highly anaplastic histological appearance, misdiagnosis may result in unnecessary evaluation and overextensive surgical intervention. This case highlights the integration of clinical, histological and immunohistochemical features to correctly diagnose keloidal AFX. Regardless of lesion location and patient age, keloidal AFX should always be taken into differential consideration when encountering plemorphic spindle cell tumors containing keloidal collagen.
| 1. |
Fussell JN, Cooke ER, Florentino F, Sheehan DJ. Atypical fibroxanthoma with keloidal collagen. Am J Dermatopathol 2010;32:713-5.
[Google Scholar]
|
| 2. |
Kim J, McNiff JM. Keloidal atypical fibroxanthoma: A case Series. J Cutan Pathol 2009;36:535-9.
[Google Scholar]
|
| 3. |
Offman S, Pasternak S, Walsh N. Keloidal and other collagen patterns in atypical fibroxanthomas. Am J Dermatopathol 2010;32:326-32.
[Google Scholar]
|
| 4. |
Davis JL, Randle HW, Zalla MJ, Roenigk RK, Brodland DG. A comparison of Mohs micrographic surgery and wide excision for the treatment of atypical fibroxanthoma. Dermatol Surg 1997;23:105-10.
[Google Scholar]
|
| 5. |
Cooper JZ, Newman SR, Scott GA, Brown MD. Metastasizing atypical fibroxanthoma (cutaneous malignant histiocytoma): Report of five cases. Dermatol Surg 2005;31:221-5.
[Google Scholar]
|
Fulltext Views
1,300
PDF downloads
1,559





