Translate this page into:
Keloidectomy with core fillet flap and intralesional verapamil injection for recurrent earlobe keloids
Correspondence Address:
Mohammed Fawzy El-Kamel
Department of Dermatology, Andrology and STDs, Mansoura University, Mansoura 35516
Egypt
| How to cite this article: El-Kamel MF, Selim MK, Alghobary MF. Keloidectomy with core fillet flap and intralesional verapamil injection for recurrent earlobe keloids. Indian J Dermatol Venereol Leprol 2016;82:659-665 |
Abstract
Background: Earlobe keloids are usually recalcitrant to treatment and have a high rate of recurrence. Verapamil is a calcium channel antagonist that has been shown to inhibit the synthesis/secretion of extracellular matrix molecules and increase collagenase. Objectives: This prospective study was designed to evaluate the results of treatment of recurrent earlobe keloids using keloidectomy with core fillet flap and intralesional verapamil injection. Methods: Nineteen keloids in 16 patients were treated using this technique with intralesional verapamil injection given intraoperatively, then every 2 weeks for 3 months, with postoperative follow-up for 18 months. Results: Fourteen patients completed the study. Ten patients (71.4%) showed response to treatment. Four (28.6%) cases showed recurrence, two (14.2%) at the wound bed and another two (14. 2%) at the incision line. Eighty percent of responders were highly satisfied with their treatment. Conclusion: Keloidectomy with core fillet flap and intralesional verapamil injection is a reliable and cost-effective method in the treatment of recurrent earlobe keloids with a low rate of recurrence and high patient satisfaction.Introduction
The result of wound healing is the formation of a scar at the site of tissue disruption. The rate and quality of scar formation varies among individuals. Alterations in this process may result in the development of a chronic wound or an abnormal scar. Keloids are hypertrophic-appearing scars that continue to evolve over time without a quiescent or regressive phase in the process of wound healing.[1],[2] They are benign hyperproliferative growths of dermal collagen that usually result from excessive tissue response to skin trauma.[3]
Keloids may occur anywhere, but the most common locations are the shoulder, presternal area, neck and upper arms.[4] In the head and neck region, these lesions are especially conspicuous and patients typically present with cosmetic concerns. Earlobes and helix of the auricle are common sites for keloid formation, usually following trauma or ear piercing, with an incidence of approximately 2.5 per cent [5] Due to the practice of ear piercing, younger women have a higher incidence of keloids than men. People over 65 years of age seldom develop keloids.[3]
There are numerous treatment modalities available to treat earlobe keloids which confirm the resistant nature and likely multifactorial etiology of these lesions. Their successful treatment thus requires the use of more than one treatment to effect a good result.[6] Available options include excision, intralesional steroids, radiotherapy, pressure, cryotherapy and imiquimod 5% cream.[7]
Excisional surgery tends to be useful as a part of a multitreatment approach. Reconstruction is undertaken with any of the usual modalities: healing by secondary intention, primary closure, skin grafting or flaps. Use of a “keloid fillet flap” enables dissection of the keloid core leaving loose skin to effect closure while an island flap uses skin bordering the defect.[8],[9] Decreased recurrence rates have been reported with excision in combination with other postoperative modalities such as radiotherapy, injected interferon (IFN) or corticosteroid therapy. Excisional surgery alone has been shown to yield a 45–100% recurrence rate.[10],[11]
Verapamil hydrochloride is a widely used calcium channel antagonist which inhibits the synthesis/secretion of extracellular matrix molecules including collagen, glycosaminoglycans and fibronectin while increasing collagenase.[12] Intralesional verapamil has shown promising results in non-randomized early clinical trials as an adjuvant after surgery, or alone.[13]
The aim of this study was to determine the effectiveness of verapamil hydrochloride as an adjunct measure after keloidectomy with core fillet as a treatment protocol for recurrent earlobe keloids and to assess patient satisfaction with treatment.
Methods
This study included 19 recurrent earlobe keloids in 16 women who were seen during the period from January 2010 to November 2011. Patients were referred from general practitioners and from general dermatology outpatient clinics, Mansoura University Hospitals to the dermatosurgery unit for further evaluation and management.
Inclusion criteria included mentally stable adult patients over 18 years of age, complaining of recurrent earlobe keloid(s), who had not received any treatment within the last 6 months and were available for follow-up at regular intervals for 18 months. Exclusion criteria were patients with skin phototype VI, systemic illnesses such as uncontrolled diabetes mellitus, mental disorders, cancer and cardiac disease, bleeding tendencies or those on anticoagulant medication, systemic isotretinoin therapy within the last 6 months and pregnant and lactating women, Written informed consent was provided by all participants before inclusion. Serial photography for each patient was taken preoperatively, intraoperatively and then every 2 months until the end of the follow-up period.
All patients underwent keloidectomy and core fillet flap according to the technique of Kim et al.[8] briefly described below and received adjuvant intralesional verapamil hydrochloride injection. Postoperatively, the surgical site was evaluated for response to treatment and occurrence of any complications. The main outcome was absence of keloid recurrence. The occurrence of complications at the surgical site was also assessed. Keloid formation at the surgical incision site was defined according to Davison et al., as any exuberant scar that extended 5 mm beyond the surgical incision.[14]
Technique
Surgery was performed in a minor surgical theater. The flap was marked so that the pedicle was toward the free edge of the earlobe and the line of incision close to the retroauricular crease, if the keloid was on the posterior aspect of earlobe, since it would be more cosmetically acceptable. If the keloid was on the anterior aspect of the earlobe, the flap was marked so that the pedicle was in the posterior position. A local anesthetic (2% lidocaine with 1:100,000 epinephrine) was infiltrated at the surgical site, after delineation of the line of incision so that borders of the mass were not obscured. Then, the cutaneous compartment was separated from the main keloidal mass using a curved blunt iris scissor until the keloid mass was completely separated, with normal skin all around. A sharp tipped scissor was used to separate the mass from its bed without perforating normal skin on either side. If perforation occurred, it was closed using nylon 5-0 interrupted sutures [Figure - 1], [Figure - 2], [Figure - 3], [Figure - 4], [Figure - 5].
 |
| Figure 1: A 19-year-old woman with sessile right earlobe keloid before treatment with marking at the site of incision |
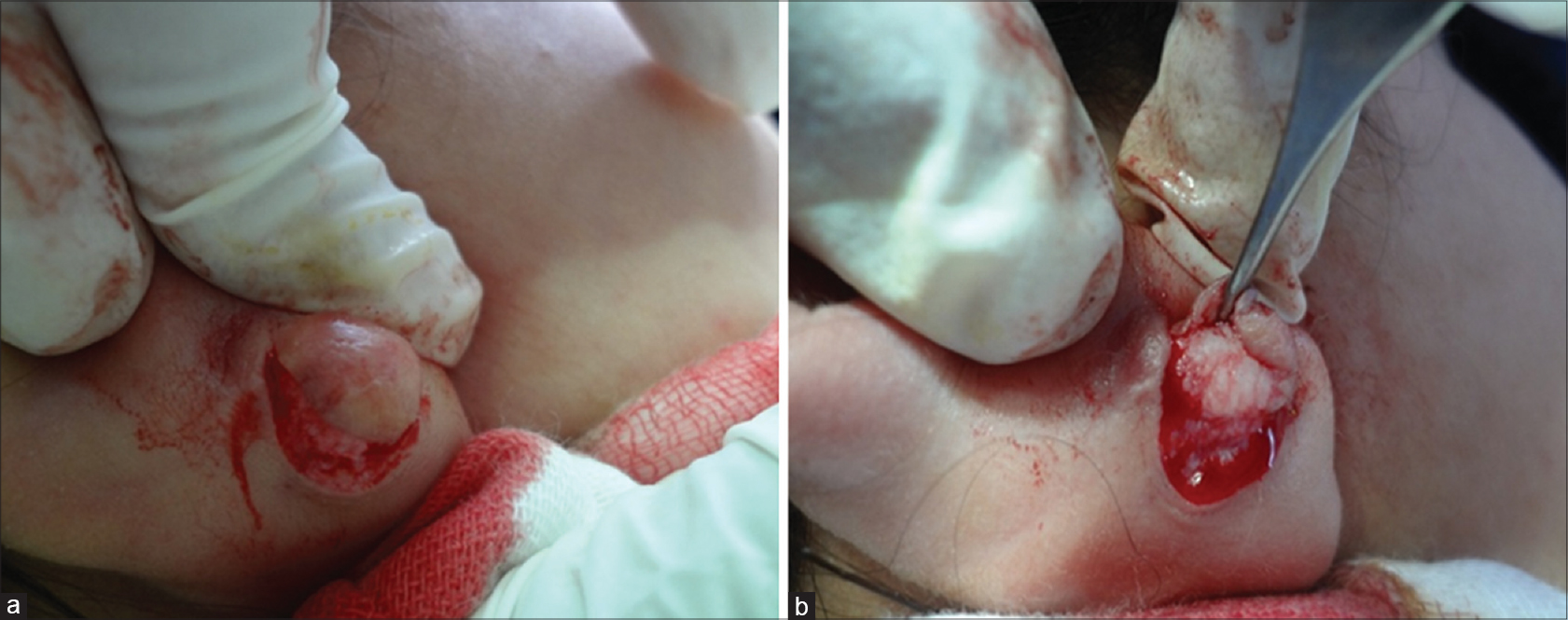 |
| Figure 2: (a and b) Intraoperative appearance during elevation of the flap and keloidectomy |
 |
| Figure 3: A 19-year-old woman 9 months postoperative |
 |
| Figure 4: A 35-year-old woman with pedunculated right earlobe keloid before treatment |
 |
| Figure 5: A 35-year-old woman intraoperative |
Bleeding was controlled by pressure. Electrocautery to control bleeding was used only if essential, to avoid possible flap necrosis. If there was a keloidal tract reaching the other skin side, which represented the site of ear piercing, it was excised using punches according to the size of the tract and then closed with nylon 5-0 sutures. The skin flap was laid down on the underlying tissues for closure, after trimming of excess skin. Before proceeding to wound closure, meticulous palpation of the wound all around and also the bed was done to make sure that there was no residual fibrous tissue. Closure was done using nylon 5-0 or 4-0 interrupted sutures. Subcutaneous sutures were not used. A pressure dressing was applied and sutures were removed 14 days later.
Verapamil hydrochloride (2.5 mg/ml) was injected locally, intraoperatively before application of the pressure dressing, then postoperatively every 2 weeks for 1 month, then monthly for 3 months. The injection was given along suture lines and also into the wound bed. The injected volume ranged from 1 ml up to 2.5 ml per sitting, according to the size of the wound.
Excised keloids were sent for histopathological confirmation. All patients, excepting two, were followed up for 18 months after surgery.
Results
This study included 16 patients with 19 recurrent earlobe keloid(s). [Table - 1] shows patient data and results of treatment.
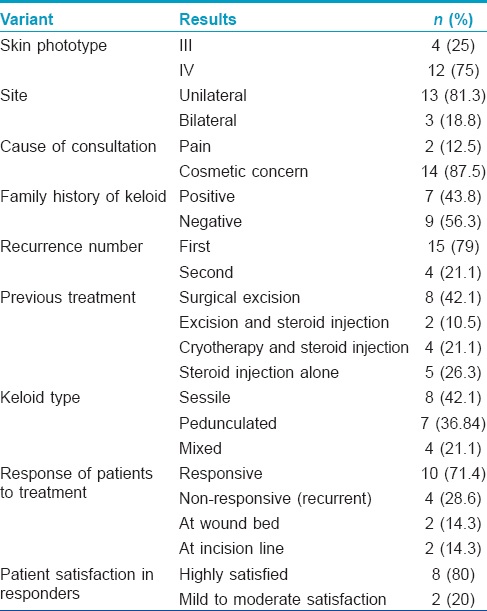
All patients were women and developed their lesions after cosmetic earlobe piercing. The lesions were unilateral in 13 (81.3%) patients and bilateral in three (18.8%) patients. The patients ranged in age from 18 to 48 years. The most common reasons for seeking medical advice were the cosmetic appearance in 14 (87.5%) patients and pain in two (12.5%) patients. The skin phototype was Type IV in 12 (75%) patients and Type III in four (25%) patients. The duration of the latest recurrence ranged from 2 years up to 9 years (average 4.57 years). A family history of keloids was present in seven (43.8%) patients.
Fifteen (79%) keloids were first recurrences and 4 (21.1%) were recurrent for the second time. The recurrence occurred after surgical excision in eight (42.1%) patients, after combined excision and postoperative local corticosteroid injection in two (10.5%) patients, after combined cryotherapy and local corticosteroid injection in four (21.1%) patients and after intralesional corticosteroid injection in five (26.3%) patients.
According to the modified Chang-Park classification, the most common type of keloid was sessile eight lesions (42.1%), followed by the pedunculated type, seven lesions (36.8%) and mixed type, four lesions (21.1%).[15] One patient with bilateral sessile keloids and another patient with a unilateral mixed keloid were lost to follow-up after a period of 12 months and 10 months respectively.
Among the 16 cases that were included, 14 patients with 17 keloids completed the study. The response was evaluated separately by two investigators for the development of recurrence and occurrence of complications on each visit. Ten (71.4%) patients showed response to treatment with no evidence of recurrence. Two (14.3%) patients with three keloids showed recurrence at the wound bed (two sessile, one mixed). Another two (14.3%) patients developed a hypertrophic scar along the incision line. Although this developed away from the site of the original keloid, it was also considered a recurrence.
Of the recurrent keloids at the wound bed, two recurred immediately within three months of operation these were of the sessile type. Another one recurred late, after 12 months, and was of the mixed type. Interestingly, all of these occurred in keloids that recurred for the second time after surgical excision and in patients whose skin phototype was Type IV.
Complications encountered were a partial flap tip necrosis in two (10.5%) keloids. Flap necrosis was limited and healed completely with conservative treatment. There was neither atrophy nor pigmentary change at the surgical site and no hematoma. Among the 10 cases that showed response, 8 (80%) cases expressed a high degree of satisfaction and 2 (20%) cases were moderately to mildly satisfied with the result.
Discussion
Keloids are only found in humans and occur in 5–15% of wounds.[16] They tend to affect both sexes equally, although a higher incidence of women presenting with keloids has been recorded, possibly secondary to cosmetic implications associated with disfigurement.[17]
Once they have formed, there is no single completely satisfactory treatment for keloids. The most important thing to consider in the management of keloids is prevention. No single therapeutic modality has been determined experimentally to be the most effective for treating keloid scars.[18] In this clinical study, we used verapamil hydrochloride injections after keloidectomy and reconstruction with the use of a keloid fillet flap, which was done by the technique of Kim et al.[8]. in an attempt to reduce the rate of recurrence in such stubborn recurrent earlobe keloids. We performed keloid removal by this technique because it avoids risk factors responsible for keloid recurrence which are the “Five As and one B” (Asepsis, Atraumatic technique, Absence of raw surface, Avoidance of tension, Accurate approximation of wound margin and complete Bleeding control).[8]
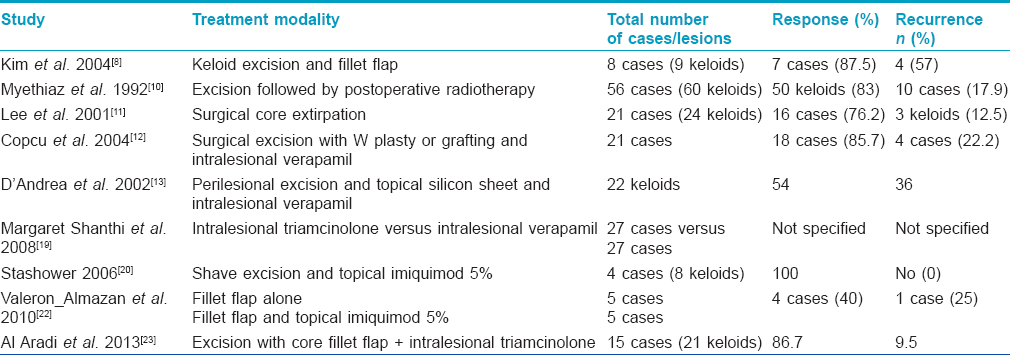
In this study, we found that keloids in 10 (71.4%) patients responded to the treatment protocol with no evidence of recurrence during the follow-up period and four (28.6%) patients showed recurrence. Copcu et al. performed total keloid excision in combination with reconstruction with W-plasty or skin grafting and injection of verapamil hydrochloride into the lesions of 21 patients with keloids.[12] They found a recurrence rate of 19.04% in a follow-up period of 2 years. Stashower stated that the treatment of earlobe keloids has historically been suboptimal and characterized by discomfort, poor response and high rates of recurrence.[20] Hence, when taking into consideration the higher recurrence rate of earlobe keloids in comparison to keloids at other locations, it seems that our treatment protocol is more promising than that of Copcu et al., with lower rates of relapses.[12]
Lawrence treated 31 patients with 40 earlobe keloids using surgical excision plus adjuvant intralesional verapamil and pressure earrings.[21] Minimum follow-up was 6 months and average follow-up was 28 months. Twenty two keloids in 16 patients with 45 earlobe keloids were cured by this treatment protocol. His results showed a much higher recurrence rate of 51.1% in comparison to our results. He found no significant differences in recurrence rates related to sex, age, keloid size, length of time the keloid was present, how long the ears had been pierced and how many verapamil injections were received.
As established from previous studies, excisional surgery alone has been shown to yield a 45–100% recurrence rate while decreased recurrence rates have been reported with excision combined with other postoperative modalities including injections of corticosteroids.[10],[11] Margaret Shanthi et al. concluded that intralesional verapamil may be a suitable alternative to triamcinolone in the treatment of hypertrophic scars and keloids with significant improvement of all clinical parameters of the scars that were investigated.[19] Our results show that verapamil injections after keloid removal were effective, and more importantly, significantly prevented recurrences.
Valerón-Almazán et al. achieved a response rate of 40% in the treatment of relapsing keloid of the pinna by a fillet flap procedure.[22] They concluded that it may be an alternative within the therapeutic arsenal for the treatment of relapsing keloid of the pinna, given that it does not require extensive resources and the skills needed to perform the procedure can be quickly acquired. These responses are significantly poorer in comparison to ours which may be due to the the additive effect of postoperative verapamil injections in our study.
Al Aradi et al. in a pilot study had treated 21 earlobe keloids using keloidectomy with core fillet flap and intra- and post-operative intralesional steroid injections.[23] The mean follow-up was 21.9 months with a clinical outcome efficacy of 87.6% and an immediate recurrence rate of 9.5 per cent. Subjectively, 82.3% of patients were highly satisfied. They recommended that this approach should be considered for the treatment of this difficult condition. The recurrence rate among their patients was slightly lower (12.4%) when compared to our results.
In this study, we found that recurrent keloids belonged to sessile and mixed type and none of the pedunculated type showed a recurrence. These findings were in agreement with Park et al. and Copcu et al. who conducted a retrospective study on 15 patients of auricular keloids and found that sessile type keloids were most likely to recur after surgical intervention.[12] Hence, clinical classification of keloidal lesions before management can assist the surgeon to predict the possibility of recurrence, especially before surgical intervention. [Table - 2] shows a summary of the results of other studies on treatment of keloids.
Complications of our treatment protocol were partial flap tip necrosis in two (10.5%) keloids and hypertrophic scar at the line of surgical incision in another two (10.5%) keloids. All complications were treated effectively with cosmetically acceptable outcomes. We found no adverse effects related to administration of verapamil injections and complications similar to those which can occur with local steroid injections, viz., atrophy, telangiectasia and pigmentary changes, were not seen. Eighty per cent of responders expressed high global subjective patient satisfaction with the results and 20% were moderately to mildly satisfied.
Limitations
Our study had two main limitations. The first was the relatively short follow-up period of 18 months and the second was the low number of cases. A longer follow up and more cases would have given more validity to this study.
Conclusion
Earlobe keloid treatment is challenging, especially in recurrent lesions. Our suggested treatment protocol is easy to do and cost-effective, with an acceptably low recurrence rate. Complications are infrequent and can be treated easily and effectively. Adjuvant postoperative verapamil injection is well tolerated and avoids the possible adverse reactions of local steroid injections. Furthermore, we achieved high global subjective patient satisfaction, which may be difficult to achieve in such stubborn recurrent keloids, especially at difficult to treat sites such as earlobes. We recommend more studies with larger number of patients to compare this treatment protocol against the same surgical technique without injection, or in combination with intralesional steroid injection.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Slemp AE, Kirschner RE. Keloids and scars: A review of keloids and scars, their pathogenesis, risk factors, and management. Curr Opin Pediatr 2006;18:396-402.
[Google Scholar]
|
| 2. |
English RS, Shenefelt PD. Keloids and hypertrophic scars. Dermatol Surg 1999;25:631-8.
[Google Scholar]
|
| 3. |
Kelly AP. Medical and surgical therapies for keloids. Dermatol Ther 2004;17:212-8.
[Google Scholar]
|
| 4. |
Ceovic R, Lipozencic J, Bukvic Mokos Z, Stulhofer Buzina D, Kostovic K. Why don't we have more effective treatment for keloids? Acta Dermatovenerol Croat 2010;18:195-200.
[Google Scholar]
|
| 5. |
Zuber TJ, DeWitt DE. Earlobe keloids. Am Fam Physician 1994;49:1835-41.
[Google Scholar]
|
| 6. |
Aköz T, Gideroglu K, Akan M. Combination of different techniques for the treatment of earlobe keloids. Aesthetic Plast Surg 2002;26:184-8.
[Google Scholar]
|
| 7. |
Butler PD, Longaker MT, Yang GP. Current progress in keloid research and treatment. J Am Coll Surg 2008;206:731-41.
[Google Scholar]
|
| 8. |
Kim DY, Kim ES, Eo SR, Kim KS, Lee SY, Cho BH. A surgical approach for earlobe keloid: Keloid fillet flap. Plast Reconstr Surg 2004;113:1668-74.
[Google Scholar]
|
| 9. |
Hatoko M, Kuwahara M, Shiba A, Tada H, Okazaki T, Muramatsu T, et al. Earlobe reconstruction using a subcutaneous island pedicle flap after resection of “earlobe keloid”. Dermatol Surg 1998;24:257-61.
[Google Scholar]
|
| 10. |
Meythiaz AM, De Mey A, Lejour M. Treatment of keloids by excision and postoperative radiotherapy. Eur J Plast Surg 1992;15:13.
[Google Scholar]
|
| 11. |
Lee Y, Minn KW, Baek RM, Hong JJ. A new surgical treatment of keloid: Keloid core excision. Ann Plast Surg 2001;46:135-40.
[Google Scholar]
|
| 12. |
Copcu E, Sivrioglu N, Oztan Y. Combination of surgery and intralesional verapamil injection in the treatment of the keloid. J Burn Care Rehabil 2004;25:1-7.
[Google Scholar]
|
| 13. |
D'Andrea F, Brongo S, Ferraro G, Baroni A. Prevention and treatment of keloids with intralesional verapamil. Dermatology 2002;204:60-2.
[Google Scholar]
|
| 14. |
Davison SP, Mess S, Kauffman LC, Al-Attar A. Ineffective treatment of keloids with interferon alpha-2b. Plast Reconstr Surg 2006;117:247-52.
[Google Scholar]
|
| 15. |
Park TH, Seo SW, Kim JK, Chang CH. Earlobe keloids: Classification according to gross morphology determines proper surgical approach. Dermatol Surg 2012;38:406-12.
[Google Scholar]
|
| 16. |
Rockwell WB, Cohen IK, Ehrlich HP. Keloids and hypertrophic scars: A comprehensive review. Plast Reconstr Surg 1989;84:827-37.
[Google Scholar]
|
| 17. |
Moustafa MF, Abdel-Fattah MA, Abdel-Fattah DC. Presumptive evidence of the effect of pregnancy estrogens on keloid growth. Case report. Plast Reconstr Surg 1975;56:450-3.
[Google Scholar]
|
| 18. |
Berman B, Bieley HC. Keloids. J Am Acad Dermatol 1995;33:117-23.
[Google Scholar]
|
| 19. |
Margaret Shanthi FX, Ernest K, Dhanraj P. Comparison of intralesional verapamil with intralesional triamcinolone in the treatment of hypertrophic scars and keloids. Indian J Dermatol Venereol Leprol 2008;74:343-8.
[Google Scholar]
|
| 20. |
Stashower ME. Successful treatment of earlobe keloids with imiquimod after tangential shave excision. Dermatol Surg 2006;32:380-6.
[Google Scholar]
|
| 21. |
Lawrence WT. Treatment of earlobe keloids with surgery plus adjuvant intralesional verapamil and pressure earrings. Ann Plast Surg 1996;37:167-9.
[Google Scholar]
|
| 22. |
Valerón-Almazán P, Dehesa-García L, Vilar-Alejo J, Domínguez-Silva J, Gómez-Duaso J, Carretero-Hernández G. Surgical treatment of relapsing keloid of the pinna by fillet flap. Actas Dermosifiliogr 2010;101:235-41.
[Google Scholar]
|
| 23. |
Al Aradi IK, Alawadhi SA, Alkhawaja FA, Alaradi I. Earlobe keloids: A pilot study of the efficacy of keloidectomy with core fillet flap and adjuvant intralesional corticosteroids. Dermatol Surg 2013;39:1514-9.
[Google Scholar]
|
Fulltext Views
5,323
PDF downloads
2,217





