Translate this page into:
Keratoacanthoma-like cutaneous metastases in a case of squamous cell carcinoma of the tongue
Correspondence Address:
Varadraj V Pai
Department of Dermatology and Venereology, Goa Medical College, Bambolim, North Goa, Goa
India
| How to cite this article: Ranglani H, Pai VV, Shukla P. Keratoacanthoma-like cutaneous metastases in a case of squamous cell carcinoma of the tongue. Indian J Dermatol Venereol Leprol 2019;85:568 |
Sir,
Cutaneous metastases from internal malignancies account for approximately 5% of all metastases.[1] Metastases to the skin from primary cancers of the upper aerodigestive tract are relatively rare.[2],[3] Of these, cutaneous metastases with a keratoacanthoma-like morphology are unusual.[2],[4]
A 50-year-old male presented with a painless nodule over the cheek of one-month duration and a single papule over the neck of 15 days duration. He had been diagnosed with squamous cell carcinoma of the base of the tongue (stage IV grade) 2 to 3 years ago, and had undergone tracheostomy and concurrent chemoradiotherapy for the same. He reported regrowth of the tumor at the base of his tongue over the past 6 months.
The cheek lesion was a hemispherical, firm, non-tender nodule, measuring 1.5 × 1.5 cm with a central crateriform depression filled with keratin [Figure - 1]. The clinical picture was suggestive of a keratoacanthoma. On the neck, changes of chronic radiation dermatitis in the form of atrophy, fibrosis and hyperpigmentation were present [Figure - 2].
 |
| Figure 1: Nodule on the cheek with central crateriform depression |
 |
| Figure 2: Changes of chronic radiation dermatitis in the form of cutaneous atrophy, fibrosis and pigmentationw |
Histopathology of the cheek lesion revealed a thinned-out epidermis with flattened rete ridges, with no evidence of cellular atypia and an intact dermoepidermal junction. The dermis showed presence of numerous atypical, large, polygonal cells displaying nuclear pleomorphism, with altered nuclear–cytoplasmic ratio, with no connection to the epidermis. In addition, a few dilated lymphatic channels showing presence of tumor emboli were present. A few horn pearls with incomplete keratinization were also evident. There was no invasion of the epidermis by the tumor cells [Figure - 3] and [Figure - 4]. Immunohistochemistry of the nodule could not be performed.
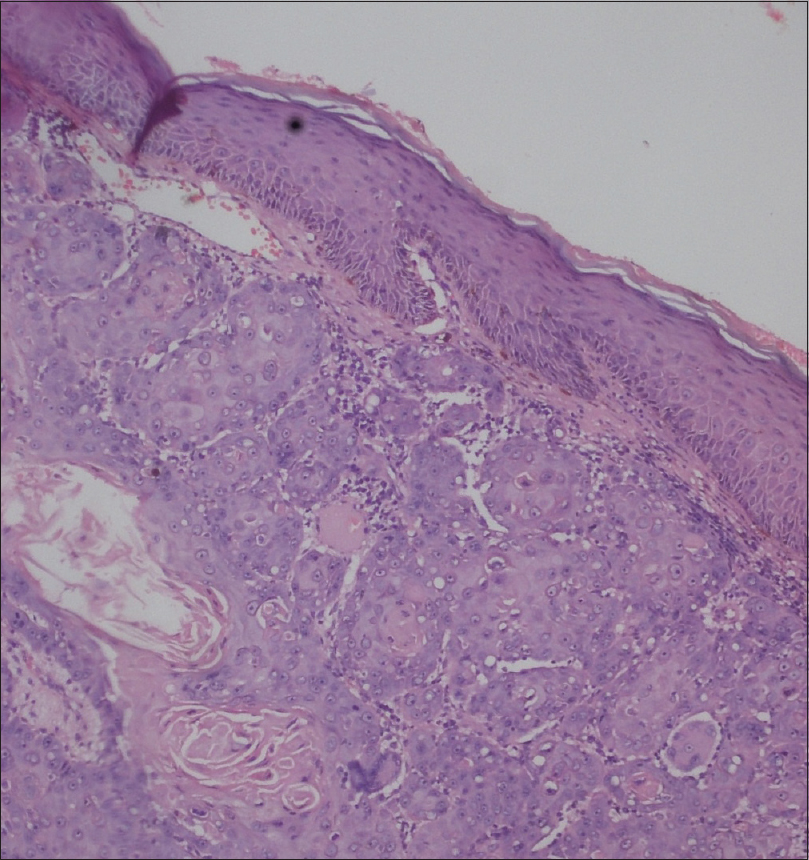 |
| Figure 3: Flattened rete ridges with an intact dermoepidermal junction. Thinned-out epidermis with dermis showing tumor cells, along with formation of horn pearls with incompletely keratinizing centres (H and E, ×10) |
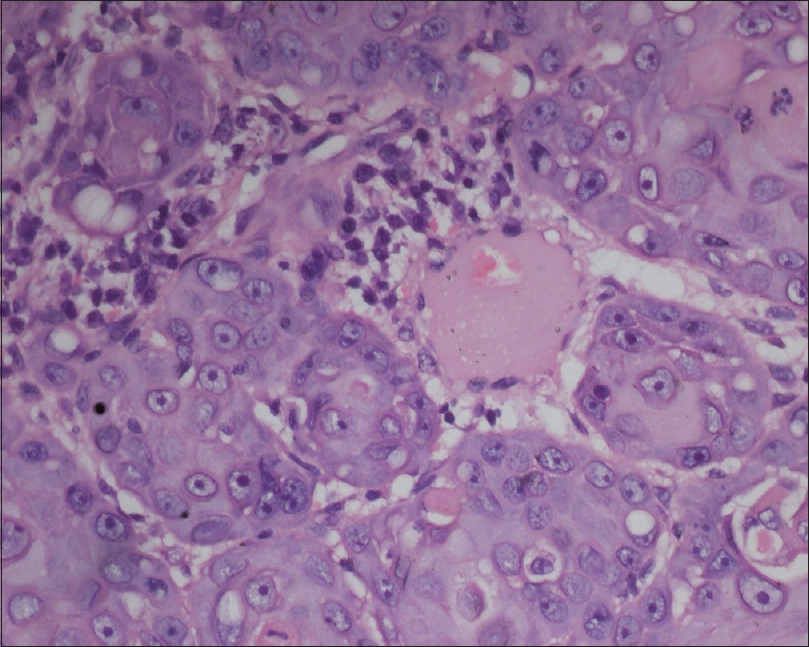 |
| Figure 4: The tumor cells exhibit cellular atypia, nuclear pleomorphism and altered nuclear–cytoplasmic ratio (H and E, ×100) |
Fine needle aspiration cytology of the enlarged cervical lymph nodes revealed deposits of tumor cells. Chest X-ray and abdominal ultrasound were normal.
Based on the clinicopathological findings of this rapidly growing nodule filled with central keratin debris in the radiation port site, along with lack of epidermal involvement, maintenance of the integrity of the dermoepidermal junction and presence of a few dilated lymphatic channels showing evidence of tumor cells, a diagnosis of keratoacanthoma-like cutaneous metastases from primary squamous cell carcinoma of the base of tongue was made upon an increase in the size of the primary tumor.
Cutaneous metastases are markers of poor prognosis.[3] The average interval between the diagnosis of primary malignancy and the appearance of cutaneous metastases is 36 months.[3] In this case, the patient presented with cutaneous metastases after 31 months of detection of the primary cancer. The interval between stoppage of treatment and appearance of cutaneous metastases was approximately 29 months. The primary tumor had been slowly increasing in size for the past two years.
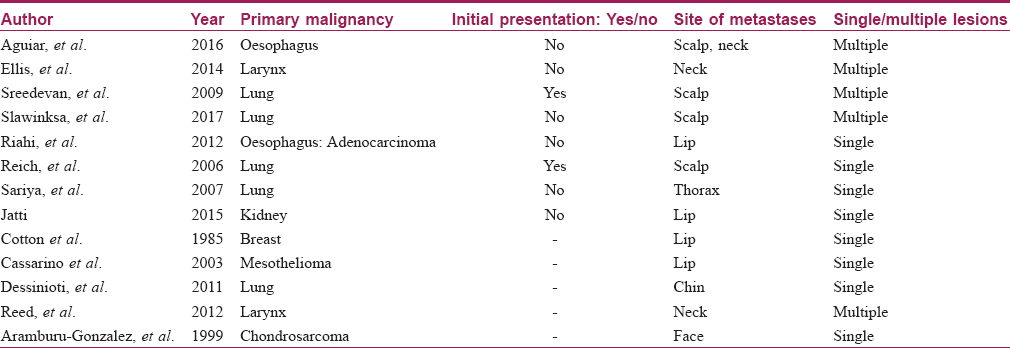
The morphology of cutaneous metastases can vary, ranging from asymptomatic papulo-nodules to erysipeloid, sclerodermoid and zosteriform lesions and even alopecia neoplastica.[3] Cutaneous metastases with keratoacanthoma-like morphology are unusual, with fewer than 20 cases reported till date [Table - 1].[2],[4],[5],[6],[7],[8],[9],[10],[11],[12],[13],[14],[15] It has also been reported to occur in the radiation port site in a patient with laryngeal carcinoma.[2] It is thought to be due to the localized alteration in the skin of the irradiated site, predisposing it to the deposition of tumor cells. The likely way of spread to the site on the right cheek was postulated to be through the lymphatics. A few malignancies associated with keratoacanthoma-like secondaries are those of the lung, bronchus, esophagus and breast.[5] Other presentations of cutaneous metastases from squamous cell carcinoma of the base of tongue include ulcerated papulonodules appearing over the face, lesions at distant sites such as thigh, forearm, abdomen and even acrometastases.
The histopathology of cutaneous metastases varies according to the nature of the primary tumor.[3] Here, the histopathology was that of moderately differentiated squamous cell carcinoma, reflecting the primary tumor.
The median survival time after the diagnosis of cutaneous metastases is approximately 6 months.[16] The treatment plan for our patient included six cycles of cyclophosphamide, doxorubicin and docetaxel. The patient was doing well for two months and was subsequently lost to follow-up.
This case is being reported for its unusual morphologic presentation of cutaneous metastases. The presence of keratoacanthoma-like lesions should alert the physician towards the possibility of cutaneous metastases.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Krathen RA, Orengo IF, Rosen T. Cutaneous metastasis: A meta-analysis of data. South Med J 2003;96:164-7.
[Google Scholar]
|
| 2. |
Ellis DL, Riahi RR, Murina AT, Cohen PR. Metastatic laryngeal carcinoma mimicking eruptive keratoacanthomas: Report of keratoacanthoma-like cutaneous metastases in a radiation port. Dermatol Online J 2014;20. pii: 13030.
[Google Scholar]
|
| 3. |
Zook MB, Wu H, Lessin SR. Cutaneous metastases. In: Jean L, Bolognia JL, Schaffer JV, editors. Dermatology. 3rd ed., Vol. 2. China: Elsevier; 2012. p. 2049-55.
[Google Scholar]
|
| 4. |
Riahi RR, Cohen PR. Clinical manifestations of cutaneous metastases: A review with special emphasis on cutaneous metastases mimicking keratoacanthoma. Am J Clin Dermatol 2012;13:103-12.
[Google Scholar]
|
| 5. |
Reich A, Kobierzycka M, Woźniak Z, Cisło M, Szepietowski JC. Keratoacanthoma-like cutaneous metastasis of lung cancer: A learning point. Acta Derm Venereol 2006;86:459-60.
[Google Scholar]
|
| 6. |
Schoenlaub P, Sarraux A, Grosshans E, Heid E, Cribier B. Survival after cutaneous metastasis: A study of 200 cases. Ann Dermatol Venereol 2001;128:1310-5.
[Google Scholar]
|
| 7. |
Aguiara HR, Calderonia DR, Stelinib RF, Andreolloc NA, Kharmandayana P. Multiple cutaneous metastases of oesophageal squamous cell carcinoma that mimic keratoacanthoma. JPRAS Open 2016;7:27-31.
[Google Scholar]
|
| 8. |
Sreedevan V, Nair SP, Kumar GN, Skaria L, Mathew R, Sanker A, et al. Keratoacanthoma like secondaries on the scalp. Indian J Dermatol Venereol Leprol 2009;75:523-4.
[Google Scholar]
|
| 9. |
Sławińska M, Sobjanek M, Biernat W, Nowicki R. Keratoacanthomalike cutaneous metastases as the first presentation of lung cancer. Pol Arch Intern Med 2017;127:66-7.
[Google Scholar]
|
| 10. |
Sariya D, Ruth K, Adams-McDonnell R, Cusack C, Xu X, Elenitsas R, et al. Clinicopathologic correlation of cutaneous metastases: Experience from a cancer center. JAMA Dermatol 2007;143:613-20.
[Google Scholar]
|
| 11. |
Jatti D, Puri G, Aravinda K, Dheer DS. An atypical metastasis of renal clear cell carcinoma to the upper lip: A case report. J Oral Maxillofac Surg 2015;73:371.e1-6.
[Google Scholar]
|
| 12. |
Cotton DW, Fairris GM. Metastatic breast carcinoma on the lip: Case report. Dermatologica 1985;171:362-5.
[Google Scholar]
|
| 13. |
Cassarino DS, Xue W, Shannon KJ. Widespread cutaneous and perioral metastases of mesothelioma. J Cutan Pathol 2003;30:582-5.
[Google Scholar]
|
| 14. |
Dessinioti C, Georgala S, Chatziolou E, Georgala K. What is your diagnosis? Cutaneous metastases from non-small cell lung carcinoma. Cutis 2011;87:277, 281-3.
[Google Scholar]
|
| 15. |
Reed KB, Cook-Norris RH, Brewer JD. The cutaneous manifestations of metastatic malignant melanoma. Int J Dermatol 2012;51:243-9.
[Google Scholar]
|
| 16. |
Aramburu-González JA, Rodríguez-Justo M, Jiménez-Reyes J, Santonja C. A case of soft tissue mesenchymal chondrosarcoma metastatic to skin, clinically mimicking keratoacanthoma. Am J Dermatopathol 1999;21:392-4.
[Google Scholar]
|
Fulltext Views
3,273
PDF downloads
2,092





