Translate this page into:
Kikuchi's disease associated with systemic lupus erythematosus
2 Departments of Medicine, S. N. Medical College and HSK Hospital and Research Centre, Bagalkot, Karnataka, India
3 Departments of Pathology, S. N. Medical College and HSK Hospital and Research Centre, Bagalkot, Karnataka, India
Correspondence Address:
S Chidambara Murthy
Department of Dermatology and Venereology, S. N. Medical College and HSK Hospital and Research Centre, Bagalkot-587 102, Karnataka
India
| How to cite this article: Murthy S C, Dandin SM, Dandin AS, Patwardan MY. Kikuchi's disease associated with systemic lupus erythematosus. Indian J Dermatol Venereol Leprol 2005;71:338-341 |
Abstract
A 25-year-old multiparous female presented with fever, joint pains, facial rash and lymphadenopathy of three months' duration. Lymph node biopsy revealed a diagnosis of Kikuchi's disease. She fulfilled seven out of the 11 ARA criteria for SLE. The association of Kikuchi's disease and SLE is rare.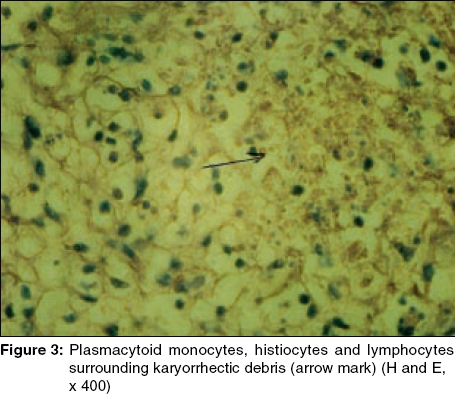 |
 |
 |
 |
 |
 |
Introduction
Kikuchi′s disease (KD), also known as Kikuchi-Fujimoto disease and histiocytic necrotizing lymphadenitis, is a rare, self-limiting condition, characteristically involving the lymph nodes. It is a distinct clinicopathological entity of unknown etiology. About 16.6% to 40% of patients with KD are reported to have cutaneous involvement.[1] Skin lesions can be non-specific and can present as facial erythema, erythematous papules, plaques, nodules and ulcers.[2] KD is rarely associated with systemic lupus erythematosus (SLE), Still′s disease and Sweet′s syndrome.[3] Rarer associations include subacute cutaneous lupus erythematosus,[4] discoid lupus erythematosus, Well′s syndrome[5] and primary Sj φgren′s syndrome.[6] The diagnosis of KD can precede, postdate or coincide with the diagnosis of SLE.[7]
CASE REPORT
A 25-year-old multiparous female presented to us with fever; pain and swelling of the small joints of the hands, feet and wrists; photosensitivity; facial rash; and lymphadenopathy of three months′ duration. She had been admitted to a hospital and had undergone fine needle aspiration cytology (FNAC) of a lymph node and was diagnosed as tuberculous lymphadenitis with discoid lupus erythematosus. She was treated with antituberculous drugs and topical corticosteroids, with no improvement. She had undergone two blood transfusions for anemia during her hospital stay. There was no drug intake, atopy or other systemic complaints.
Cutaneous examination revealed a bilaterally symmetrical erythematous, edematous rash over the malar eminences and the bridge of the nose. A few pustules, ulceration and crusting were present over the nose and lower lip [Figure - 1]. A discoid rash involving the face, scalp, and ears, and diffuse alopecia of the scalp were present. The mucosae were normal. The nails were normal, with no dilated nailfold capillaries. Firm, discrete, non-tender lymphadenopathy involving bilateral deep cervical and left axillary groups was present. Swelling and tenderness of small joints of the hands, feet, and wrists were present bilaterally. Systemic examination did not reveal unusual findings.
Her hematological investigations showed anemia (Hb, 8.6 g%), leucopenia (total leucocyte count, 3,900/cmm) and mild thrombocytopenia (platelet count, 1,36,200/cmm); the ESR was 115 mm/h and direct Coombs test was negative. Urine analysis showed traces of proteins and the 24-hour urine protein was 268 mg. The blood glucose, liver function tests, blood urea, serum creatinine, and ECG were normal. A chest X-ray, X-ray of the involved joints, and ultrasonography of the abdomen were normal. Blood VDRL, HIV (ELISA), Mantoux test, rheumatoid factor and LE cell phenomenon were negative. Antinuclear antibodies (ANA) and anti-DNA antibody were positive.
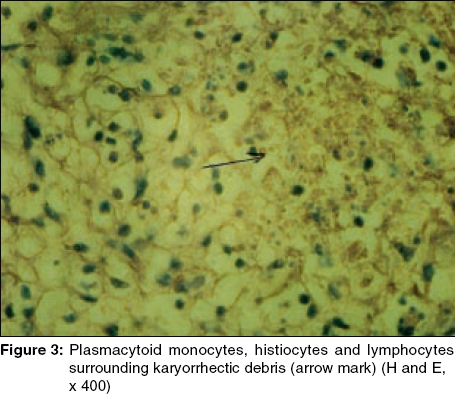
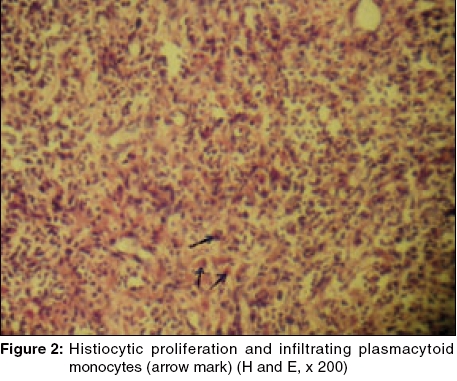
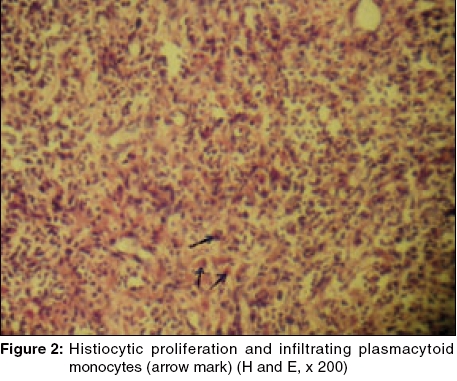
Skin biopsy from a discoid lesion showed features consistent with discoid lupus erythematosus. FNAC of the axillary lymph node was suggestive of Kikuchi′s disease. Biopsy of the lymph node showed well-defined focal paracortical necrosis, with zonal histiocytic proliferation, infiltrating plasmacytoid monocytes [Figure - 2], and lymphocytes surrounding karyorrhectic debris [Figure - 3]. Neutrophils and hematoxyphilic bodies were conspicuously absent. Staining for AFB was negative. Serology for Epstein-Barr virus, cytomegalovirus, parvovirus B19, toxoplasma, HHV-6, and HTLV-1 could not be done for the want of facilities. Based on these findings, a diagnosis of Kikuchi′s disease associated with SLE was made.
DISCUSSION
Histiocytic necrotizing lymphadenitis was first described in Japan by Kikuchi and then independently by Fujimoto et al in 1972. Pileri et al, in 1982, reported this condition for the first time outside Japan. Since then, it has been reported worldwide.[2]
The cause of this rare, self-limiting disease remains unknown. It may be due to a hyperimmune reaction to an infectious agent. Several infectious agents, including Epstein-Barr virus, HHV-6, HIV, Parvovirus B19, Yersinia, and Toxoplasma have been suggested.[2] Apoptosis is thought to play an important role in the pathogenesis. Cytotoxic T lymphocytes are considered to be apoptotic effectors as well as target cells, while histiocytes could possibly enhance apoptosis in KD.[1] The role of autoimmunity has also been suggested in the pathogenesis. [1],[2],[3],[4],[5],[6],[7],[8],
KD predominantly affects females (male:female ratio 1:4), with a mean age of 30 years. The disease commonly presents with cervical lymphadenopathy, which may be painless and isolated, or accompanied by diffuse lymphadenopathy, fever, chills, myalgia and non-specific skin lesions. Systemic symptoms are severe when extra-nodal involvement is present. Although recurrences are possible, it clears spontaneously in 1-4 months. Histologically, lymphohistiocytic aggregates with patchy necrosis and karyorrhexis are seen. The lymphohistiocytic aggregates contain atypical lymphoid cells, histiocytes, transformed lymphoid cells and "plasmacytoid" T cells.[2]
The association of KD and SLE is well documented.[3],[4],[5],[6],[7],[8],[9],[10], It is also speculated that KD may be one of the manifestations of SLE.[9] Some investigators have suggested that KD may represent a forme fruste of SLE.[11]
Clinically, tuberculous lymphadenitis remains a major differential diagnosis, especially in developing countries like India. Patients may be empirically started on anti-tuberculous therapy (ATT), with no significant response. Biopsy of the lymph node reveals the actual diagnosis.[12] Our case was started on ATT, after FNAC, with no improvement.
SLE can also present with lymphadenopathy, although there are a few differences between them. The involvement of lymph nodes in KD is focal, while more extensive involvement is observed in lupus lymphadenitis. Histologically, the presence of hematoxyphilic bodies, abundant plasma cells and true vasculitis outside the areas of necrosis also favors a diagnosis of SLE.[11] The absence or paucity of neutrophils confirms the diagnosis of KD.[7] Histologically, KD has to be differentiated from malignant lymphoma, SLE, Yersinia infection, cat scratch disease, toxoplasmosis, infectious mononucleosis, lymph node infarction, Kawasaki disease and AIDS.[2]
Our case fulfilled seven out of the eleven ARA criteria, compatible with the diagnosis of SLE. Histopathology of a lymph node showed typical features of KD.
Although KD is a self-limiting disease, corticosteroids are suggested as an appropriate treatment,[7] as they may aid in speedy resolution.[3] Further, corticosteroids are effective for both the disorders. Recent therapeutic options for KD include minocycline,[13] ciprofloxacin,[14] chloroquine and hydroxychloroquine.[15] Response to antimicrobials suggests a possible microbial etiology.[14],[15] Chloroquine and hydroxychloroquine probably act by their anti-inflammatory property.[15]
Patients with KD should be assessed for SLE and followed up for development of SLE. KD should be ruled out in a flare-up of SLE accompanied by lymphadenopathy.[7] This report emphasizes the association of KD and SLE.
| 1. |
Yasukawa K, Matsumura T, Sato-Matsumura KC, Takahashi T, Fujioka Y, Kobayashi H, et al . Kikuchi's disease and the skin: case report and review of the literature. Br J Dermatol 2001;144:885-9.
[Google Scholar]
|
| 2. |
Yen A, Fearneyhough P, Raimer SS, Hudnall SD. EBV- associated Kikuchi's histiocytic necrotizing lymphadenitis with cutaneous manifestations. J Am Acad Dermatol 1997;36:342-6.
[Google Scholar]
|
| 3. |
Rowell NR, Goodfield MJ. The 'Connective tissue diseases'. In : Champion RH, Burton JL, Burns DA, Breathnach SM, editors. Textbook of dermatology. 6th edn. Oxford: Blackwell Science; 1998. p. 2438-99.
In : Champion RH, Burton JL, Burns DA, Breathnach SM, editors. Textbook of dermatology. 6th edn. Oxford: Blackwell Science; 1998. p. 2438-99.'>[Google Scholar]
|
| 4. |
Toll A, Gilaberte M, Matias-Guiu X, Camacho L, Alomar A, Gonzalez-Gay MA, et al. Kikuchi's disease (necrotizing lymphadenitis) with cutaneous involvement associated with subacute cutaneous lupus erythematosus. Clin Exp Dermatol 2004;29:240-3.
[Google Scholar]
|
| 5. |
Viseux V, Schoenlaub P, Marciniak S, Staroz F, Plantin P. Kikuchi's disease associated with cutaneous manifestations evoking Well's syndrome. Ann Dermatol Venereol 2003;130:1150-3.
[Google Scholar]
|
| 6. |
Miyashita Y, Yamaguchi M, Fujimoto W. Painful indurated erythema suggestive of Kikuchi-Fujimoto disease in a patient with primary Sj φgren's syndrome. J Dermatol 2003;30:608-11.
[Google Scholar]
|
| 7. |
Martinez-Vazquez C, Hughes G, Bordon J, Alonso-Alonso J, Anibarro-Garcia A, Redondo-Martinez E, et al . Histiocytic necrotizing lymphadenitis, Kikuchi-Fujimoto's disease, associated with systemic lupus erythematosus Q J Med 1997:90:531-3.
[Google Scholar]
|
| 8. |
Meyer O, Ribard P, Belmatoug N, Kahn MF, Grossin M, Fournet JC, et al . Three cases of Kikuchi's lymphadenitis in systemic lupus erythematosus: role of the parvovirus B19. Ann Med Interne (Paris) 1991;142:259-64.
[Google Scholar]
|
| 9. |
El-Ramahi KM, Karrar A, Ali MA. Kikuchi's disease and its association with systemic lupus erythematosus. Lupus 1994;3:409-11.
[Google Scholar]
|
| 10. |
Komocsi A, Tovari E, Pajor L, Czirjak L. Histiocytic necrotizing lymphadenitis preceding systemic lupus erythematosus. J Eur Acad Dermatol Venereol 2001;15:476-80.
[Google Scholar]
|
| 11. |
Spies J, Foucar K, Thompson CT, Le Boit PE. The histopathology of cutaneous lesions of Kikuchi's disease (necrotizing lymphadenitis). A report of five cases. Am J Surg Pathol 1999;23:1040-7.
[Google Scholar]
|
| 12. |
Basu D, Mutha SM. Histiocytic necrotizing lymphadenitis (Kikuchi-Fujimoto disease) - A report of four cases. Indian J Pathol Microbiol 2002;45:89-92.
[Google Scholar]
|
| 13. |
Takada K, Suzuki K, Hidaka T, Konishi T, Shinohara T, Kataharada K, et al . Immediate remission obtained by minocycline in a patient with histiocytic necrotizing lymphadenitis. Intern Med 2001;40:1055-8.
[Google Scholar]
|
| 14. |
Mahajan VK, Sharma NL. Kikuchi-Fujimoto disease: immediate remission with ciprofloxacin. Int J Dermatol 2004;43:370-2.
[Google Scholar]
|
| 15. |
Rezai K, Kuchipudi S, Chundi V, Ariga R, Loew J, Sha BE. Kikuchi-Fujimoto disease: hydroxychloroquine as a treatment. Clin Infect Dis 2004;39:124-6.
[Google Scholar]
|
Fulltext Views
3,415
PDF downloads
3,112





