Translate this page into:
Lack of an etiologic role of human papillomavirus in the development of skin tags in the Korean population: A cross-sectional comparative study
2 Department of Dermatology, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
Correspondence Address:
Hyun Jeong Park
Department of Dermatology, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, 10, 63-Ro, Yeongdeungpo-Gu, Seoul, 07345
Korea
| How to cite this article: Woo YR, Jung Y, Park HJ. Lack of an etiologic role of human papillomavirus in the development of skin tags in the Korean population: A cross-sectional comparative study. Indian J Dermatol Venereol Leprol 2020;86:588-591 |
Sir,
The skin tag is a commonly encountered benign cutaneous tumor located frequently in the intertriginous area. Although the etiology of skin tag has been poorly understood, diabetes mellitus, obesity and atherosclerosis have been reported to be related to the pathogenesis of the skin tag.[1] Also, infection with human papillomaviruses has been implicated in the pathogenesis of skin tag.[2] To date, some studies have described the importance of human papillomavirus in the etiopathogenesis of skin tag,[2],[3] however, another study has been unable to confirm this association.[4] Therefore, this study is aimed to clarify the biological relevance of specific types of human papillomavirus in the pathogenesis of skin tags by using multiplex real-time polymerase chain reaction assay.
Skin samples of clinically suspicious skin tags were biopsied for pathological confirmation [Figure - 1] and recruited from the Department of Dermatology at Yeouido St. Mary's Hospital. This study was approved by the Ethics Committee of the Yeouido St. Hospital. Among them, skin tags from 34 patients were clinically and pathologically diagnosed as skin tags, by two board-certified dermatologists [Figure - 1]. Finally, lesional skin tissues of skin tags from 34 patients were retrieved. Additionally, skin biopsies were conducted from 26 healthy subjects as negative controls and five patients with condyloma as positive controls. DNA was purified from skin biopsy specimens using the DNA isolation kit (Maxwell TM, Promega Corporation, Madison, USA) according to the manufacturer's instructions. Purified DNA was analyzed for the presence of 20 high-risk human papillomavirus types (16, 18, 26, 31, 33, 35, 39, 45, 51, 52, 53, 56, 58, 59, 66, 68, 69, 70, 73 and 82) and 20 low-risk human papillomavirus types (6, 11, 30, 32, 34, 40, 42, 43, 44, 54, 55, 61, 62, 67, 74, 81, 83, 84, 87 and 90) by using the multiplex real-time polymerase chain reaction amplification and melting curve analysis (human papillomavirus PANA RealTyperTM, Panagene, Daejeon, South Korea) as previously described.[5] The demographic characteristics of the patients with skin tags are summarized in [Table - 1]. The mean age of patients with skin tags was 50.62 years (standard deviation: 2.27). Moreover, 24 (28%) patients with skin tags had been diagnosed with hypertension, followed by dyslipidemia (n = 10, 20%) and diabetes mellitus (n = 9, 18%). Furthermore, 22 (64.7%) patients with skin tags were overweight. On multiplex real-time polymerase chain reaction analysis, the presence of 20 high-risk human papillomavirus types or 20 low-risk human papillomavirus types was not observed in all specimens from patients with skin tags [Figure - 2]. Human papillomavirus 6 (n = 2), 11 (n = 2) and 54 (n = 1) types were detected in positive controls. Polymerase chain reactions for negative controls showed negative results among the tested human papillomavirus types.
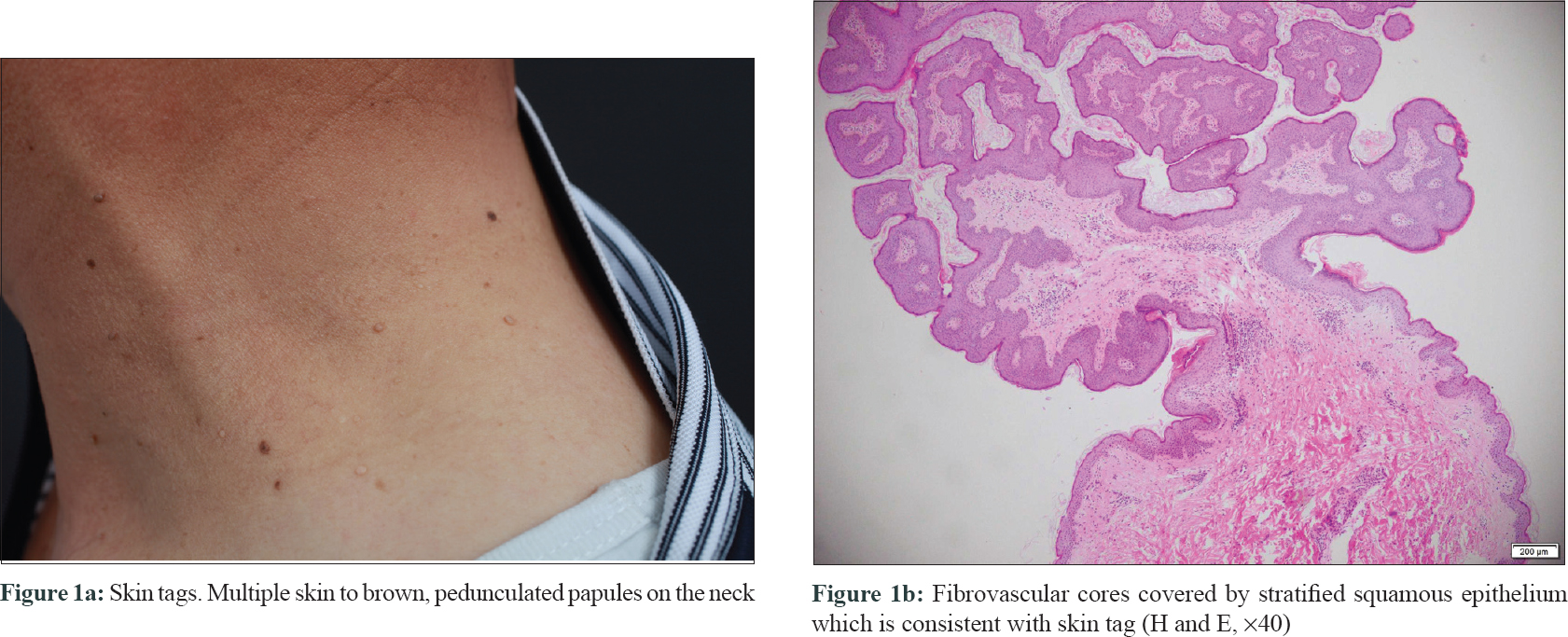 |
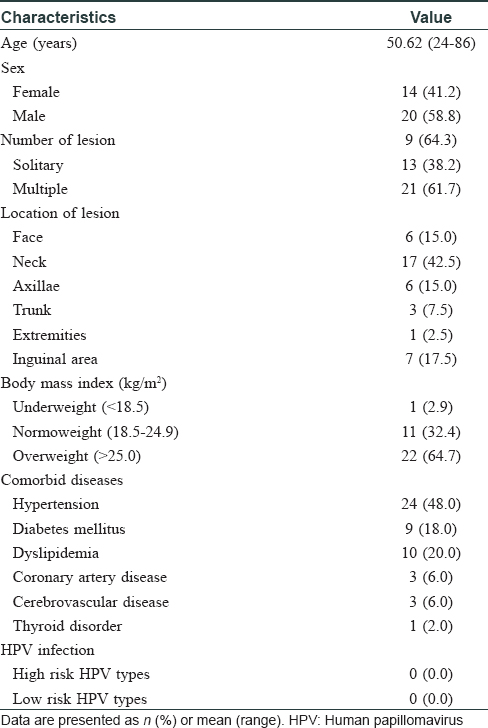
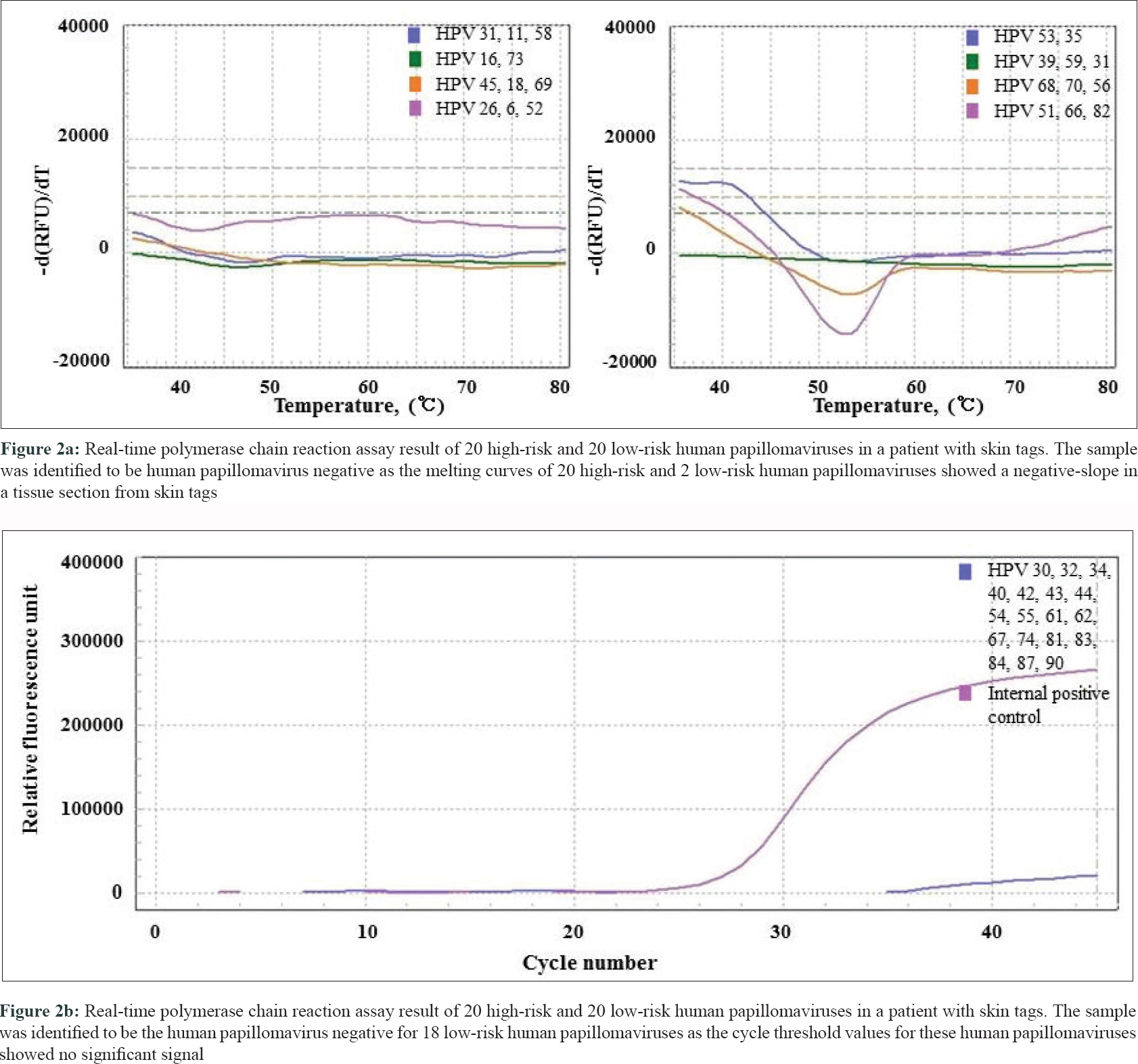 |
In this study, we found a lack of an association between skin tags and 20 high-risk and 20 low-risk human papillomavirus infections in the Korean population. However, Dianzani et al.[2] found an 88% positivity of human papillomavirus DNA type 6/11 in skin tags from Caucasian patients, and Gupta et al.[3] found 48.6% of skin tags presented with human papillomavirus DNA 6/11, which were in contrast to the findings of this study. The methodological differences in human papillomavirus detection or ethnic disparities in the study population might explain this difference. However, we suspect that this discrepancy might be due to the possibility of inclusion of a cutaneous wart as a study specimen in previous studies, instead of a skin tag, due to the clinical similarity between a skin tag and a viral wart. In this study, we only included pathologically confirmed skin tags and used the real-time polymerase chain reaction method for the analysis which could provide a more reliable result in our study compared with previous studies. In conclusion, skin tags have varied etiology and human papillomavirus could be one of them, which may be an independent causative factor or one producing comorbidity. The frequency of human papillomavirus infection varies in diverse studies. Although the specific types of human papillomavirus might be associated with the causation of skin tags, our pilot study showed the lack of association between 20 high-risk and 20 low-risk human papillomavirus types and skin tags. The limitation of this study is the small sample size. Therefore, further studies with a larger number of patients and wider human papillomavirus screening are needed to clarify this observation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal the identity, but anonymity cannot be guaranteed.
Acknowledgment
This work was supported by the Basic Science Research program and Creative Materials Discovery Program through the National Research Foundation of Korea (NRF), which is funded by the Ministry of Education, Science and Technology and the Ministry of Science, ICT and Future Planning (2018R1A1A3A04078241).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Mettman D, Fraga GR. Adipocytes in fibroepithelial polyps are not related to diabetes mellitus or obesity. J Am Acad Dermatol 2018;79:1154-5.
[Google Scholar]
|
| 2. |
Dianzani C, Calvieri S, Pierangeli A, Imperi M, Bucci M, Degener AM. The detection of human papillomavirus DNA in skin tags. Br J Dermatol 1998;138:649-51.
[Google Scholar]
|
| 3. |
Gupta S, Aggarwal R, Gupta S, Arora SK. Human papillomavirus and skin tags: Is there any association? Indian J Dermatol Venereol Leprol 2008;74:222-5.
[Google Scholar]
|
| 4. |
Pezeshkpoor F, Jafarian AH, Ghazvini K, Yazdanpanah MJ, Sadeghian A, Esmaili H, et al. An association of human papillomaviruses low risk and high risk subtypes with skin tag. Iran J Basic Med Sci 2012;15:840-4.
[Google Scholar]
|
| 5. |
Kim YH, Chung HS, Lee MJ. Comparison of PANA RealTyper HPV kit with AdvanSure HPV GenoBlot assay for human papillomavirus genotyping. Ann Clin Microbiol 2018;21:86-91.
[Google Scholar]
|
Fulltext Views
3,358
PDF downloads
1,924





