Translate this page into:
Langerhans cell histiocytosis: An uncommon presentation, successfully treated by thalidomide
Correspondence Address:
Safoura Shakoei
Skin Research Center, Shahid Beheshti University, Shohada-e Tajrish Hospital, Shahrdari St., 1989934148, Tehran
Iran
| How to cite this article: Shahidi-Dadras M, Saeedi M, Shakoei S, Ayatollahi A. Langerhans cell histiocytosis: An uncommon presentation, successfully treated by thalidomide. Indian J Dermatol Venereol Leprol 2011;77:587-590 |
Abstract
Langerhans cell histiocytosis (LCH) is a rare disease and generally affects children under 15 years of age. Adult onset form and cutaneous features at presentation are uncommon. There are some options for treatment of the skin lesions of LCH such as topical and intralesional corticosteroid, nitrogen mustard, etc., which are not completely curative. Herein, we report a case of perianal LCH in a 20-year-old man with one-year history of recalcitrant well-demarcated, erythematous, and ulcerated plaque surrounding the anal orifice, with pain and difficulty in defecation that was successfully treated with thalidomide.Introduction
Langerhans cell histiocytosis (LCH), the most common type of histiocytosis, is a rare disease and generally affects children. [1] Various clinical syndromes have been described for LCH. Four major types are acute disseminated LCH (Letterer-Siwe disease), classic multifocal LCH (Hand-Schuller-Christian disease), chronic unifocal LCH (eosinophilic granuloma), and congenital self-healing reticulohistiocytosis. The cutaneous lesions may be the sole manifestation of LCH where typical manifestation is a seborrheic dermatitis-like lesion on the scalp and the flexural regions. [2],[3] There are some options to treat the skin lesions of LCH such as thalidomide.
Case Report
A 20-year-old man was referred to our dermatology clinic with one-year history of perianal lesion, with pain and difficulty in defecation. Physical examination revealed well-demarcated, erythematous, and ulcerated plaque surrounding the anal orifice [Figure - 1]. It was infiltrated on palpation and severely tender. Medical history was unremarkable. Despite several therapies, such as different types of systemic and topical antibiotics and topical steroids, he had not experienced any significant improvements. The routine laboratory assessments such as blood count, kidney and liver function tests, serum electrolytes, erythrocyte sedimentation rate, collagen vascular disease tests, and tuberculin test were all within normal limits. The patient had undergone a colonoscopy for detection of probable extension of the lesion to gastrointestinal (GI) tract and also to rule out the Crohn′s disease, but no abnormal finding was reported. A biopsy was taken with a clinical differential diagnoses of extramammary Paget′s disease, Bowen′s disease, chronic eczema, tuberculosis, and Crohn′s disease.
 |
| Figure 1: Well demarcated, erythematous and ulcerated plaque, surrounded the anal orifice |
Histological examination showed a rich dermal infiltration with large histiocytes with reniform nucleus. There were few eosinophils, neutrophils, lymphocytes, plasma cells, and mast cells among the histiocytic infiltration. All of these findings were compatible with the diagnosis of LCH [Figure - 2].
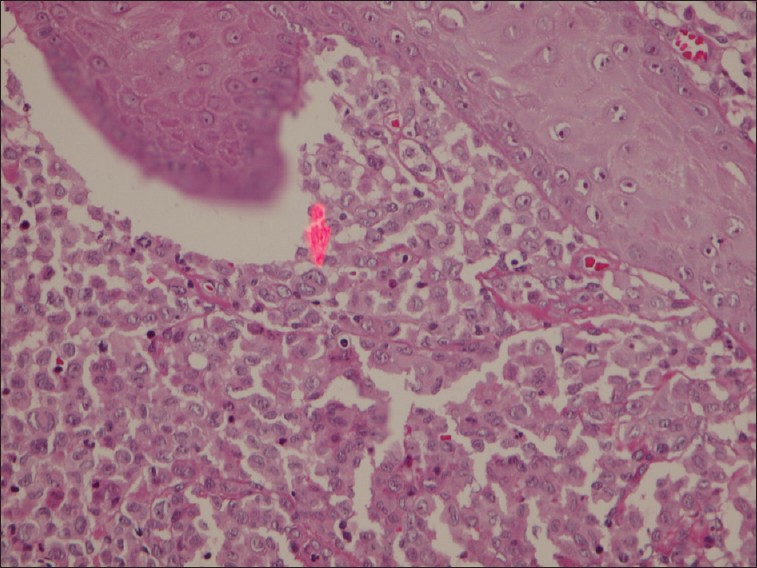 |
| Figure 2: Rich dermal infiltration with large histiocytes with reniform nucleus (H and E, ×400) |
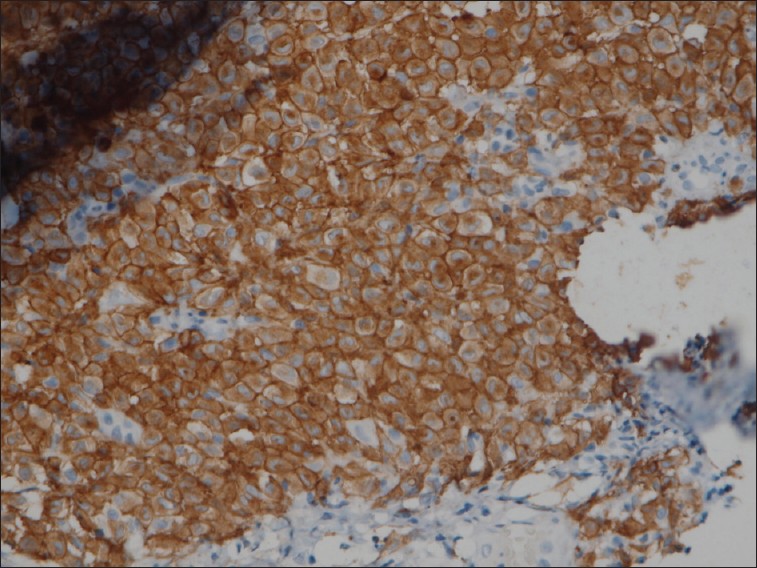
On immunohistochemical study, tumoral cells were positive for S100 [Figure - 3] and CD1a [Figure - 4] and negative for CD68 [Figure - 5], thus the diagnosis of LCH was established.
 |
| Figure 3: Immunohistochemical study, S100 positivity (×400) |
 |
| Figure 4: Immunohistochemical study, CD1a positivity (×400) |
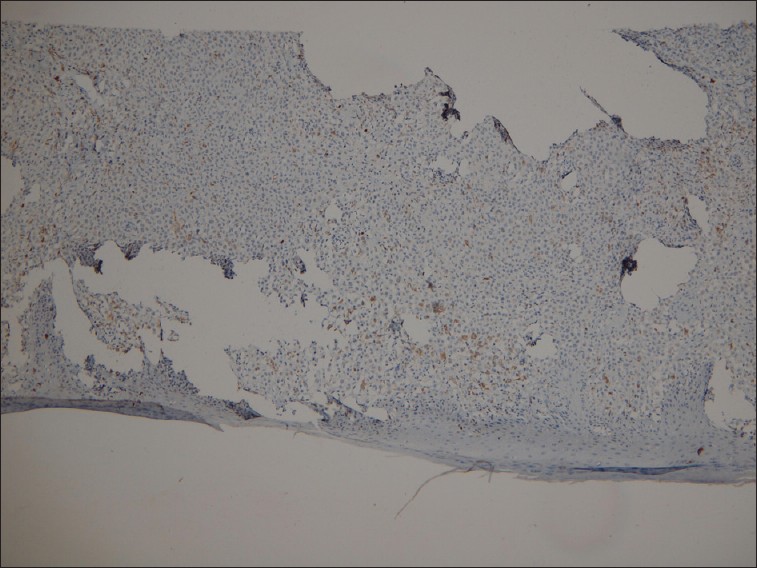 |
| Figure 5: Immunohistochemical study, negative for CD68 (×400) |
After confirmation of the diagnosis, a systemic evaluation for detection of any other site of involvement was done. Hematologic and serologic assessments including differential blood count and peripheral blood smear were all in normal range. Also, imaging studies including bone X-ray and CT scan of brain, chest, abdomen, and pelvis were performed to look for any bone, lymph node, pituitary, or visceral involvement. There was no site of involvement except the perianal lesion. Thalidomide was initiated at a dose of 100 mg nightly, gradually increased to 200 mg at night. One and half months after starting thalidomide, partial improvement was noted. He was on 200 mg daily thalidomide for 4 months followed by 2 months treatment with 100 mg daily. After 6 months, the lesion dramatically shrunk and became painless [Figure - 6] and thalidomide was tapered to a maintenance dose of 50 mg/d. No adverse effects of thalidomide were seen during the course of the treatment.
 |
| Figure 6: Six months after thalidomide therapy |
Discussion
LCH, the most common type of the histiocytosis, is a rare disease and generally affects children. [1] Three to four cases per million occur annually in children under 15 years of age, [2] with a male : female ratio of 2 : 1. [1] Its peak incidence is in infants aged 1 to 2 years, but can affect all age groups.
The cutaneous lesions may be the only manifestation of LCH. [2],[3] The typical skin manifestation is a seborrheic dermatitis-like lesion on the scalp and the flexures. Adult onset type and the presence of cutaneous features at presentation are uncommon. [3]
Chest x-ray and standard laboratory tests such as full blood count, liver function tests, and coagulation studies are usually requested in the case of LCH. Urine osmolality test is mandatory for assessing the presence of diabetes insipidus. More specific tests are required depending on the site of the suspected lesion. [1] Perianal involvement as the sole manifestation of LCH has been described earlier in few case reports. [3],[4],[5],[6] We also found two reports of perianal lesion with the involvement of other organs. [7],[8] Our case was a 20-year-old man with solitary perianal lesion without systemic involvement that was treated with thalidomide.
The treatment for LCH is varied and depends on the extent of the disease and the degree of the organ involvement.
Observation, curettage, excision, intralesional corticosteroids, nitrogen mustard, external beam radiotherapy, systemic chemotherapy, immunomodulation, and stem cell transplantation have been used for management of mucocutaneous LCH with varying outcomes. [6],[9] Glucocorticoids have been used either topically for skin lesions or systemically for more invasive disease and when there is multisystem involvement chemotherapeutic agents are indicated. [1]
Topical corticosteroid was used in our case with no significant improvement. Nitrogen mustard was not available. X-rays may induce perianal cicatricial contracture, and surgery or systemic corticosteroids would have produced more side effects than thalidomide. Stem cell transplantation was not considered for him. Therefore, we chose oral thalidomide for treating the lesion. Thalidomide is an anti-inflammatory, anti angiogenic, and immunomodulatory compound that decreases the level of cytokines and TNF-α. The proliferation and production of Langerhans cells from hematopoietic stem cells is promoted by TNF-α. [6] Therefore, thalidomide can theoretically treat LCH by inhibiting the production of TNF-α.
Thalidomide has been used successfully for treatment of localized LCH such as perianal lesions, [6] genital and disseminated skin lesions. [10] Earlier case studies have reported dramatic responses to thalidomide of both cutaneous and anogenital lesions. [6],[10]
Our case was treated with thalidomide and after six months, the lesion had significantly resolved.
It should be kept in mind that LCH could be one of the differential diagnoses of the perianal lesions.
| 1. |
Foster A, Epanoimeritakis M, Moorehead J. Langerhans cell histiocytosis of the perianal region. Ulster Med J 2003;72:50-1.
[Google Scholar]
|
| 2. |
Broekaert SM, Metzler G, Burgdorf W, Rocken M, Schaller M. Multisystem Langerhans cell histiocytosis: Successful treatment with thalidomide. Am J Clin Dermatol 2007;8:311-4.
[Google Scholar]
|
| 3. |
Field M, Inston N, Muzaffar S, Cruickshank N. Perianal Langerhans cell histiocytosis. Int J Colorectal Dis 2007;22:1141-2.
[Google Scholar]
|
| 4. |
Landolsi A, Ben Fatma L, Yacoubi MT, Kallel L, Gharbi O, Aloulou S , et al. Perianal ulceration revealing Langerhans cell histiocytosis. Tunis Med 2003;81:967-8.
[Google Scholar]
|
| 5. |
Mango JC, D'Almeida DG, Magalhães JP, Pires VJ, Araújo ML, Miranda CB, et al. Perianal Langerhans cell histiocytosis: Case report and literature review. Rev bras. Colo-proctol 2007;27:83-8.
et al. Perianal Langerhans cell histiocytosis: Case report and literature review. Rev bras. Colo-proctol 2007;27:83-8.'>[Google Scholar]
|
| 6. |
Li R, Lin T, Gu H, Zhou Z. Successful thalidomide treatment of adult solitary perianal Langerhans cell histiocytosis. Eur J Dermatol 2010;20:391-2.
[Google Scholar]
|
| 7. |
Tinsa F, Brini I, Kharfi M, Mrad K, Boussetta K, Bousnina S. Perianal presentation of Langerhans cell histiocytosis in children. Gastroentérol Clin Biol 2010;34:95-7.
[Google Scholar]
|
| 8. |
Oguzkurt P, Sarialioglu F, Ezer SS, Ince E, Kayaselcuk F, Hicsonmez A. An uncommon presenting sign of Langerhans cell histiocytosis: Focal perianal lesions without systemic involvement. J Pediatr Hematol Oncol 2008;30:915-6.
[Google Scholar]
|
| 9. |
Mittal T, Davis MD, Lundell RB. Perianal Langerhans cell histiocytosis relieved by surgical excision. Br J Dermatol 2009;160:213-5.
[Google Scholar]
|
| 10. |
Sander CS, Kaatz M, Elsner P. Successful treatment of cutaneous Langerhans cell histiocytosis with thalidomide. Dermatology 2004;208:149-52.
[Google Scholar]
|
Fulltext Views
4,716
PDF downloads
2,530





