Translate this page into:
Langerhans cell histiocytosis of vulva and perineum
Corresponding author: Dr. Chandra Sekhar Sirka, Department of Dermatology and Venereology, AIIMS, Sijua, Patrapada, Bhubaneswar - 751 019, Odisha, India. csirka2006@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sirka CS, Sethy M, Rout AN, Sahu K. Langerhans cell histiocytosis of vulva and perineum: A rare case report. Indian J Dermatol Venereol Leprol 2021;87:75-7.
Sir,
Langerhans cell histiocytosis (LCH) is a rare disorder characterized by clonal proliferation of bone-marrow-derived Langerhans cells in various systems. Lesions on the genital tract are uncommon, with only a few reports of isolated vulvar LCH.1 Rarely, LCH has been reported in postmenopausal women with nonspecific vulvar lesions.2 We report a case of isolated vulvar and perineal LCH in a postmenopausal woman successfully treated with oral prednisolone and methotrexate. A- 54-year-old female presented with painless nonhealing ulcer over the vulva of 2 years duration. There was history of intermittent bleeding from the ulcer. She had received many antibiotics for variable period without any improvement. There was no history of any loss of weight or appetite. Bowel habits were normal. She was married with three children and gave no history of extra-marital contact. On examination, there was a well-defined ulcer of size 7 cm × 4.5 cm, with friable pale granulation tissue in the floor, undermined edges and irregular margin. The- labia minora were enlarged and indurated [Figure 1]. There was no enlargement of regional lymph nodes. The clinical possibilities of Crohn’s disease and lymphogranuloma venereum were considered. On routine laboratory examination, there was no other abnormality except microcytic hypochromic anemia with hemoglobin level 8.5 g/dL. The histopathological examination of the ulcer showed multiple atypical histiocytic cells within the whole thickness of the dermis with positivity for CD1a and CD 207 (Langerin) on immunohistochemistry [Figure 2a-d]. A final diagnosis of LCH was made. The patient was worked up to exclude systemic involvement, including a normal bone marrow biopsy and negative skeletal survey. Computed tomography scan of the chest, abdomen and pelvis revealed nonspecific findings, with no signs of involvement of any other system, leading to a diagnosis of vulvar LCH. The patient was started on oral prednisolone 40 mg daily and methotrexate 15 mg once weekly. The oral steroid was tapered over the- next 2 months and the ulcer healed completely over the next 4 months [Figure 3]. The patient is not having any recurrence or any other systemic symptoms till now.

- Well-defined ulcer with pale granulation tissue in the floor over perineum with vulvar nodules
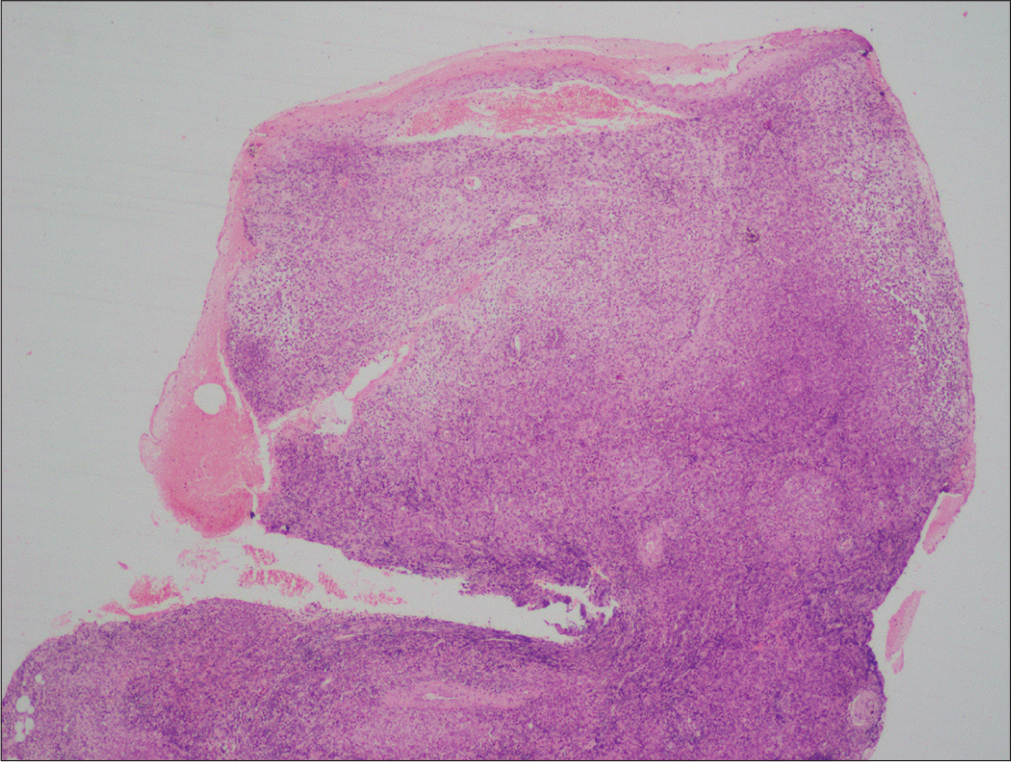
- Scanner view showing variable degree of cellular infiltration in the whole thickness of dermis (H and E, ×20)
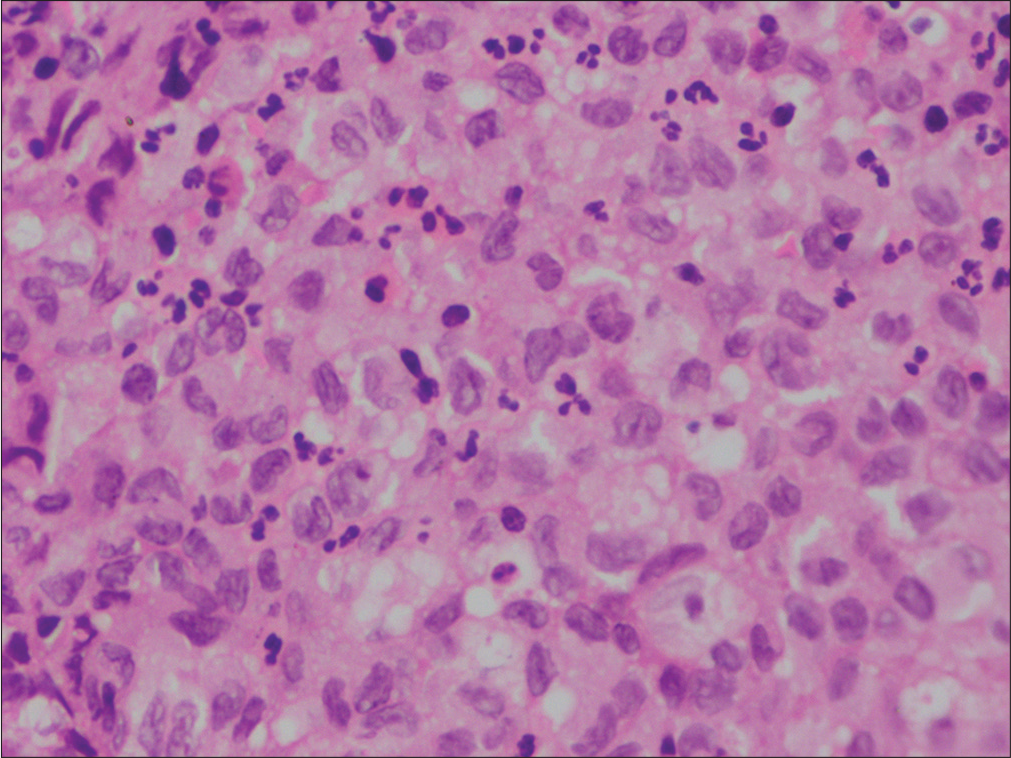
- High-power view showing multiple pale histiocytic cells (containing abundant cytoplasm, reniform nuclei, and prominent nuclear grooving) within the dermis (H and E, ×400).
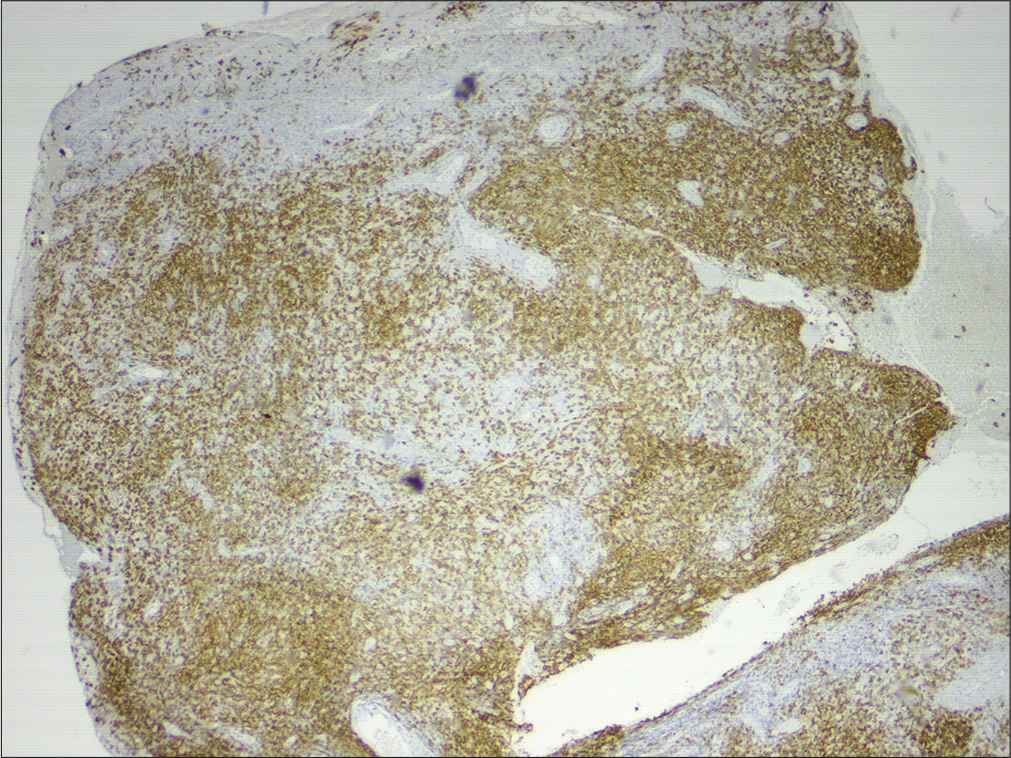
- Histiocytes showing CD1a positivity on immunohistochemistry (40x)
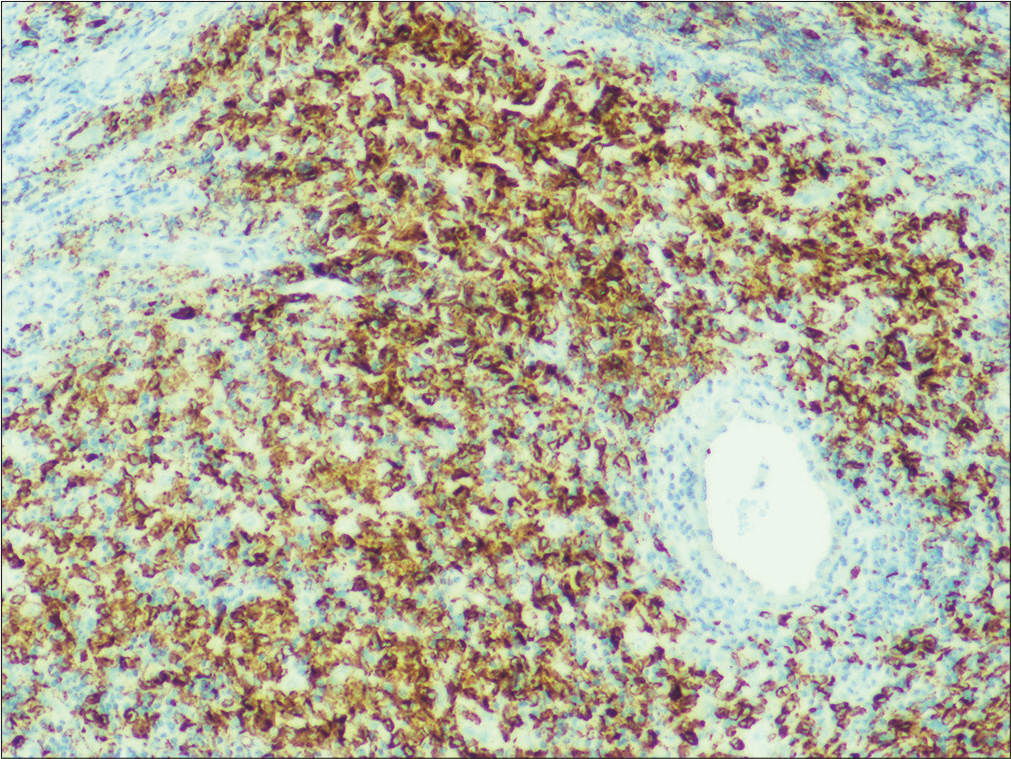
- Histiocytes showing Langerin positivity on immunohistochemistry (100x)

- Complete healing of the ulcer with resolution of the nodules
LCH, previously known as histiocytosis X, includes eosinophilic granuloma, Hand–Schüller–Christian disease and Letterer–Siwe disease, depending on the involved tissues.1 Four patterns of involvement of the female reproductive tract have been identified: (a) pure genital LCH, (b) genital tract LCH with subsequent multiorgan involvement, (c) oral or cutaneous LCH with subsequent genital and multiorgan involvement and (d) diabetes insipidus with organ involvement.1 Sites include the vulva, vagina, cervix, and endometrium, with vulva being the most common site. The lesions may present as an area of induration, pruritic rash, papules, nodules or ulceration, and fissuring.1 Associated involvement of the oral mucosa with gingival nodules or ulceration may be present. In our case, all other mucosa except genital mucosa were unaffected and there was no clinical evidence suggestive of involvement of any other organ system.
Clinical differential diagnoses of genital LCH include Crohn’s disease, vulvar tuberculosis, amoebiasis, and malignancy. Cutaneous Crohn’s disease presents as perianal, peristomal and perifistular ulceration, as well as granulomatous cutaneous inflammation separate from gastrointestinal tract openings (metastatic Crohn’s disease).3 Vulvar tuberculosis may have clinical presentation varying from small superficial ulcers to hypertrophic lesions.4 Amoebiasis cutis presents as a granulomatous ulcer or well-demarcated, intensely tender and painful ulcer with central slough, raised purplish-black undermined margin, outer erythematous zone and purulent exudates usually associated with fever, malaise, and general debility which can lead to death. Demonstration of trophozoites in wet-drop preparations or histological sections from the ulcer is diagnostic.5 Cutaneous malignancy can also present as chronic ulcers.
The diagnosis of LCH is confirmed through histopathology. On hematoxylin and eosin stain, the biopsy classically consists of reniform Langerhans cells associated with an eosinophil-rich inflammatory infiltrate. Diagnosis is confirmed by positive staining for CD1a or CD207 (Langerin) marker.1 S-100 may be positive. Both CD1a and Langerin are transmembrane proteins expressed in normal Langerhans cells as well as cells seen in LCH. Electron microscopy depicting Birbeck granules is no longer essential for the diagnosis. Imaging studies of the head, chest, abdomen and pelvis along with a bone marrow biopsy should be performed to rule out hematogenous spread and involvement of other organs.
There is no consensus till date in the treatment of LCH. Treatment options for vulvar involvement include topical and oral steroids, chemotherapy (vinblastine, vincristine or 2-chlorodeoxyadenosine), immunomodulators (methotrexate or tacrolimus), thalidomide, partial or radical vulvectomy with or without lymph node resection, and radiation therapy.1
The patient had presented with vulvar nodules and nonhealing ulcers on the perineum, which remained undiagnosed for a long time. Mucosal biopsy and immunohistochemistry led to the final diagnosis. Hence dermatologists, gynecologists, and venereologists must consider LCH as a differential diagnosis of chronic, nonhealing nodules, and ulcers on the vulva and perineum.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Langerhans cell histiocytosis limited to the female genital tract: A review of literature with three additional cases. Gynecol Oncol Rep. 2017;22:4-8.
- [CrossRef] [PubMed] [Google Scholar]
- Primary langerhans cell histiocytosis of the vulva in a postmenopausal woman: Response to treatment with oral methotrexate. J Low Genit Tract Dis. 2018;22:169-70.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous manifestations of Crohn's disease. J Am Acad Dermatol. 1981;5:689-95.
- [CrossRef] [Google Scholar]
- Vulvar tuberculosis-a rare manifestation of the disease. Rev Bras Ginecol Obstet. 2019;41:575-8.
- [CrossRef] [PubMed] [Google Scholar]
- Amoebiasis cutis: Clinical suspicion is the key to early diagnosis. Australas J Dermatol. 2010;51:52-5.
- [CrossRef] [PubMed] [Google Scholar]





