Translate this page into:
Late onset localized steatocystoma multiplex of the vulva
2 Department of Dermatology, Chonbuk National University Medical School, Jeonju, South Korea
Correspondence Address:
Seok-Kweon Yun
Department of Dermatology, Chonbuk National University Medical School, 20, Geonji-ro, Deokjin-gu, Jeonju-561712
South Korea
| How to cite this article: Park J, Hwang SR, Kim DW, Kim JI, Yun SK. Late onset localized steatocystoma multiplex of the vulva. Indian J Dermatol Venereol Leprol 2014;80:89-90 |
Sir,
Steatocystoma multiplex is a hamartomatous malformation of the pilosebaceous duct junction, and is often familial with an autosomal dominant inheritance. The lesions typically appear in adolescence or early adulthood; however, steatocystoma multiplex can first develop late in life. Although it is principally located on the upper anterior portion of the trunk, upper arms, and thighs, several reports of localized steatocystoma multiplex limited to the face, scalp, groin, and vulva have been described. [1] This case report describes an 82-year-old woman diagnosed with sporadic steatocystoma multiplex strictly confined to the vulva, the oldest patient and the most late onset known in the literature.
An 82-year-old woman presented to the dermatology outpatient clinic for a slowly growing skin lesion on the vulva of about 6-month duration [Figure - 1]. Physical examination revealed multiple non-tender white to yellow cystic papules and nodules of various sizes on her vulva. She had no family history of skin lesions or nail dystrophy, and the results of routine laboratory testing were within normal limits. A skin biopsy from one of the cysts showed a stratified squamous epithelium with an absent granular layer. Sebaceous glands were located in the cyst wall, and there was a homogeneous, undulating, eosinophilic cuticle on the luminal side wall [Figure - 2]. Based on these pathological and clinical findings, we made the diagnosis of a localized variant of vulvar steatocystoma multiplex.
 |
| Figure 1: Multiple cystic papulonodules of varying sizes on the vulva |
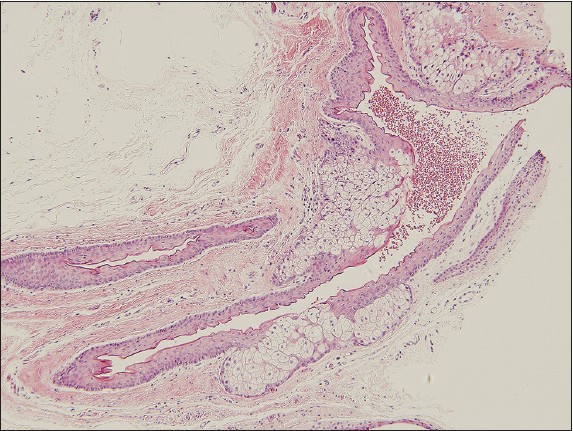 |
| Figure 2: Sebaceous glands located in the cyst wall, and a homogeneous, undulating eosinophilic cuticle seen on the luminal side of the wall (H and E, ×100) |
Although our case demonstrated the characteristic histopathological findings of a steatocystoma, its unusual location and late onset were particularly interesting. In contrast to the typical steatocystoma multiplex seen in patients, the lesions in this case were limited to the vulva. To date, only four cases dealing with vulvar steatocystoma multiplex have been reported in the literature. [2],[3] In 1948, Lewis was the first to describe a 37-year-old woman with multiple sebaceous cysts confined only to the vulva, but histopathological findings were undefined. The case was familial and the lesions were suppurated. [2] The second patient was a 40-year-old woman with the familial form. The patient received surgical treatment to address pain. The remaining two patients were women older than 60 with no family history; of these, one patient did not undergo treatment, and the other was treated with surgical removal of larger lesions. our patient refused treatment. Steatocystoma multiplex can be present at or shortly after birth, especially in familial cases, whereas sporadic forms of steatocystoma multiplex may present as late as 78 years. [4] Our case is the oldest patient and the most late onset of steatocystoma multiplex reported in the literature.
The causative factors of steatocystoma multiplex remain unclear, but trauma, infection, or immunologic events might be responsible. A few authors have reported that steatocystoma multiplex could be associated with many diseases such as ichthyosis, koilonychia, and Jackson-Lawler syndrome (pachyonychia congenita type 2). [5] In our case, there were no associated findings. The clinical differential diagnosis for steatocystoma multiplex includes multiple epidermoid cysts, eruptive vellus hair cyst, neurofibromatosis, lipoma, and xanthomatosis. Biopsy needs to be done to exclude other potential diagnoses.
The lesion of steatocystoma multiplex is cosmetically disconcerting and usually asymptomatic, but may become inflamed and eventually infected. Treatment is difficult, and various medical and surgical therapies have been tested, including anti-inflammatory and antibiotic therapy for infected lesions, radical excision of larger tumors, needle aspiration, dermabrasion, cryotherapy, carbon dioxide laser, and mini incision with drainage and extraction. Isotretinoin has also been tried with varying degrees of success.
| 1. |
Cole LA. Steatocystoma multiplex. Arch Dermatol 1976;112:1437-9.
[Google Scholar]
|
| 2. |
Lewis B. Multiple sebaceous cysts of the vulva. Royal Society of Medicine Section of Dermatology.Br J Dermatol 1948;60:254-5.
[Google Scholar]
|
| 3. |
Rongioletti F, Cattarini G, Romanelli P. Late onset vulvar steatocystoma multiplex. Clin Exp Dermatol 2002;27:445-7.
[Google Scholar]
|
| 4. |
Riedel C, Brinkmeier T, Kutzne H, Plewig G, Frosch PJ. Late onset of a facial variant of steatocystoma multiplex-calretinin as a specific marker of the follicular companion cell layer. J Dtsch Dermatol Ges 2008;6:480-2.
[Google Scholar]
|
| 5. |
Muhammed K, Safia B. Jackson-lawler syndrome. Indian J Dermatol Venereol Leprol 1999;65:242-3.
[Google Scholar]
|
Fulltext Views
7,807
PDF downloads
3,515





