Translate this page into:
Leukemia cutis preceding bone marrow relapse in acute monocytic leukemia
2 Department of Medical Laboratory Techniques, Technical Institute of Halabja, Sulaimani Polytechnic University; Department of Medical Laboratory Sciences, College of Science, Komar University of Science and Technology, Iraq
Correspondence Address:
Najmaddin Khoshnaw
Department of Haematology, Hiwa Hospital, Sulaymaniyah, Kurdistan Region
Iraq
| How to cite this article: Khoshnaw N, Muhammad BA. Leukemia cutis preceding bone marrow relapse in acute monocytic leukemia. Indian J Dermatol Venereol Leprol 2016;82:713-716 |
Sir,
Leukemia cutis is a non-specific term used to describe an extra-medullary manifestation of any type of leukemia characterized by skin infiltration (epidermis, dermis or subcutaneous tissues) with neoplastic leukemic cells resulting in clinically identifiable skin lesions.[1],[2],[3]
A 50-year-old woman presented to the hematology department with a 2-week history of generalized nodular skin lesions along with mild bone pain and fever. The patient had a history of acute monocytic leukemia which was diagnosed 6 months prior to the present admission. She experienced a complete remission which lasted for 5–6 months following an induction course of chemotherapy with cytosine arabinocide and daunorubicin (7 + 3) and three additional consolidation courses of the same protocol (5 + 2).
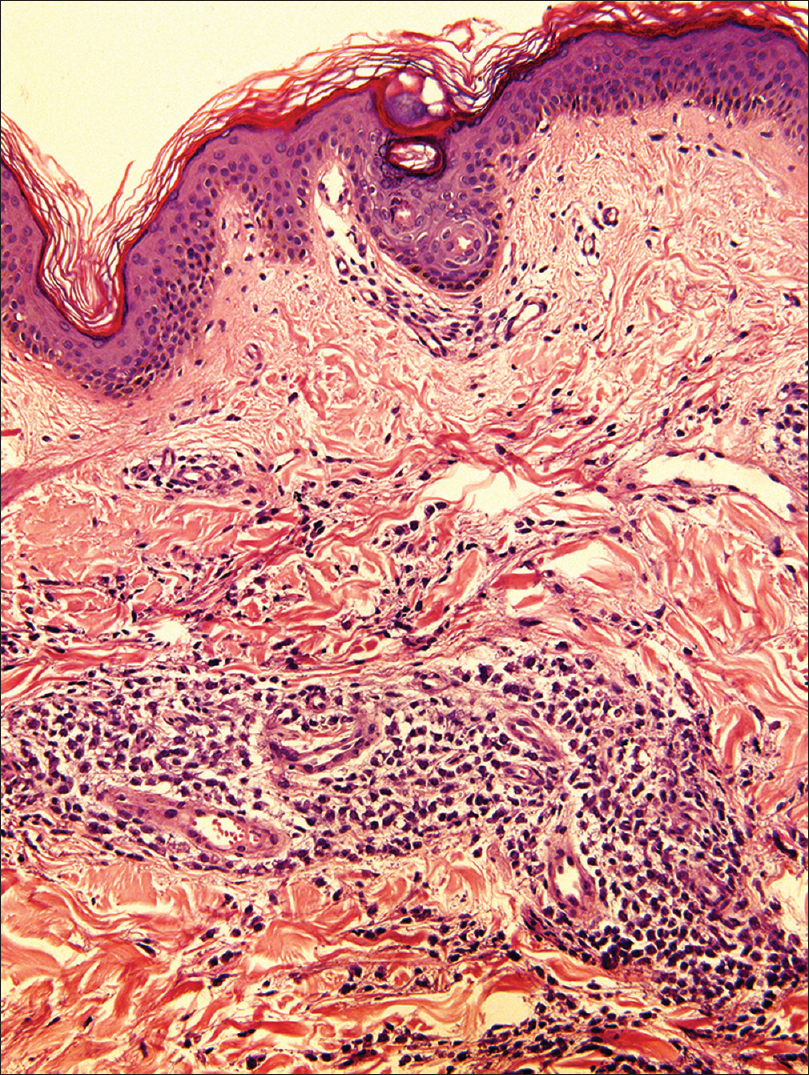
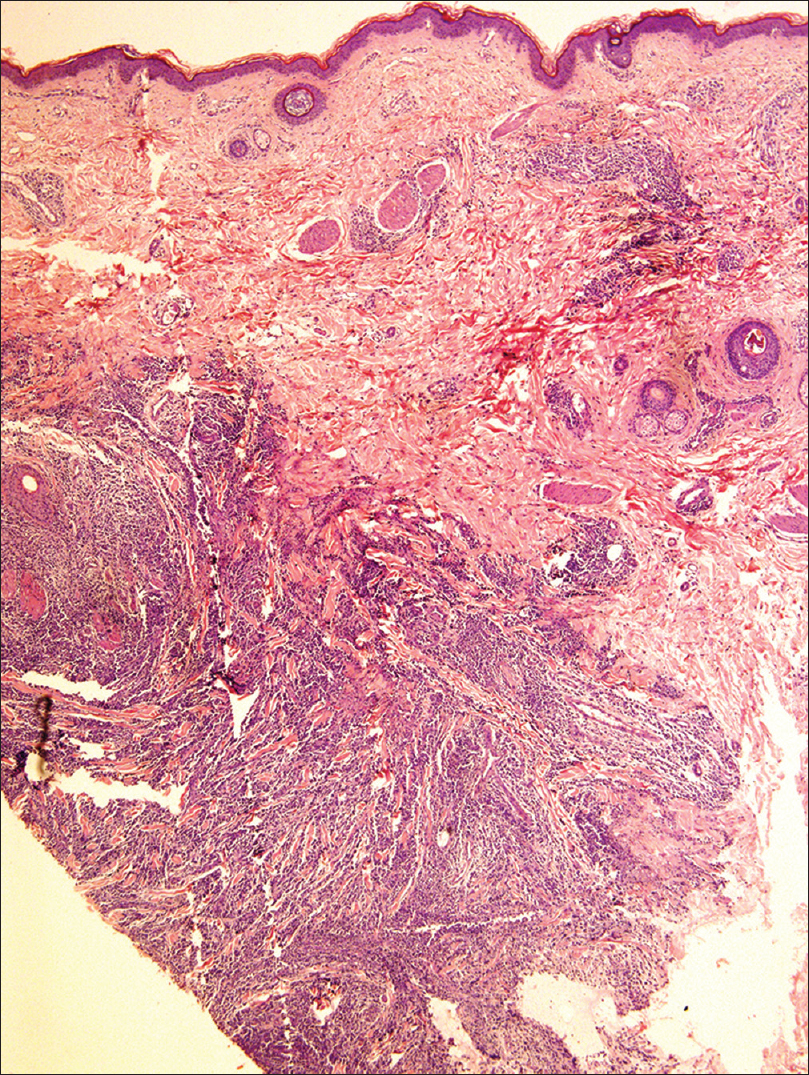
On examination, we found that the skin lesions were of different shapes and sizes ranging from small to large nodules (0.5–3.0 cm in diameter), bullae and erythematous plaques distributed all over the body including the trunk and the ventral aspect of extremities. Tender nodules were felt on the extensor surface of the hands and shin [Figure - 1]a,[Figure - 1]b,[Figure - 1]c,[Figure - 1]d. She also had mild splenomegaly. A biopsy from the largest skin nodule on the upper part of the right leg revealed extensive mononuclear blast cell infiltration in the dermis and the subcutaneous tissue. The blasts had relatively abundant cytoplasm with dispersed chromatin [Figure - 2]a,[Figure - 2]b,[Figure - 2]c. Bone marrow examination at this point revealed 2% blasts and no blasts were detected in the peripheral blood film.
 |
| Figure 1a: Morphological appearance of the skin lesions. Generalized skin lesions, consisting of violaceous subcutaneous nodules, papules, bullae and erythematous lesions on abdomen, per-umbilical |
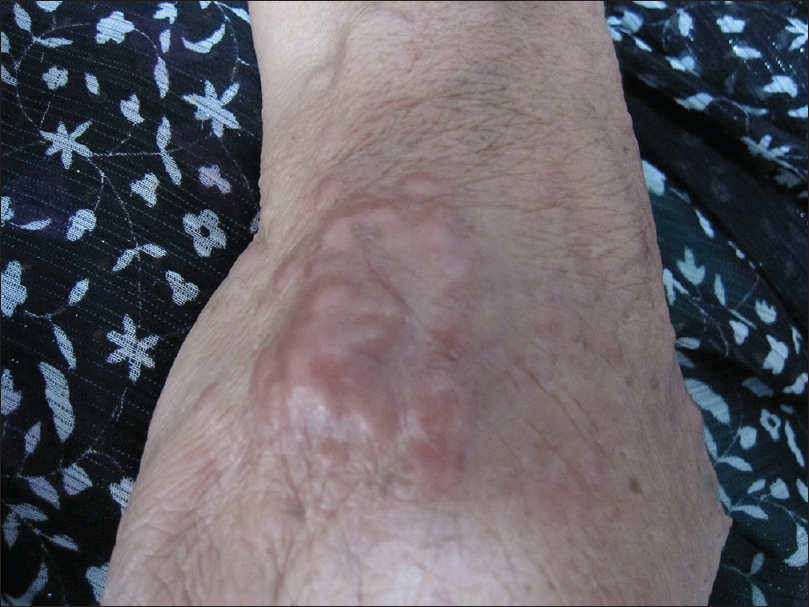 |
| Figure 1b: Morphological appearance of the skin lesions. Generalized skin lesions, consisting of violaceous subcutaneous nodules, papules, bullae and erythematous lesions on extensor surface of the hand showing a large nodule (3 cm × 2 cm). |
 |
| Figure 1c: Morphological appearance of the skin lesions. Generalized skin lesions, consisting of violaceous subcutaneous nodules, papules, bullae and erythematous lesions on lower extremities (plaster indicates the site of the skin biopsy) |
 |
| Figure 1d: Morphological appearance of the skin lesions. Generalized skin lesions, consisting of violaceous subcutaneous nodules, papules, bullae and erythematous lesions on extensor surface of the forearms showing skin lesions |
 |
| Figure 2a: Skin biopsy and bone marrow aspiration. Skin biopsy showing extensive infi ltration of dermis and subcutaneous tissue by mononuclear cells (H and E, ×40) |
 |
| Figure 2b: Skin biopsy and bone marrow aspiration. Skin biopsy showing extensive infi ltration of dermis and subcutaneous tissue by mononuclear cells (H and E, ×200) |
 |
| Figure 2c: Skin biopsy and bone marrow aspiration. Skin biopsy showing extensive infi ltration of dermis and subcutaneous tissue by mononuclear cells (H and E, ×400) |
Three weeks following the appearance of the initial skin lesions, the symptoms gradually worsened and the patient developed severe pain in the bones coupled with high fever, anorexia, night sweats and productive cough with purpura and ecchymosis in the skin. Physical examination revealed gum hypertrophy with mild splenomegaly. Laboratory investigations revealed moderate anemia, leukocytosis and severe thrombocytopenia with an erythrocyte sedimentation rate of 76 mm/h and raised lactate dehydrogenase levels of 564 IU.
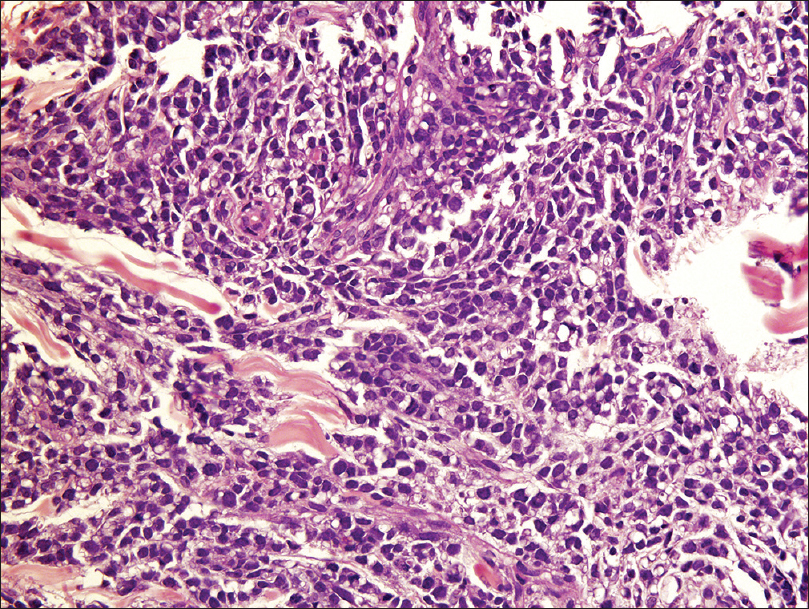
Further investigations revealed obvious signs of relapsed acute monocytic leukemia in both the peripheral blood smear (5% of blasts) and the bone marrow aspirate (32% blasts) [Figure - 2]d. The blast cells were large with abundant moderately basophilic cytoplasm. Although a partial remission was obtained after a course of aggressive chemotherapy with FLAG-IDA (fludarabine 30 mg/m[2], Ara-C 2 g/m[2] for 5 days, idarubicin 10 mg/m[2] for 3 days and granulocyte-colony stimulating factor from day 6 until neutrophil recovery), the patient could not achieve a complete remission. Eventually, she died 35 days after the initial presentation with skin lesions. Death was attributed to complications including severe febrile neutropenia and septicemia.
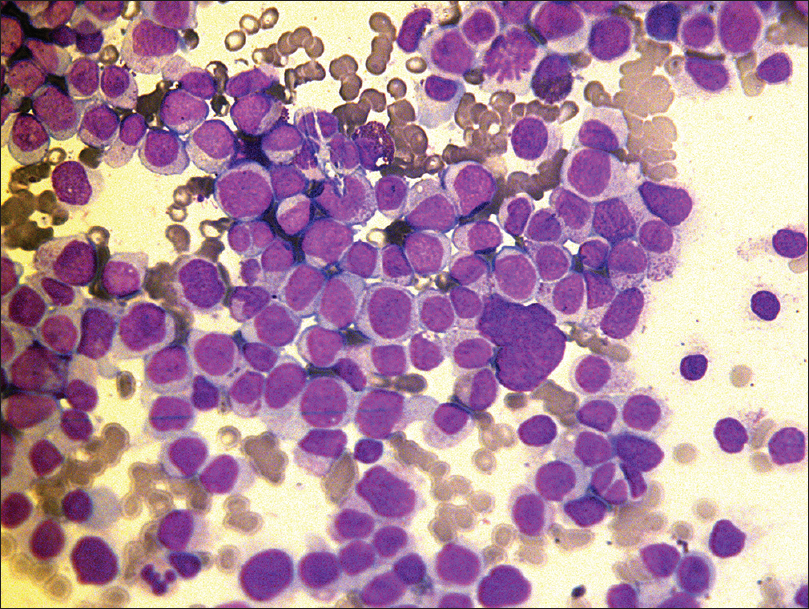 |
| Figure 2d: Skin biopsy and bone marrow aspiration. Bone marrow aspiration showing extensive infiltration by monocytes and monoblasts (Leishman, ×400) |
Leukemia cutis is an extramedullary skin infiltration which usually occurs in leukemias, especially in acute monocytic and myelomonocytic leukemias. It may, sometimes, occur before the appearance of peripheral and/or bone marrow leukemia (called aleukemic leukemia cutis) or it may occur concomitantly with systemic leukemia or after a complete remission. The duration may range from weeks to months or even more.[4] Cases of leukemia cutis are often associated with a bad prognosis.[1],[5],[6] Therefore, once a patient is diagnosed to have leukemia cutis, urgent treatment with aggressive chemotherapy is required. Our patient was treated with FLAG-IDA protocol and had entered a period of pancytopenia and febrile neutropenia but eventually died 35 days after the diagnosis of leukemia cutis.
Isolated extramedullary recurrence of acute non-lymphoblastic leukemias always heralds bone marrow relapse and should be treated with re-induction chemotherapy.[7] The increased risk of extramedullary relapse is presumably related to the higher incidence of extramedullary disease as in FAB (French–American–British classification) M4 and M5 subclasses.[8] However, very rarely, leukemia cutis precedes peripheral or bone marrow leukemia as noted in our case.
To sum up, we describe a case of aleukemic leukemia cutis which preceded the relapse of acute monocytic leukemia occurring after a complete remission, with aggressive symptoms and a very short survival time. Due to its aggressive clinical presentation, we strongly recommend that aleukemic leukemia cutis be carefully sought when patients with a history of leukemia, when develop cutaneous nodules.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Ansell LH, Mehta J, Cotliar J. Recurrent aleukemic leukemia cutis in a patient with pre-B-cell acute lymphoblastic leukemia. J Clin Oncol 2013;31:e353-5.
[Google Scholar]
|
| 2. |
Cho-Vega JH, Medeiros LJ, Prieto VG, Vega F. Leukemia cutis. Am J Clin Pathol 2008;129:130-42.
[Google Scholar]
|
| 3. |
Wagner G, Fenchel K, Back W, Schulz A, Sachse MM. Leukemia cutis – Epidemiology, clinical presentation, and differential diagnoses. J Dtsch Dermatol Ges 2012;10:27-36.
[Google Scholar]
|
| 4. |
Barzilai A, Lyakhovitsky A, Goldberg I, Meytes D, Trau H. Aleukemic monocytic leukemia cutis. Cutis 2002;69:301-4.
[Google Scholar]
|
| 5. |
Kaddu S, Zenahlik P, Beham-Schmid C, Kerl H, Cerroni L. Specific cutaneous infiltrates in patients with myelogenous leukemia: A clinicopathologic study of 26 patients with assessment of diagnostic criteria. J Am Acad Dermatol 1999;40(6 Pt 1):966-78.
[Google Scholar]
|
| 6. |
Su WP. Clinical, histopathologic, and immunohistochemical correlations in leukemia cutis. Semin Dermatol 1994;13:223-30.
[Google Scholar]
|
| 7. |
Byrd JC, Edenfield WJ, Shields DJ, Dawson NA. Extramedullary myeloid cell tumors in acute nonlymphocytic leukemia: A clinical review. J Clin Oncol 1995;13:1800-16.
[Google Scholar]
|
| 8. |
Harris AC, Kitko CL, Couriel DR, Braun TM, Choi SW, Magenau J, et al. Extramedullary relapse of acute myeloid leukemia following allogeneic hematopoietic stem cell transplantation: Incidence, risk factors and outcomes. Haematologica 2013;98:179-84.
[Google Scholar]
|
Fulltext Views
4,308
PDF downloads
1,707





