Translate this page into:
Lichen planus presenting as erythroderma
Correspondence Address:
Lalit K Gupta
A 3, Sai Villa, Opposite Head Post Office, Madhuvan, Udaipur 313 001, Rajasthan
India
| How to cite this article: Gupta LK, Garg A, Khare AK, Mittal A. Lichen planus presenting as erythroderma. Indian J Dermatol Venereol Leprol 2012;78:409 |
Sir,
Erythroderma, first described by Hebra in 1868, is an inflammatory disorder characterized by erythema and scaling involving more than 90% of the body surface. [1] It results from worsening of preexisting skin disease, or may be caused by drugs or underlying neoplasm. In many cases, the cause remains unknown. The onset may be acute or insidious. A gradual onset is the most frequent pattern of evolution, probably because of its relationship to preexisting dermatoses. The prognosis is frequently related to the cause, time of evolution, onset, associated diseases and laboratory findings. Erythrodermic form of lichen planus is an extreme rarity. We herein report a case of erythroderma due to lichen planus.
A 30-year-old man presented with generalized itchy skin lesions of 3 months duration. The lesions first appeared on the forearms and legs and then spread rapidly to involve the trunk, face and other parts of the body in around 2 months. There was no history of any significant medical illness or medication prior to the onset of skin lesions. Cutaneous examination revealed erythroderma [Figure - 1]a and b. A few islands of normal skin were also seen interspersed [Figure - 1]a and b. Multiple discrete as well as confluent, flat-topped violaceous, scaly papules and plaques typical of lichen planus were present over the dorsa of hands [Figure - 1]c. The lips and buccal mucosa showed white lacy plaques [Figure - 2]a. The genitalia showed whitish plaques with erosions on glans and inner prepuce [Figure - 2]b. Hair and nails were normal. Systemic examination did not reveal any abnormality. Routine hematological, biochemical investigations, chest skiagram, urine and stool examination were normal. tests for hepatitis B, hepatitis C and HIV were also negative. Skin biopsy from the dorsa of the right hand showed classical features of lichen planus consisting of orthokeratosis, hypergranulosis, acanthosis with saw-toothed rete ridges and vacuolar degeneration of basal cell layer with pigmentary incontinence. A band-like lymphohistiocytic infiltrate was present in the upper dermis [Figure - 3].
 |
| Figure 1: (a, b) Erythroderma with a few spared areas of normal skin (anterior and posterior view). (c) Classical flat-toped violaceous papules and plaques of lichen planus over the dorsa of the hand |
 |
| Figure 2: (a) White lacy plaques seen on the lips and in the oral cavity. (b) Whitish plaques with erosions on the glans and inner prepuce |
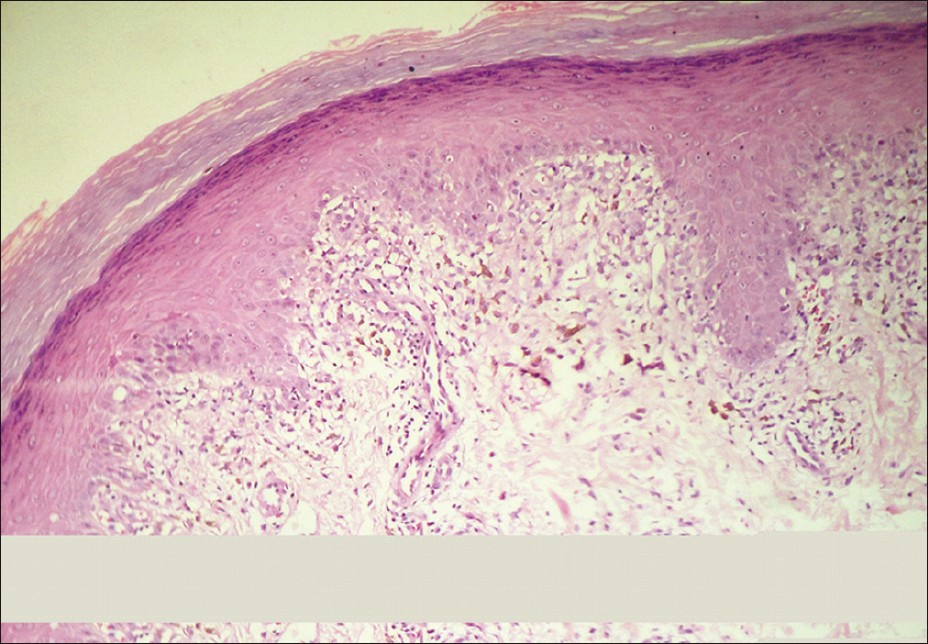 |
| Figure 3: Photomicrograph showing hyperkeratosis, hypergranulosis, vacuolar degeneration of basal cell layer, saw-toothed elongation of rete ridges and a band-like dermal infiltrate (H and E, �40) |
Lichen planus has a worldwide distribution, with the overall prevalence believed to be around 1% of the adult population. [1],[2] It is an idiopathic inflammatory disease of the skin and mucous membranes, characterized by pruritic, violaceous papules that favor the extremities. [1] Various clinical variants of lichen planus includes acute eruptive, hypertrophic, atrophic, bullous, actinic and oral. [1],[2] Although lichen planus has been mentioned in the standard textbooks of dermatology as a cause of erythroderma, [1],[2] one hardly encounters such presentation in clinical practice. A thorough search of published reports on erythroderma and its causes revealed very few cases of lichen planus as a cause of erythroderma. [3],[4],[5] In one of the cases, erythroderma was reported in association with lichen planus pemphigoides. [3] In a case series of 80 cases of erythroderma, [4] only one case of erythroderma due to lichen planus was reported. Another case has recently been described [5] in a 71-year-old male who, in addition to the papular lesions, also had bullous lesions and erosions. There was a history of intake of angiotension receptor blocker for hypertension. Histology in this case showed eosinophils. A possibility of lichenoid drug eruptions in this case is therefore difficult to rule out.
Our case had classical lesions of lichen planus with mucosal lesions. There were no bullous lesions and history of drug intake prior to the onset of disease. The index case represents a classic case of lichen planus presenting as erythroderma. The rarity of lichen planus as a cause of erythroderma has prompted us to report this case. Although unusual, lichen planus may be considered as a cause of erythroderma.
| 1. |
Sterry W, Assaf C. Erythroderma. In: Bolgonia JL, Jorizzo JL, Rapini RP, editors. Dermatology. 2 nd ed. Spain: Mosby Elsevier; 2008. p. 149-58.
[Google Scholar]
|
| 2. |
Holden CA, Berth-Jones J. Eczema, lichenification, prurigo and erythroderma. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 7 th ed. Oxford: Blackwell Scientific Publications; 2004. p. 17.48-17.52.
th ed. Oxford: Blackwell Scientific Publications; 2004. p. 17.48-17.52.'>[Google Scholar]
|
| 3. |
Campos-Domínguez M, Silvente C, de la Cueva P, González0-Carrascosa M, Lecona M, Suárez R, et al. Erythrodermic lichen planus pemphigoides. Actas Dermosifiliogr 2006;97:583-6. (Spanish)
[Google Scholar]
|
| 4. |
Rym BM, Mourad M, Bechir Z, Dalendo E, Faika C, Ladh AM, et al. Erythroderma in adults: A report of 80 cases. Int J Dermatol 2005;44:731-5.
[Google Scholar]
|
| 5. |
Rose AE, Patel U, Chu J, Patel R, Meehan S, Latkowski JA. Erythrodermic lichen planus. Dermatol Online J 2011;17:26.
[Google Scholar]
|
Fulltext Views
3,049
PDF downloads
3,557





